Annals of B Pod - Neurolisteriosis
/HISTORY OF PRESENT ILLNESS
The patient is a Swahili-speaking female in her 40s with a past medical history of HIV on HAART who presents to the emergency department (ED) after being found unresponsive. Family reports that the patient was last seen well approximately 14 hours prior to presentation. The patient is minimally responsive and unable to provide any further history.
Chart review reveals a recent admission five days prior for psychosis and visual hallucinations for which outpatient risperidone was initiated. The patient was seen at that time for dizziness and palpitations. During admission, serum labs, urine labs, and non-contrast head CT were within normal limits, and blood and urine cultures had been sent. She was noted to be slightly confused, but this was thought to be secondary to dehydration. She was discharged home in stable condition after improvement in symptoms.
Past medical history: HIV, psychosis with delusions
Past surgical history: None
Medications: Risperidone, bictegrav-emtricit-tenofov alafenamide, folic acid
Allergies: No known allergies
Physical exam
Vitals: T 40.0 HR 125 BP 119/47 RR 29 SpO2 98% on RA
The patient is lethargic, does not attend or regard, and is nonverbal and minimally responsive to painful stimuli. Her pupils are equal, round, and reactive to light, and a disconjugate gaze is present. The patient blinks to confrontation in all visual fields and her face is grossly symmetric. She is noted to have rigidity in all four extremities, left greater than right. She favors the flexed position of extremities, but allows for passive extension. She demonstrates areflexia in biceps, triceps, patellar and Achilles tendons bilaterally with a negative Babinski bilaterally. She is noted to be tachycardic, otherwise cardiopulmonary exam is unremarkable. There are no external signs of trauma, and the patient is incontinent of stool and urine.
Diagnostics
WBC: 10 Hgb: 13.3 Hct: 39.4 Plt: 204
Na: 141 K: 3.6 Cl: 105 HCO3: 21 BUN: 21 Cr: 1.56 Glucose: 360
VBG: pH: 7.4 pCO2: 37 BE: -1.4
Lactate: 3.4 Troponin: 0.06 CK: 11,839
ALT: 87 AST: 109 Tbili: 0.4 Alk phos: 54 Albumin: 3.6
TSH: 0.8 fT4: 1.17
EtOH: negative Salicylate: negative Tylenol: negative
UDS: negative
Upreg: negative
CT head: negative for acute intracranial process
EKG: T wave inversions in V3-V6, no prior to compare
Lumbar Puncture: opening pressure 29 cm H20
Tube 1 WBCs: 4534
RBCs: 1024
Tube 4 WBCs: 1560
RBCs: 5996
Glucose: 90
Protein: 259
Hospital Course
Given the patient’s fever, tachycardia and altered mental status, a broad work up was initiated to include intracranial, infectious, metabolic, and toxidrome-related etiologies. She was started on vancomycin, ceftriaxone, and acyclovir for empiric antimicrobial coverage of encephalitis or meningitis. She was given acetaminophen for her fever, resuscitated with intravenous fluid, and started on external cooling measures. Due to concern for possible neuroleptic malignant syndrome given the recent initiation of risperidone, the patient was empirically given dantrolene. Her mental status did not improve while in the ED and she was admitted to the neurosciences intensive care unit (NSICU).
In the NSICU, providers added voriconazole and ampicillin to cover for fungal and additional bacterial pathogens due to the patient’s history of HIV. Infectious disease was consulted, along with psychiatry to rule out malignant catatonia as a possible etiology of her symptoms. Continuous video electroencephalography (EEG) showed no seizure activity and magnetic resonance imaging (MRI) found no focal abnormalities.
During hospitalization, the patient’s blood cultures grew Staphylococcus epidermidis and Listeria monocytogenes. Cerebrospinal fluid (CSF) cultures also grew L. monocytogenes. Records from the prior outside hospital visit were later obtained and revealed positive blood cultures for L. monocytogenes. Antibiotic therapy was narrowed to vancomycin and ampicillin based on these culture results. The patient’s mental status improved dramatically throughout her hospitalization, and she was able to be discharged to inpatient rehabilitation on hospital day 10. The patient was discharged with a three-week course of ampicillin and a two-week course of vancomycin. The patient was neurologically intact at her infectious disease appointment several months later.
