Air Care Series: Sepsis Update
/Introduction:
Sepsis is fundamentally a systemic response to infection that results in organ dysfunction, however it is characterized by complex underlying pathophysiology and represents a broad spectrum of disease. Reflecting this, the clinical criteria that define sepsis continue to evolve.
Sepsis was formally defined in a 1992 consensus statement by the ACCP/SCCM as the systemic inflammatory response syndrome (SIRS) in the setting of infection. Recognizing the continuum of disease severity this encompassed, severe sepsis and septic shock were defined as nested subsets of sepsis. (1) The SEP-1 definitions, released by the Centers for Medicare and Medicaid Services (2) in 2015 as a component of the core measure for care of patients with sepsis, adhere to this same framework. Per CMS, sepsis is defined as ≥2 SIRS criteria in the setting of known or suspected infection. Severe sepsis is considered sepsis plus evidence of organ dysfunction, including lactate >2 mmol/L or hypotension, defined as SBP <90 mmHg, MAP <65 mmHg, or a decrease in SBP ≥40 mmHg from a previously documented baseline. Septic shock is defined as sepsis plus an initial lactate >4 mmol/L or hypotension persisting after a 30 mL/kg fluid bolus.
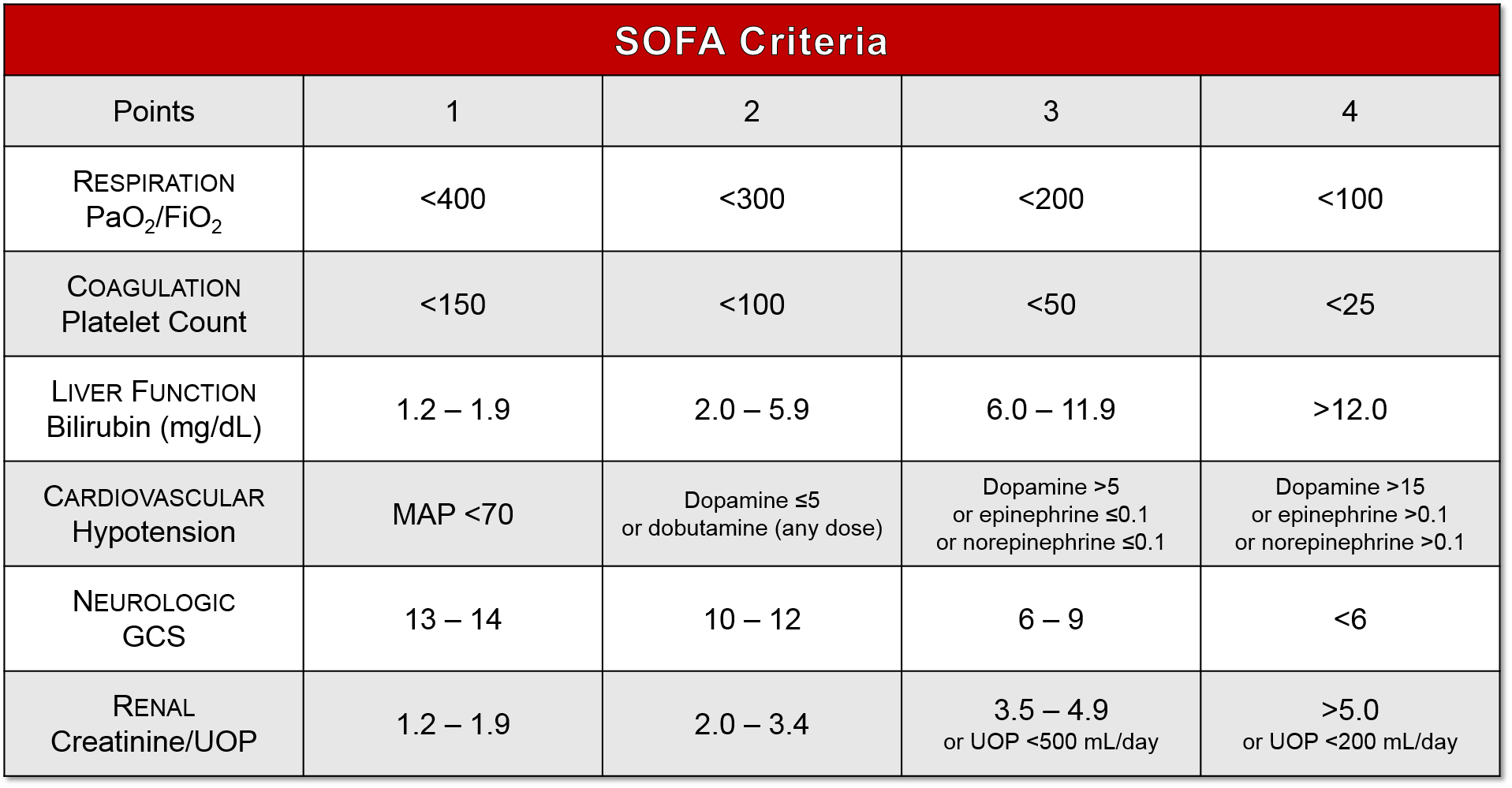
More recently, the Sepsis-3 task force proposed revised definitions for sepsis and septic shock, eliminating the severe sepsis classification and incorporating the Sequential Organ Failure Assessment (SOFA) score (3) as an alternative to the SIRS criteria. Per Sepsis-3, sepsis is defined as a dysregulated immune response producing life-threating organ dysfunction, quantified by an acute increase in SOFA score of 2 or more points. Septic shock refers to sepsis accompanied by profound circulatory, cellular, and metabolic derangements associated with increased mortality relative to sepsis alone, clinically identified by serum lactate >2 mmol/L and persistent hypotension despite adequate fluid resuscitation, requiring vasopressor support to maintain a MAP ≥65. (4)
The management of sepsis and septic shock hinges on early identification of at-risk patients and rapid initiation of therapy. While the SIRS criteria have long served as the primary screening tool for sepsis, the Sepsis-3 task force proposed a bedside assessment tool, qSOFA, to identify patients at risk for poor outcomes in the setting of suspected infection. (4) A systematic review and meta-analysis comparing their prognostic performance found positive qSOFA scores had a sensitivity of 0.51 and specificity of 0.83 for predicting in-hospital mortality in patients with suspected infection, versus a sensitivity of 0.86 and specificity of 0.29 for positive SIRS criteria. Discrimination for in-hospital mortality was similar between positive qSOFA scores and SIRS criteria (AUC 0.74 vs. 0.71, p = 0.816). (5)
