The Return of Droperidol...
/What are the big takeaways from this post?
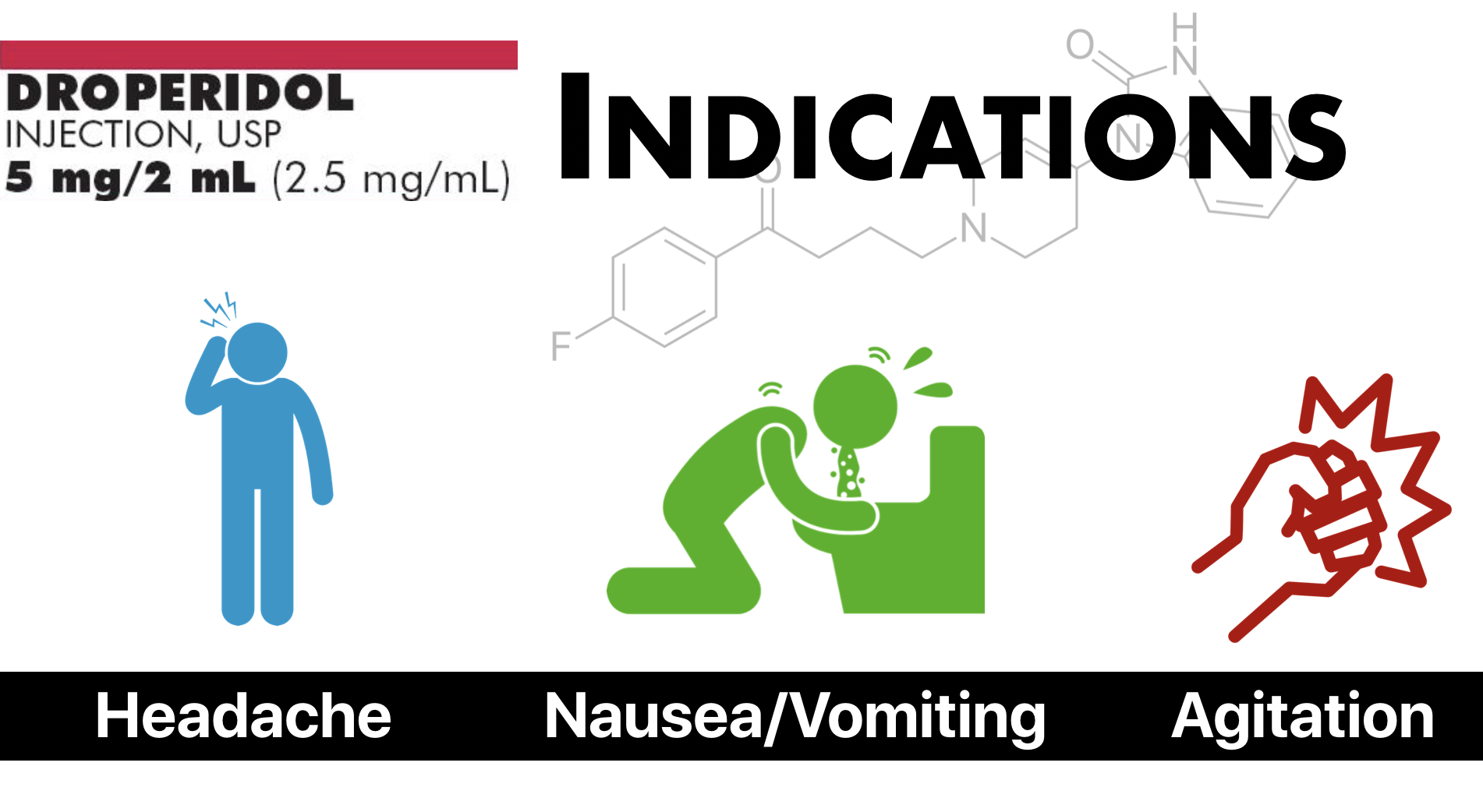
Droperidol has evidence for efficacy in the treatment of nausea and vomiting, benign headache and migraine, and for the control of acute agitation in the Emergency Department. Its main side effects are sedation, extrapyramidal effects (primarily akathisia), hypotension (especially orthostatic), and prolongation of the QT interval (dose dependent). A black box warning for torsade de pointes was issued in 2001 for IVP doses >2.5 mg.
What is this Drug, Is it Safe and Why Did it Go Away?