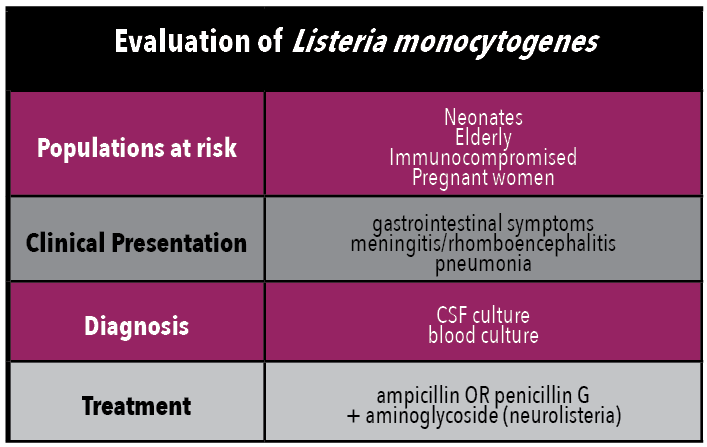
Neurolisteriosis
Epidemiology and Pathophysiology
L. monocytogenes is an aerobic and facultatively anaerobic, motile, fastidious gram-positive rod that is naturally occurring in soil, water, and flora. Exposure is most often from ingestion of unpasteurized milk, soft cheeses, deli meats, and smoked seafood. [1] After ingestion, bacteria invade the intestinal mucosa and spread systemically. L. monocytogenes’s ability to grow at refrigerated temperatures contributes significantly to its ability to cause foodborne illness in the developed world.
Infection with L. monocytogenes is relatively rare, especially in immunocompetent patients, and commonly presents as a self-limited disease of the gastrointestinal tract. However, L. monocytogenes has demonstrated a particular predilection for the central nervous system (CNS), thus has significant potential as an invasive pathogen, especially in neonatal and elderly populations. Primary immunity against L. monocytogenes is from T-cell lymphocytic activation of macrophages, thus immunosuppressed and immunocompromised patients are at higher risk of infection. [2] Interestingly, the use of stomach acid suppressants has also been described as a risk factor for infection. [1] Incubation period ranges from several days to up to four weeks depending upon an individual’s risk factors.
Pregnant women are another population with increased susceptibility to listeriosis. One in seven cases of listeriosis occurs in pregnant women, attributed to the suppressed cell-mediated immunity of pregnancy. Maternal infection is associated with increased rates of miscarriage, preterm labor, stillbirth, and fetal demise; [3] one study demonstrated major fetal and neonatal complications in greater than 80% of pregnant women infected prior to 29 weeks of gestation. [2] Additionally, infection can be vertically transmitted from mother to the fetus and can, very rarely, lead to granulomatosis infantiseptica, a severe form of fetal infection leading to pyogenic granuloma formations in all internal fetal organs. [4] This may occur with relatively little symptomology of the mother and usually goes undiagnosed until birth. Pregnant women are not at increased risk of neuro-invasive listeriosis, suggesting that placental and CNS infection mechanisms differ. [5]
Regardless of risk factors, invasive listeriosis confers a mortality rate estimated at 20%. [6] In the United States, an estimated 1,600 people contract invasive listeriosis each year, of which an estimated 260 die from infection. [6]
Clinical Presentation
L. monocytogenes has well-described neuro-invasive potential, also known as neurolisteriosis, most commonly presenting as meningitis. [2] While L. monocytogenes accounts for only four percent of bacterial meningitis cases in patients aged two to 60, it is responsible for 25% of cases in patients younger than two and older than sixty years. [7] Thus, both neonatal and elderly patients with a high clinical suspicion for meningitis are empirically treated for L. monocytogenes. Unlike meningitis, encephalitis is relatively rare; it is estimated that anywhere from 6-24% of patients with neurolisteriosis exhibit signs of encephalitis presenting as focal neurologic deficits or seizures. [8]
Another presentation of neurolisteriosis is rhomboencephalitis, a focal encephalitis involving the brainstem and/or cerebellum. L. monocytogenes rhomboencephalitis has a characteristic biphasic disease course. Typically, it begins with a prodrome of headache, nausea, and fever which lasts for several days. The second phase then develops abruptly with the onset of asymmetric or unilateral cranial nerve deficits, cerebellar signs, and hemiparesis or hemisensory deficits. [5,8] In contrast to other presentations of neurolisterosis, rhomboencephalitis occurs primarily in otherwise healthy individuals. [5] While the mechanism is unclear, one study posited that L. monocytogenes may access the brainstem directly via cranial nerves, thus bypassing the body’s immune defenses. In some animal models, conjunctival or buccal inoculation with L. monocytogenes has resulted in rhomboencephalitis. [9] Rhomboencephalitis is not unique to L. monocytogenes; it has also been described with Epstein-Barr virus, tuberculosis, JC virus, multiple sclerosis, and Behcet’s disease. [10]
Respiratory complications are commonly associated with neurolisteriosis as well. Pneumonia affects an estimated 17% of patients with L. monocytogenes meningoencephalitis, which is significantly higher than rates observed in meningitis alone. [8] In cases of rhomboencephalitis, respiratory failure occurs in an approximately 41% of patients. Case studies cite impingement of abscesses on the medullary respiratory center or the development of obstructive hydrocephalus as possible etiologies. [9]
In pregnancy, L. monocytogenes infection can present with a broad range of symptoms. Many patients will present with fever and nonspecific flu-like symptoms while having disseminated infection and bacteremia. Some may present with primary gastrointestinal symptoms. Others may be completely asymptomatic. Thus, providers must remain vigilant during the course of a patient’s pregnancy, especially in those with risk factors for L. monocytogenes, as both maternal and fetal morbidity and mortality rates are high.