Once sepsis or septic shock is suspected in a patient, the immediate management priorities are ensuring airway patency, providing supplemental oxygen and respiratory support as appropriate, and establishing vascular access for prompt administration of fluids, antibiotics, and vasopressors if needed.
Early Goal-Directed Therapy:
Restoring adequate tissue perfusion through fluid resuscitation, and potentially vasopressor use, is essential to reversing the organ dysfunction characteristic of sepsis and septic shock. In a landmark 2001 study, Rivers et al. demonstrated that early, aggressive resuscitation of emergency department patients with severe sepsis or septic shock led to a marked reduction in all-cause mortality. (6) The study utilized protocol-driven administration of crystalloids, vasopressors, inotropes, and blood products to target quantitative hemodynamic endpoints, such as CVP and ScvO2, in an approach termed early goal-directed therapy (EGDT). The Rivers trial revolutionized care of sepsis patients in the emergency department, and heavily influenced previous iterations of the Surviving Sepsis guidelines. In the last five years, however, three large, multi-center randomized controlled trials (ProCESS, ARISE, and ProMISe) demonstrated no mortality benefit to EGDT-driven resuscitation of patients with septic shock relative to a less aggressive protocol-based approach or to so-called usual care, while acknowledging that the usual care of patients with septic shock has evolved considerably since 2001. (7,8,9)
The ProCESS trial enrolled 1341 patients identified as having septic shock in 31 emergency departments in the United States. Patients were randomized to three groups for a six-hour period of resuscitation: protocol-based EGDT as described in the study by Rivers, et al.; protocol-based standard therapy with no requirement for CVC placement, inotropes, or blood products; or usual care. There was no significant difference in mortality between treatment arms at either 90 days or one year. (7) The ARISE trial enrolled 1600 patients presenting to 51 emergency departments, primarily in Australia and New Zealand, with early septic shock. Patients were randomized to either EGDT or usual care for an initial six-hour treatment period, with no difference in 90-day all-cause mortality between the two groups. (8) The ProMISe trial enrolled 1260 patients with septic shock from 56 emergency departments across England, randomized to receive care per a 6-hour EGDT protocol or usual care. At 90 days, there was no significant difference in all-cause mortality. (9) Two subsequent meta-analyses – a prospectively-designed analysis of individual patient data from all three trials (10) and a systematic review and meta-analysis including 11 studies and conducted by the same investigators (11) – similarly found no mortality benefit with EGDT relative to usual care. On the basis of these studies, the 2016 Surviving Sepsis guidelines no longer recommend EGDT for the management of patients presenting with septic shock, instead stressing ongoing reassessment of hemodynamic status and clinical response to therapy as guides for resuscitation efforts.
