Background
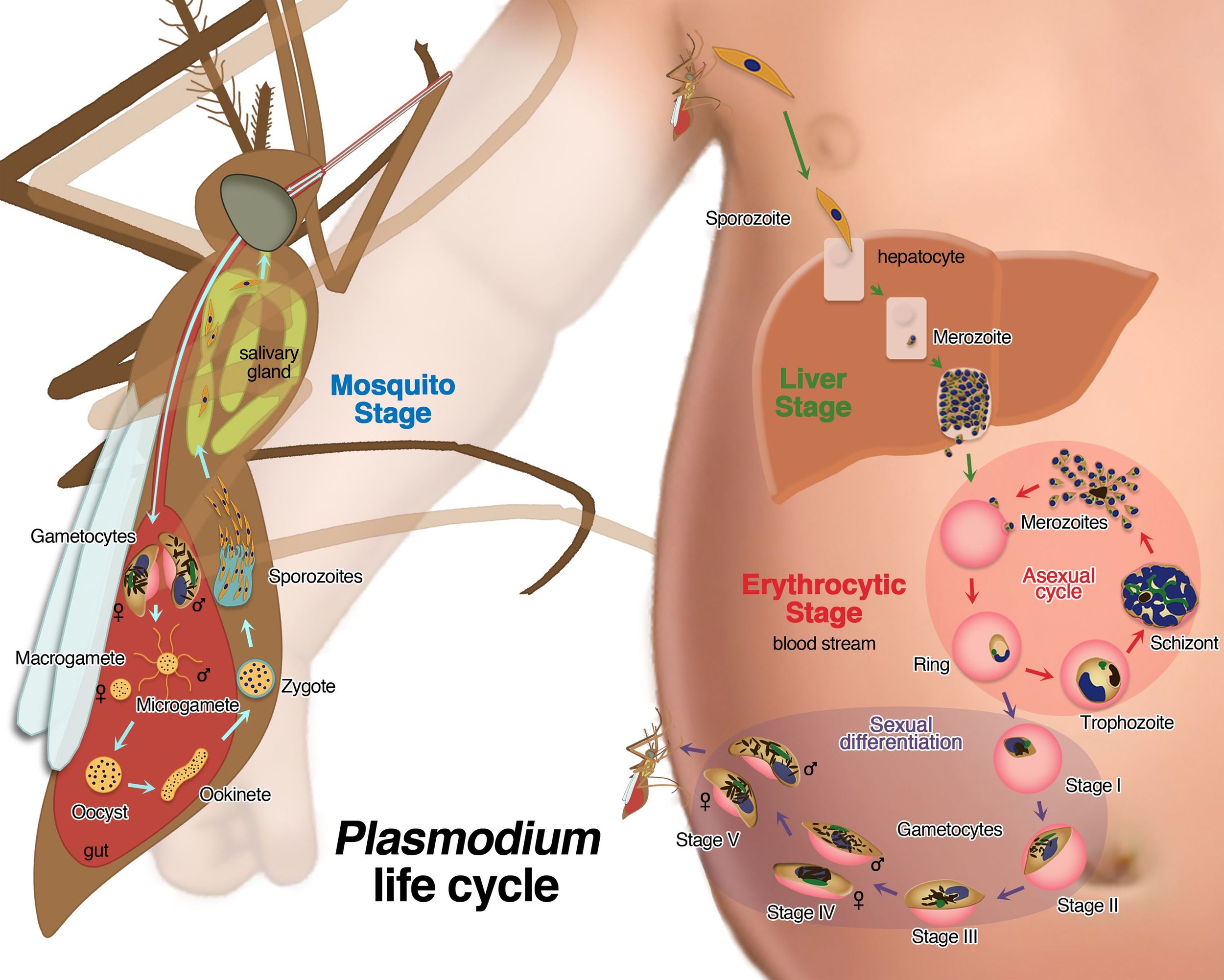
Malaria is a mosquito-borne infectious disease commonly transmitted via a bite from an infected female Anopheles mosquito. The disease is widespread in tropical regions surrounding the equator. There are five species of Plasmodium and the vast majorities of deaths are caused by P. falciparum. There were 198 million documented cases of malaria in 2013 and as many as 1.2 million people died (WHO). Most deaths occur in children under the age of 5, and it is estimated that a child dies of malaria every 30 seconds. Other high risk groups include pregnant women and non-immune travelers. Malaria is commonly associated with poverty and is a potential barrier to economic growth, accounting for nearly 40% of public health expenditure in Africa.
Clinical Presentation
Signs/symptoms of malaria typically begin 8-25 days following infection. Patients often initially develop flu-like symptoms. Presentation may include fever (often cyclical), headache, rigors, arthralgias, nausea/vomiting. Findings include hemolytic anemia (sometimes severe), splenomegaly, jaundice, hemoglobinuria (aka “Blackwater Fever with renal failure), and jaundice. Cerebral malaria is defined as severe P. falciparum-malaria presenting with neurologic symptoms, including coma or seizure, and is often fatal. Severe malaria can progress rapidly and mortality is as high as 20% despite aggressive management.
Diagnosis
There are no pathognomonic clinical signs or symptoms for the diagnosis of malaria. The gold standard is visualization of parasites in stained samples—3 sets of Giemsa thick & thin blood smears. In resource-limited settings (such as Shirati), Rapid diagnostic tests (RDTs), detecting antigens or antibodies, are more common and very useful.
Treatment
Most effective treatment is with use of artemisinins in combination with other antimalarials (amodiaquine, lumefantrine, mefloquine, or sulfadoxine/pyrimethamine). We commonly used artemisinin-lumefantrine (Coartem) for outpatient treatment in Tanzania. For severe cases and inpatient management we used IV quinine therapy as well.
Prophylaxis
Multiple regimens including chloroquine (extensive resistance), mefloquine, doxycycline, and Malarone (atovaquone-proguanil HCl) can be used.
Shirati clinical Case
13 year old-male with no significant medical history presents with 3 days of fever, cough, chest pain, and intermittent nose bleeds. He denies nausea, vomiting, diarrhea, or abdominal pain. His cough is non-productive and he has had no sick contacts.
T 39.1C HR 98 BP 110/70 RR 16 weight 40kg
Generally he is a mildly ill-appearing with skin that is warm to touch. He has mild conjunctival pallor with a clear oropharynx without erythema or lesions. Cardiovascular exam with S1 S2 present, borderline tachycardia, regular rhythm, no murmurs. He has no respiratory distress with good air movement and diffuse mild expiratory wheezing. His abdomen is soft, nontender and nondistended. He has palpable splenomegaly with the lower spleen edge palpated 2-3 finger-breadths below the left costal margin. He has wam skin without edema or rash.
Article by Anand Selvam, MD
References:
- World Malaria Report. 2015
- White NJ, Pukrittayakamee S, Hien TT, et al. Malaria. The Lancet 2014; 723-735.
- Agarwal A, McMorrow M, Onyango P, et al. A randomized trial of artemether-lumefantrine and dihydroartemisinin-piperaquine in the treatment of uncomplicated malaria among children in western Kenya. Malaria Journal 2013; 12:254.
- Rosenthal PJ. Artesunate for the Treatment of Severe Falciparum Malaria. N Engl J Med. 2008; 388:1829-36.
- Breman, JG. Conquering Malaria. Improving Population Health Workshop. Fogarty International Center. Cuernavaca, Mexico. 2003.
- Trampuz A, Jereb M, Muzlovic I, et al. Clinical Review: Severe Malaria. Critical Care. 2003, 7:315-323.