Diagnosis
Suspicion of neurolisteriosis should be based on clinical presentation and risk factors. However, there is no particular historical factor or physical exam finding that will differentiate between L. monocytogenes infection and other etiologies of meningoencephalitis disease. Thus, diagnosis largely depends on isolation of the organism via cerebrospinal fluid (CSF) or blood cultures. [1,10] In regards to CSF results, L. monocytogenes is unique in that it is one of the only nontuberculous bacteria that will have lymphocytosis in addition to increased protein and decreased glucose on CSF analysis. [4] However, providers must be aware that CSF culture sensitivity may be reduced when encountering more focal CNS infections. In regard to blood cultures, L. monocytogenes is a fastidious organism which requires Meuller-Hinton agar for growth, and as such, many patients with neurolisteriosis will not develop positive blood cultures. [1] It is estimated that positive blood cultures occur in only 61-63% of cases of L. monocytogenes encephalitis. [2,8] Blood cultures may be of limited utility due to two reasons: L. monocytogenes is an intracellular parasite and may not be detectable; and it is oftentimes mistaken for diplococci or diphtheroids, therefore it may be named a contaminant if providers are not aware of the clinical suspicion for L. monocytogenes infection. [11] Mortality rates are higher in patients with positive blood cultures, suggesting patients with concomitant bacteremia and neurolisteriosis may have a more severe disease profile. [2]
Stool cultures do not typically play a role in diagnosis of L. monocytogenes, even during pregnancy. The bacterium is commonly present in the environment, and has been isolated from the gut of asymptomatic humans in several studies, therefore intermittent carriage and shedding may occur that does not always indicate active infection. [12] Furthermore, most gastrointestinal illnesses self-resolve and do not require antibiotic therapy.
Cross-sectional imaging of the brain is recommended in cases of suspected or confirmed neurolisteriosis, as brain abscesses and obstructive hydrocephalus are well described complications. [1,9] MRI should be strongly considered in cases of L. monocytogenes encephalitis or rhomboencephalitis if there is any clinical uncertainty or suspicion for intraparenchymal involvement. In a case series of nine patients with confirmed L. monocytogenes rhomboencephalitis, only one patient had a normal MRI, indicating that detection of neurosurgically-intervenable lesions are commonly identified. [9]
Treatment
Ampicillin or penicillin G are recommended as first-line agents for L. monocytogenes infections. Although aminoglycosides have poor CNS penetration, a 2017 large prospective observational study demonstrated possible mortality benefit when used in conjunction with beta lactam antibiotics in patients with neurolisteriosis or bacteremia that portends a higher risk for CNS infection. [2] Bactrim is an acceptable second-line therapy for those patients with a penicillin or beta lactam allergy. [1] L. monocytogenes is resistant to all cephalosporins, and some strains have developed complete resistance to vancomycin as well. [13] Less commonly used antibiotics, such as meropenem and linezolid, have efficacy against L. monocytogenes, however these are primarily anecdotally used and only in severe circumstances. Duration of antibiotic therapy largely depends on degree of dissemination, however neurolisteriosis requires at least six weeks of antibiotic therapy. [14]
One study found that neurolisteriosis treated with dexamethasone in addition to antibiotics significantly increased mortality. [2] Thus, steroids are not recommended in the treatment of Listeria encephalitis and rhomboencephalitis, and if initiated empirically at patient presentation, use should be discontinued as soon as L. monocytogenes infection is confirmed. [2]
Reported mortality rates differ widely, as L. monocytogenes encephalitis and rhomboencephalitis are overall uncommon entities. In one case review, 100% of untreated patients died; of those treated early with ampicillin or penicillin, mortality rates were less than 30%. [8] Mortality rates were higher in patients with underlying malignancies, diabetes, poorly controlled comorbidities, and those who developed multi-organ failure, [2] whereas otherwise healthy patients had lower mortality rates. CNS infection and bacteremia have 30% and 45% mortality rates, respectively. [2] These reviews suggest that early detection and early institution of antibiotic therapy can be very effective in treating life-threatening L. monocytogenes infection, thus empiric coverage should be considered in patients with suspected exposure. [2,3,15] Of those that develop neurolisteriosis and survive, permanent neurologic sequelae remained in 61% of survivors. [8]
Summary
In summary, neurolisteriosis is a rare disease process with a high morbidity and mortality that can affect both immunocompetent and immunocompromised individuals, particularly those at extremes of age and during pregnancy. Early recognition is critical in order to ensure appropriate treatment and improve survival rates.