Droperidol is a butyrophenone with primarily dopaminergic action as a D2 receptor antagonist. (1) It has a number of uses for ED patients (which will be detailed more below) including treatment of nausea and vomiting, migraine, and acute agitation. The side effects of droperidol include extrapyramidal effects (akathisia and dystonia), sedation, hypotension (through mild alpha adrenergic blockade and peripheral vascular dilation), and QTc prolongation. In 2001, the FDA issued a black box warning due to concerns about QT prolongation and torsade de pointes. The recommended ECG telemetry monitoring for 2-3 hours after administration of droperidol, that an ECG be performed on all patients prior to receiving droperidol, and that droperidol should NOT be administered to patients with QTc >440 msec for males and >450 msec for females. (2) Notably the black box warning applies only for the dosages of droperidol as indicated in the package insert (2.5 mg and higher). Lower doses are commonly used in the ED setting (0.625 to 1.25 mg are typical doses for nausea, vomiting, and migraine).
The FDA’s black box warning has drawn significant comment and controversy in the medical literature. (1, 3, 4, 5) The black box warning was based on 273 case reports recorded over a 4 year period of time. It is important to note, in the majority of 89 deaths reported in the 273 case reports doses of droperidol ranged from 25 to 250 mg (4, 6) Adverse cardiac events or death occurred in 10 patients who had received doses less than 2.5 mg. A review of those cases by Habib and colleagues however found that all cases had confounding factors that could have also accounted for the noted adverse reactions. (6) Those who argue against the FDAs black box warning, refer to a number of randomized clinical trials where droperidol was used in doses less than 2.5 mg and where no significant increased risk of cardiac events were reported (4). Those who argue (somewhat) in support of the black box warning, note that there is a dose and time dependent relationship between the administration of droperidol and prolongation of the QTc interval. (3) For its part, the FDA has not revised their black box warning but did clarify that the black box warning does not apply for doses less than 2.5 mg and that they do not have data to make any determination for the safety or lack of safety of droperidol at doses less than 2.5 mg (5).
The black box warning does identify patients in which to administer droperidol with extreme caution, as they may be at increased risk for development of prolonged QT syndrome. Such patient populations include: congested heart failure, bradycardia, use of a diuretic, cardiac hypertrophy, hypokalemia, hypomagnesemia, or administration of other drugs known to increase the QT interval. Other risk factors for increased QTc include age greater than 65 years, alcohol abuse, and use of agents such as benzodiazepines, volatile anesthetics, and IV opiates. It would be prudent to initiate droperidol at a lower dose and titrate up as needed to reach desired effect in these patient populations.
What are the potential uses for droperidol in the ED?
Nausea and Vomiting
Furyk and colleagues (7) conducted a Cochrane Review looking at the safety and efficacy of anti-emetic medications in the Emergency Department, including 8 randomized control trials with a total of 952 patients. The included trials examined a number of anti-emetic medications. In comparison to placebo, droperidol was the only medication to result in a significant change in a nausea visual analog scale (VAS) at 30 minutes. Comparing droperidol to active control (i.e. other anti-emetics), there was no evidence that droperidol was more effective than metoclopramideor prochlorperazine. It should be noted that the data for this part of the Cochrane Review came from a single study by Bruade and colleagues (8). The authors in this study did note a significantly higher incidence of self-reported akathisia at 24 hr follow-up for droperidol vs all other agents (71.4% vs 23.5%).
Migraine/Headache
A systematic review by Thomas and colleagues (9) looked at the efficacy of droperidol for the treatment of migraine and acute headache. Droperidol showed improved pain relief as measured by VAS when compared to placebo (1 study), prochlorperazine (2 studies), and meperidine (1 study). The 2 most interesting studies in this article were the studies comparing droperidol to prochlorperazine. Miner et al (10) enrolled a convenience sample of 168 patients, randomizing them to either receive droperidol (5 mg IM or 2.5 mg IV) or prochlorperazine (10 mg IM or IV). Baseline characteristics were similar between groups. Droperidol was more effective as judged by VAS at 30 and 60 min but rates of rescue medication use were similar in both groups. Incidence of akathisia was 6.1% in the droperidol group and 8.1% in the prochlorperazine group. There were no reports of adverse cardiac events. The second of these 2 studies of interest was by Weaver and colleagues (11). It was a prospective, randomized controlled trial comparing droperidol 2.5 mg IV to prochloperazine 10 mg IV for patients presenting with headache and a normal neurologic exam. The trial was stopped early because of the FDAs black box warning which was released mid-study. The investgators had initially sought to enroll 230 patients per group based on their power analysis, but only ended up enrolling 48 patients in each group. They did find that a higher proportion of patients in the droperidol group had a >50% reduction in pain scores at 30 min as compared to prochlorperazine (83.3% vs 72.3%) with similar rates of akathisia in each group.
