Ultrasound Guided Subclavian Line Pearls
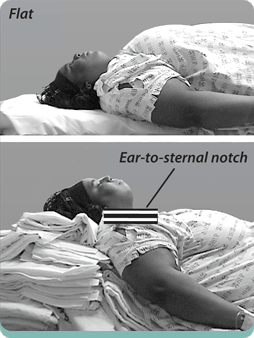
/Subclavian central lines have historically been a landmark based procedure. While for years IJ and femoral central venous access had move to being primarily ultrasound guided (or entirely ultrasound guided), the subclavian line was a long standing holdout. As such, providers may be unfamiliar with some of the pearls that can facilitate performance of the procedure with ultrasound. In this post, Dr. Ben Duncan, ultrasound fellow discusses some of the ways to help make ultrasound work for you while trying to perform a subclavian line.
Read More