Needle Thoracostomy
/There has been much digital ink spilled over the topic of needle thoracostomy (check below for some additional reading) with most of the hub bub surrounding the proper location to place the needle. We’re not going to completely rehash that which has already been said, but instead focus on distilling the highlights and turning our attention to a video showing how to perform what is ultimately a potentially life saving procedure. We won’t go much into finger thoracostomy as we will cover that procedure in a future blog post. So I heard that you’re setting yourself up for failure if you choose the 2nd ICS MCL to decompress the chest?
Hold your horses there cowboy… The literature looking at the proper location to perform a needle decompression is not exactly settled. The classic teaching of this procedure (as from ATLS) is that a large bore needle (14 G or greater) should be placed in the 2nd ICS in the mid clavicular line. The dogma of this teaching was thrown a bit off kilter in the past several years based on several different studies. In 2010, Micheal Blaivas reported findings in the Journal of Ultrasound Medicine, that 26% of patients that had received prehospital anterior needle thoracostomy had no evidence of pneumothorax. Then, in 2011, Inaba, et al released a study showing that in a cadaveric module, there was a significantly higher rate of failure with the 2nd ICS MCL site as opposed to the 5th ICS anterior axillary line. As summed up by the folks over at EMLyceum, “The reasons for these differing measurements and results are not immediately clear.” There have been several other studies (outlined in the EMLyceum post) that have shown, based on CT imaging, that the 2nd ICS MCL would have a lower overall failure rate than the 4th or 5th ICS.
What’s the take away from this?
Failure is always a possibility.
Look at your patient. If he/she seems to have a significant amount of anterior chest soft tissue, consider the lateral approach. If there’s a significant amount of lateral chest soft tissue, consider an anterior approach.
Whichever approach you use, look closely for your patient’s response. If the tension physiology is not reversed or only transiently reversed, consider trying the other site or going on to do a finger thoracostomy.
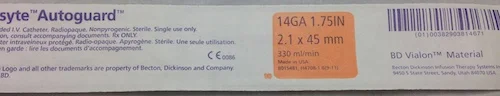
Lets take a look at our tools
14 G IV - note the length 1.75 in, that's 45 mm or 4.5 cm for the metric folks out there
10 G IV - note the length here 3 in, or 76 mm, 7.6cm for the metric folks. This should be more than enough to get into the thoracic cavity of most every patient. Not that it should play into your decision, but, these puppies are pricey (about $20 per based on prices online)
Lets take a look at the procedure itself
References/Further Reading
- EM Lyceum - Pneumothorax Answers
- Blaivis, M. (2010) Inadequate Needle Thoracostomy Rate in the Prehospital Setting for Presumed Pneumothorax. Journal of Ultrasound Medicine. 29. 1285-1289.
- Inaba, K., Branco, B., Eckstein, M., Shatz, D., Martin, M., Green, D., Noguchi, T., & Demetriades, D. (2011) Optimal Positioning for Emergent Needle Thoracostomy: A cadaver-based study. Journal of Trauma. 71 (5) 1099-1103. doi: 10.1097/TA.0b013e31822d9618
- The Trauma Professionals Blog - Needle Thoracostomy: Where to Put it?
- Auckland HEMS - Have we been taught all wrong?... A New Location of Needle Decompression?