Acute Agitation
Chan and colleagues (12) conducted a multi-center, randomized, double-blind, controlled trial evaluating a control (midazolam), droperidol (5 mg IV), and olanzapine (5 mg IV). Patients were included if they were determined to be acutely agitated requiring ‘sedative containment’ by the treating physician. The primary outcome of the study was time to achieve adequate sedation and proportion of patients sedated at 5 and 10 minutes. 336 patients were enrolled and randomized to the 3 groups. Baseline characteristics were well matched and protocol violations were similar across all three groups. Droperidol and olanzapine performed similarly well against the midazlolam only group. Median time to sedation was 6 min for droperidol and 5 min for olanzapine compared to 10 min for midazlolam. Need for additional sedating medications was lower in the droperidol group (12.5%) as compared to the olanzapine group (18.4%). There were no arrhythmias reported in the droperidol group. One patient in the olanzapine group had an arrhythmia.
Gottlieb and Schiebout (13) conducted a systematic review of the literature looking at the efficacy of droperidol for acute psychosis-induced agitation. They identified 6 trials which met their inclusion criteria, 3 of which were conducted in the ED setting. In the studies, a higher proportion of patients that received droperidol were sedated within 30 minutes as compared to placebo but no difference was found in time to sedation when compared with haloperidol, midazlolam, or olanzapine. There were no reports of increased cardiac or respiratory events in the droperidol groups of the included trials.
References
Perkins J, Ho JD, Vilke GM, DeMers G.American Academy of Emergency Medicine Position Statement: Safety of Droperidol Use in the Emergency Department. JEM 2015;49(1):91–7.
Droperidol Drug Insert. http://labeling.pfizer.com/ShowLabeling.aspx?id=4412Accessed 4/11/2019.
Habib AS, Gan TJ.PRO: The Food and Drug Administration Black Box Warning on Droperidol Is Not Justified. Anesthesia & Analgesia 2008;106(5):1414–7.
Ludwin DB, Shafer SL.CON: The Black Box Warning on Droperidol Should Not Be Removed (But Should Be Clarified!). Anesthesia & Analgesia 2008;106(5):1418–20.
Rappaport BA.FDA Response to Droperidol Black Box Warning Editorials. Anesthesia & Analgesia 2008;106(5):1585–1.
Habib AS, Gan T. Food and Drug Administration Black Box Warning on the Perioperative Use of Droperidol: A Review of the Cases. Anesthesia & Analgesia 2003;:1377–9.
Furyk JS, Meek RA, Egerton-Warburton D. Drugs for the treatment of nausea and vomiting in adults in the emergency department setting. Cochrane Database of Systematic Reviews 2015;29(3):247–53.
Braude D, Soliz T, Crandall C, Hendey G, Andrews J, Weichenthal L. Antiemetics in the ED: a randomized controlled trial comparing 3 common agents. The American Journal of Emergency Medicine 2006;24(2):177–82.
Thomas MC, Musselman ME, Shewmaker J. Droperidol for the Treatment of Acute Migraine Headaches. Annals of Pharmacotherapy 2015;49(2):233–40.
Miner J, Fish S, Smith S, Biros M. Droperidol vs. Prochlorperazine for Benign Headaches in the Emergency Department. Academic Emergency Medicine 2001;8(9):873–9.
Weaver CS, Jones JB, Chisholm CD, et al. Droperidol vs. prochlorperazine for the treatment of acute headache. The Journal of Emergency Medicine 2004;26(2):145–50.
Chan EW, Taylor DM, Knott JC, Phillips GA, Castle DJ, Kong DCM. Intravenous Droperidol or Olanzapine as an Adjunct to Midazolam for the Acutely Agitated Patient: A Multicenter, Randomized, Double-Blind, Placebo-Controlled Clinical Trial. Annals of Emergency Medicine 2013;61(1):72–81.
Gottlieb M, Schiebout J. What Is the Efficacy of Droperidol for the Management of Acute Psychosis-Induced Agitation? Annals of Emergency Medicine 2018;71(1):141–3.