Volume resuscitation:
The recommended initial fluid volume for resuscitation of patients with suspected septic shock is at least 30 mL/kg IV crystalloids administered within the first 3 hours of treatment, with the need for additional fluids dictated by clinical exam and evidence of fluid responsiveness. In the absence of high-quality data to support a specific volume recommendation, the figure of 30 mL/kg was chosen to reflect the usual care of patients with septic shock, and was the approximate volume of fluid given in the control arms of the ProCESS and ARISE trials. (12)
Red Blood Cell Transfusion:
Additionally, there is no recommendation for routine transfusion of RBCs in patients with sepsis or septic shock and hemoglobin levels ≥7.0 g/dL, though there may be specific clinical situations (e.g. concurrent major hemorrhage, profound hypoxemia) in which transfusions are warranted. (Rhodes 2017) This recommendation is based in large part on the results of a 2014 study which found no difference in 90-day mortality between ICU patients with septic shock who received RBC transfusions for hemoglobin ≤9 g/dL versus ≤7 g/dL. (13)
Vasopressors:
If volume resuscitation alone is not sufficient, vasopressors are recommended to achieve a target MAP of 65 mm Hg, with norepinephrine considered the first-line agent. (12) A 2015 systematic review and meta-analysis found norepinephrine was associated with an all-cause mortality benefit relative to dopamine in the treatment of adults with septic shock, as well as lower risk of major adverse events and cardiac dysrhythmias. (14) The same study identified a trend towards mortality benefit with norepinephrine relative to epinephrine, vasopressin/terlipressin, and phenylephrine, but the results did not reach statistical significance. In the absence of compelling data to support the use of an alternative agent, however, norepinephrine remains the initial vasopressor of choice. Vasopressin and epinephrine are recommended as second-line agents, with dobutamine considered a third-line option for patients with refractory hypoperfusion or with suspected low cardiac output despite adequate volume resuscitation. (12)
Corticosteroids:
The evidence for routine use of corticosteroids in patients with septic shock is conflicting, and the 2016 Surviving Sepsis guidelines suggest administration of IV hydrocortisone only in patients who remain hemodynamically unstable despite appropriate treatment with fluids and vasopressors. (12) Since the development of the 2016 guidelines, two large, multi-center, randomized controlled trials investigating the use of corticosteroids in septic shock were published, with conflicting results. The ADRENAL trial found no benefit in 90-day mortality to continuous infusion of hydrocortisone in patients with septic shock undergoing mechanical ventilation (15), while the APROCCHSS trial found that co-administration of hydrocortisone and fludrocortisone conferred a 90-day mortality benefit in ICU patients with septic shock. (16) Subsequent meta-analyses concluded that corticosteroid administration resulted in no mortality benefit at or beyond 90 days (17), or small or no reduction in mortality. (18) Furthermore, a 2015 study found that administration of hydrocortisone in patients with sepsis did not reduce development of septic shock within 14 days, and had no impact on all-cause mortality up to 180 days. (19) While studies regarding mortality benefit are conflicting and current guidelines recommend against the use of steroids in patients with sepsis without accompanying hypotension (12), it is widely accepted that steroids will decrease vasopressor requirements.
