B Pod Case: Double Vision
/78 year old male with past medical history coronary artery disease status post stenting, hypertension, hyperlipidemia, chronic kidney disease presents with a chief complaint of double vision, feeling off balance. Patient states he awoke this morning with double vision. He states this sensation of double vision is worse when he looks side to side, and completely resolves when he closes one of his eyes. He does not wear glasses or contacts and denies any eye pain or trauma. Also, since this morning he has felt somewhat off balance, however denies any focal numbness or weakness of extremities. He noted an episode of slurred speech approximately 1 hour prior to arrival that has since resolved. No other difficulties with word finding or language. Otherwise patient denies headache, head trauma, neck pain, chest pain, or shortness of breath. He has not had symptoms like this in the past.
Past Medical History
Coronary artery disease status post stenting to LAD x 1, Hypercholesterolemia, Hypertension, Chronic Renal Insufficiency, Anemia
Past Surgical History
Coronary stent placement to LAD- 2003, Appendectomy- 1986
Medications
Aspirin 81mg, atorvastatin, labetalol,
Social History
Drinks EtOH socially. Denies tobacco or illicit drug use
Physical Exam
Vital Signs: T 97.5, HR 94, RR 20, BP 146/76, O2 97% on room air, Blood glucose 150
Constitutional: Well developed, well nourished, male sitting upright in no acute distress, non-toxic appearance
Eyes: PERRL, conjunctiva normal. Left eye with full extraocular movements in all directions. Right eye has full lateral abduction, however is unable to adduct his right eye medially past midline when looking left. Left eye with nystagmus with leftward gaze. No ptosis, hyphema, hypopyon present.
HENT: Atraumatic, external ears normal, nose normal, oropharynx moist, no pharyngeal exudates. Neck- normal range of motion, no tenderness, supple
Neurologic: Alert & oriented x 3, Patient unable to adduct right eye medially past midline when looking left, and left eye with nystagmus with leftward gaze. Accommodation intact. No ptosis, symmetric eyebrow raise, normal smile without facial droop. Past-pointing with left upper extremity with finger to nose. Intact 5/5 motor strength in upper and lower extremities, sensation intact upper and lower extremities. Gait unsteady with mild gait ataxia. NIHSS 2 for partial gaze palsy and limb ataxia.
Psychiatric: Speech and behavior appropriate
Hospital Course
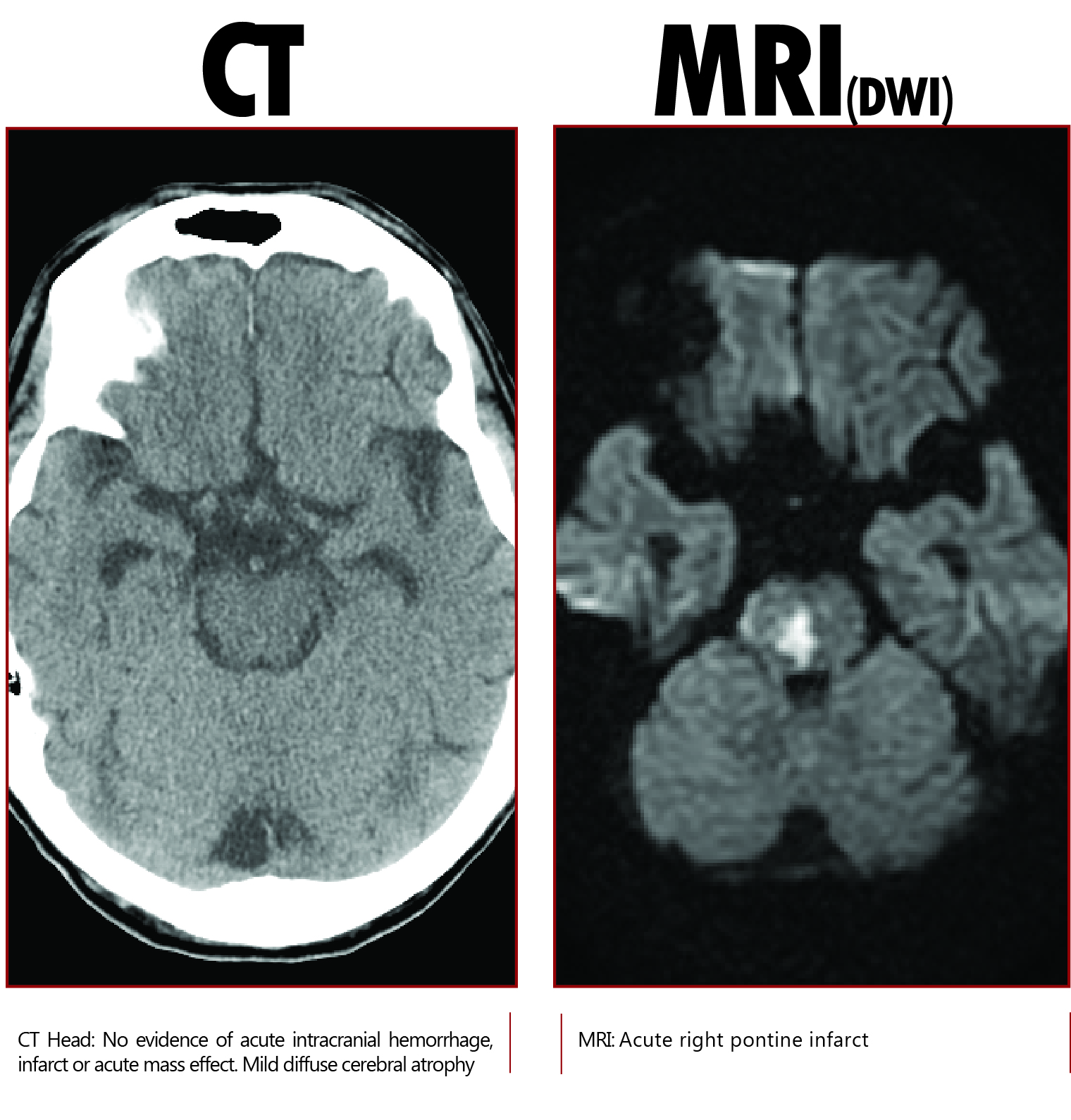
Patient with NIHSS of 2 for partial gaze palsy (Right internuclear ophthalmoplegia) and limb ataxia. Not a tPA candidate as last seen normal > 4.5 hours previously. Patient subsequently admitted to neurology service for further evaluation and management of symptoms concerning for posterior circulation infarct. .