AUTHORED BY Sarah Wolochatiuk, MD
Editing BY the Annals of B Pod Editors
References
Rogalla D, Bomar PA. Listeria monocytogenes. [Updated 2019 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www-ncbi-nlm-nih-gov.proxy.libraries.uc.edu/books/NBK534838/
Charlier C, Perrodeau É, Leclercq A, Cazenave B, Pilmis B, Henry B, Lopes A, Maury MM, Moura A, Goffinet F, Dieye HB. Clinical features and prognostic factors of listeriosis: the MONALISA national prospective cohort study. The Lancet Infectious Diseases. 2017 May 1;17(5):510-9.
Craig AM, Dotters-Katz S, Kuller JA, Thompson JL. Listeriosis in pregnancy: a review. Obstetrical & Gynecological Survey. 2019 Jun 1;74(6):362-8.
Gelfand M. Clinical manifestations and diagnosis of Listeria monocytogenes infection. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-listeria-monocytogenes-infection?search=listeria monocytogenes infection&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. Accessed December 29, 2019.
Disson O, Lecuit M. Targeting of the central nervous system by Listeria monocytogenes. Virulence. 2012 Mar 1;3(2):213-21.
Angelo KM, Jackson KA, Wong KK, Hoekstra RM, Jackson BR. Assessment of the incubation period for invasive listeriosis. Clinical Infectious Diseases. 2016 Dec 1;63(11):1487-9.
Schuchat A, Robinson K, Wenger JD, Harrison LH, Farley M, Reingold AL, Lefkowitz L, Perkins BA. Bacterial meningitis in the United States in 1995. New England journal of medicine. 1997 Oct 2;337(14):970-6.
Armstrong RW, Fung PC. Brainstem encephalitis (rhombencephalitis) due to Listeria monocytogenes: case report and review. Clinical Infectious Diseases. 1993 May 1;16(5):689-702.
Workman S, Theal M. Rhomboencephalitis caused by Listeria monocytogenes. Canadian Journal of Infectious Diseases. 1997 Mar;8.
Moragas M, Martínez-Yélamos S, Majós C, Fernández-Viladrich P, Rubio F, Arbizu T. Rhombencephalitis: a series of 97 patients. Medicine. 2011 Jul 1;90(4):256-61.
Mylonakis E, Paliou M, Hohmann EL, Calderwood SB, Wing EJ. Listeriosis during pregnancy: a case series and review of 222 cases. Medicine 2002;81:260–9.
Lamont RF, Sobel J, Mazaki-Tovi S, Kusanovic JP, Vaisbuch E, Kim SK, et al. Listeriosis in human pregnancy: a systematic review. J Perinat Med 2011;39:227–36.
Cherubin CE, Appleman MD, Heseltine PN, Khayr W, Stratton CW. Epidemiological spectrum and current treatment of listeriosis. Reviews of infectious diseases. 1991 Nov 1;13(6):1108-14.
Mylonakis E, Hohmann EL, Calderwood SB. Central Nervous System Infection withListeria monocytogenes: 33 Years' Experience at a General Hospital and Review of 776 Episodes from the Literature. Medicine. 1998 Sep 1;77(5):313-36.
Mansbridge CT, Grecu I, Chong JS, Vandervelde C, Saeed K. Two cases of listeria rhombencephalitis. IDCases. 2018 Jan 1;11:22-5.