Antimicrobials:
In addition to interventions to restore hemodynamic stability, early administration of appropriate antimicrobials is the cornerstone of treatment for patients with sepsis and septic shock. Empiric therapy should be sufficiently broad to cover all likely pathogens based on clinical picture, suspected source of infection, and patient-specific risk factors (12). While there is no doubt that appropriate antibiotic therapy is an essential component of sepsis care, there is conflicting data regarding the exact time frame in which antibiotic administration should occur. The 2016 Surviving Sepsis recommendation is as soon as possible and within 1 hour of the recognition of sepsis with or without shock, ideally after blood cultures are drawn. (12) In patients with septic shock specifically, a landmark 2006 study found that administration of appropriate antimicrobials within 1 hour of documented hypotension was associated with a significant mortality benefit; furthermore, within the first six hours of recognized hypotension, each 1-hour delay in antimicrobial administration conferred an average 7.6% decrease in survival. (20) More recently, a retrospective analysis of more than 49,000 emergency department patients that found each 1-hour delay in antibiotic administration from the time of hospital arrival conferred a 4% increase in in-hospital mortality among patients with severe sepsis or septic shock. (21) In contrast, a 2015 systematic review and meta-analysis using pooled data from 11 studies, and incorporating over 16,000 patients, found no mortality benefit to administration of antibiotics within 3 hours of emergency department triage or within 1 hour of recognition of severe sepsis or septic shock. (22) Notably, the Infectious Disease Society of America declined to endorse the 2016 Surviving Sepsis guidelines, in part due to the “overly rigid” 1-hour time frame for initiation of antibiotics, citing concern that it could promote administration of broad-spectrum antibiotics in uninfected patients for the sake of compliance with a potentially-arbitrary metric. The IDSA did voice explicit agreement, however, that antibiotics should be administered as soon as possible in patients with suspected severe infection. (23)
For emergency department providers in the United States, the timing of interventions is ultimately dictated by the CMS SEP-1 severe sepsis/septic shock bundle. Within 3 hours of presentation with severe sepsis, CMS mandates that patients must have an initial lactate measurement, receive appropriate antibiotics, and have blood cultures drawn before antibiotic administration. If the initial lactate is elevated, a repeat level must be drawn within 6 hours. Patients presenting in septic shock must additionally receive an initial 30 mL/kg crystalloid bolus within 3 hours, vasopressors within 6 hours if still hypotensive despite fluid resuscitation, and a documented repeat assessment of volume and perfusion status within 6 hours if requiring vasopressor support or if initial lactate was ≥4 mmol/L. (2)
Development of new and adjunctive therapies for sepsis is an area of ongoing research, and while numerous investigational therapies exist, vitamin C and thiamine have, in particular, gained widespread attention. In 2017, a small, single-center retrospective before-and-after study found marked improvement in the clinical course of ICU patients admitted with severe sepsis or septic shock after treatment with intravenous hydrocortisone, vitamin C, and thiamine. All-cause hospital mortality in the treatment group was 8.5%, compared with 40.4% in the control group (p<0.001). Moreover, all patients in the treatment group survived to ICU discharge, and subsequent deaths in the group were attributed to underlying diseases rather than complications of sepsis. (24) While additional studies are needed to validate these findings, the utility of vitamin C and thiamine in the treatment of sepsis continues to be an area of active research with more than 20 related trials currently registered with the NIH.
Summary:
Sepsis = dysregulated immune response to infection causing organ dysfunction.
Empiric antibiotic therapy should be broad and should be initiated as soon as possible
Source Control is a key component in the treatment and reversal of sepsis
Current recommendation for volume resuscitation is 30 mL/kg crystalloid within 3 hours, with need for additional fluid determined by clinician judgement.
Transfusion of RBCs is recommended only for hemoglobin <7 in absence of active hemorrhage, MI, other extenuating circumstances.
Vasopressors should be used to maintain MAP ≥65. Norepinephrine is first line. Vasopressin or epinephrine is second line. Dobutamine may be considered in refractory cases. Dopamine is associated with higher mortality than norepinephrine and is generally not recommended as first-line agent.
IV corticosteroids are recommended only in septic shock refractory to adequate fluid resuscitation and vasopressors.