CTA Head/Neck: 70% or greater stenosis of the proximal left vertebral artery, with 50% stenosis of the distal right vertebral artery beyond PICA, and 50% stenosis of the basilar artery beyond AICA.
Given stroke in the setting of severe intracranial stenosis, patient was started on dual antiplatelet agents with ASA and Plavix. Symptoms of diplopia and ataxia improved. Interventional Neuroradiology was consulted for severe left vertebral artery stenosis who recommended aggressive medical therapy, with the possibility of intracranial vascular stenting should symptoms recur. Patient discharged home in stable condition on hospital day # 4 with home health and physical therapy resources.
Approach to the Patient with Diplopia
Diplopia is defined as the perception of 2 images of a single object. [1] In the evaluation of diplopia, the first step is to determine if the patient is demonstrating monocular or binocular diplopia. To test this, have the patient close one of their eyes. If diplopia persists with one eye closed, this is called monocular diplopia, and occurs due to a distortion of light transmission through the eye to the retina. Common causes of monocular diplopia include cataracts, corneal irregularities, and refractive errors such as astigmatism. [2] If diplopia is present with both eyes open but disappears when one eye is closed, this is termed binocular diplopia. It's key to differentiate between these two entities because the pathophysiology and diagnostic implications of each are different.
Monocular diplopia is secondary to local eye disease, and workup can typically be deferred to outpatient ophthalmology follow- up. Binocular diplopia on the other hand occurs secondary to disconjugate alignment of the eyes, and has a broad differential diagnosis. Cranial nerve palsies are the most common cause of binocular diplopia, typically involving cranial nerves 3, 4 or 6. Other differential considerations causing ocular misalignment include neuromuscular transmission disorders, and those processes causing mechanical interference with ocular motion. [1] Suggestive findings on history and physical exam can help differentiate between these causes and help guide further workup and neuroimaging.
Video from NEJM video series - http://youtu.be/U2ue1YFjhms - Patient with MS demonstrating bilateral internuclear ophthalmoplegia.
As in our patient, a finding of an internuclear ophthalmoplegia on physical exam can provide important clues to the etiology and localization of pathology causing binocular diplopia. Internuclear ophthalmoplegia (INO) is characterized by paresis of eye adduction in horizontal gaze, but not in convergence. (See attached image) In other words, on horizontal gaze testing there is diplopia, weak adduction of the affected eye (typically can’t adduct past midline), and nystagmus of the contralateral eye. [1] This occurs secondary to a lesion in the medial longitudinal fasciculus (MLF) in the dorsomedial brainstem tegmentum of the pons or midbrain. [3] The most common causes of an INO vary by patient demographics. In younger patients < 45 years, the most common cause of INO is multiple sclerosis, and these defects are typically bilateral, up to 73%. In older patients > 60, and especially those with cardiovascular risk factors, the most common cause of INO is an ischemic infarction of the pons or medulla, and the findings are typically unilateral. [4] The pathophysiology of this infarct is typically small artery occlusion or lacunar disease involving the penetrating arteries originating from the basilar artery. [3] Other causes of INO include infections, tumor, and trauma.
Case seen and written by Megan Redmond, MD. Dr. Redmond is an R4 in Emergency Medicine at the University of Cincinnati.
References
1. Colby, K. Diplopia: Symptoms of Ophthalmologic Disorders. In Merck manual online: Professional Edition. (Accessed on November 30, 2014) http://www.merckmanuals.com/professional/eye_disorders/symptoms_of_ophthalmologic_disorders/diplopia.html
2. Bienfang, DC. Overview of Diplopia. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on December 1, 2014.) http://www.uptodate.com/contents/overview-of-diplopia?source=machineLearning&search=diplopia&selectedTitle=1%7E150§ionRank=1&anchor=H14#H14
3. Frohman, EM; Frohman, TC. Internuclear Ophthalmoparesis. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA. (Accessed on December 1st 2014.) http://www.uptodate.com/contents/internuclear-ophthalmoparesis?source=search_result&search=ino&selectedTitle=1%7E19
4. Keane JR. Internuclear ophthalmoplegia: unusual causes in 114 of 410 patients. Arch Neurol 2005; 62:714.