Development of new and adjunctive therapies for sepsis is an area of ongoing research.
References:
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest. 1992;136(5 Suppl):e28.
Centers for Medicare and Medicaid Services. Sepsis Bundle Project (SEP) Specifications Manual for National Hospital Inpatient Quality Measures Discharges 10-01-15 (4Q15) through 06-30-16 (2Q16). 2015. [Accessed February 6, 2019]. Available at: https://www.nhfca.org/psf/resources/Updates1/SEP-1%20Measure%20Information%20Form%20(MIF).pdf.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707-710.
Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315(8):801-810.
Song J, Sin CK, Park HK, et al. Performance of the quick Sequential (sepsis-related) Organ Failure Assessment score as a prognostic tool in infected patients outside the intensive care unit: a systematic review and meta-analysis. Crit Care. 2018;22:28.
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368-1377.
The ProCESS Investigators. A Randomized Trial of Protocol-Based Care for Early Septic Shock. N Engl J Med. 2014;370(18):1683-1693.
The ARISE Investigators and the ANZICS Clinical Trials Group. Goal-Directed Resuscitation for Patients with Early Septic Shock. N Engl J Med. 2014;371(16):1496-1506.
Mouncey PR, Osborn TM, Sarah PG, et al. Trial of Early, Goal-Directed Resuscitation for Septic Shock. N Engl J Med. 2015;372(14):1301-1311.
The PRISM Investigators. Early, Goal-Directed Therapy for Septic Shock – A Patient-Level Meta-Analysis. N Engl J Med. 2017;376(23):2223-2234.
Angus DC, Barnato AE, Bell D, et al. A systematic review and meta-analysis of early goal-directed therapy for septic shock: the ARISE, ProCESS and ProMISe Investigators. Intensive Care Med. 2015;41:1549-1560.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving Sepsis Campiagn: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43:304-377.
Holst LB, Haase N, Wetterslev J, et al. Lower versus Higher Hemoglobin Threshold for Transfusion in Septic Shock. N Engl J Med. 2014;371(15):1381-1391.
Avni T, Lador A, Lev S, et al. Vasopressors for the Treatment of Septic Shock: Systematic Review and Meta-Analysis. PLoS ONE. 2015;10(8):e0129305.
Venkatesh B, Finfer S, Cohen J, et al. Adjunctive Glucocorticoid Therapy in Patients with Septic Shock. NEJM. 2018;378(9):797-808.
Annane D, Renault A, Brun-Biusson B, et al. Hydrocortisone plus Fludrocortisone for Adults with Septic Shock. NEJM. 2018;378(9):809-818.
Rygard SL, Butler E, Granholm A, et al. Low-dose corticosteroids for adult patients with septic shock: a systematic review with meta-analysis and trial sequential analysis. Intensive Care Med. 2018;44:1003-1016.
Rochwerg B, Oczkowski SJ, Siemieniuk RAC, et al. Corticosteroids in Sepsis: An Updated Systematic Review and Meta-Analysis. Crit Care Med. 2018;46(9):1411-1420.
Keh D, Trips E, Marx G, et al. Effect of Hydrocortisone on Development of Shock Among Patients With Severe Sepsis: The HYPRESS Randomized Clinical Trial. JAMA. 2016;316(17):1775-1785.
Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34(6):1589-1596.
Seymour CW, Foster G, Prescott HC, et al. Time to Treatment and Mortality during Mandated Emergency Care for Sepsis. N Engl J Med. 2017;376(23):2235-2244.
Sterling SA, Miller WR, Pryor J. The Impact of Timing of Antibiotics on Outcomes in Severe Sepsis and Septic Shock: A Systematic Review and Meta-Analysis. Crit Care Med. 2015;43(9):1907-1915.
IDSA Sepsis Task Force. Infectious Disease Society of America (IDSA) POSITION STATEMENT: Why IDSA Did Not Endose the Surviving Sepsis Campaign Guidelines. Clin Infect Dis. 2018;66(10):1631-1635.
Marik PE, Khangoora V, Rivera R, et al. Hydrocortisone, Vitamin C, and Thiamine for Treatment of Severe Sepsis and Septic Shock. Chest. 2017;151(6):1229-1238.