EKG Toxicology
/Emergency medicine physicians frequently assess and treat patients who have accidental or intentional poisonings. United States poison centers receive over two million case referrals per year. And, about 20% of these poisonings present to an Emergency Department for evaluation. Evaluation of these patients always includes a history and physical, but further testing can provide valuable information. Blood work is often be needed, but an EKG is a faster, cheaper tool that can provide key pieces of information prompting early interventions.
Brief History of EKG
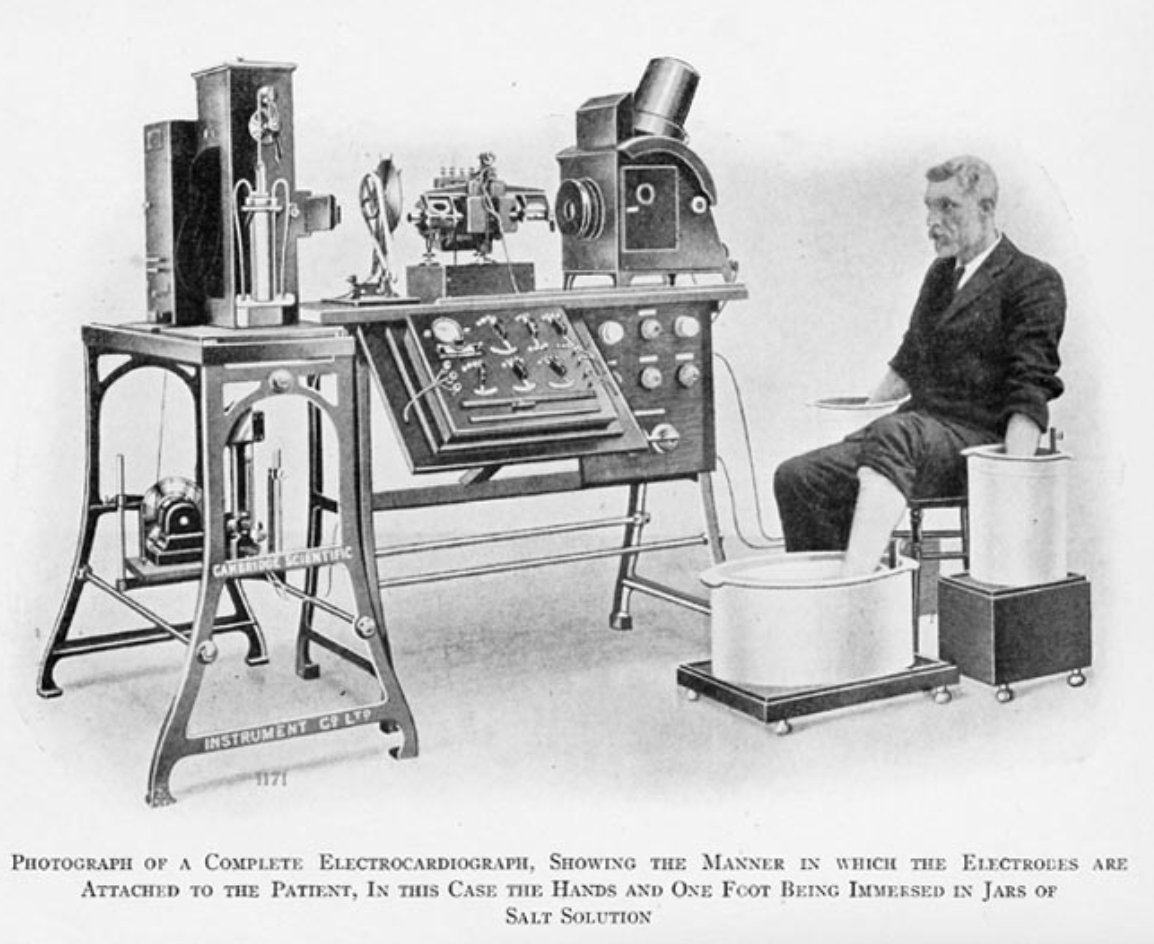
The EKG was invented by Dr. Willem Einthoven, a Dutch physiologist. He created a large machine that could measure electrical waveforms in 1901. Over the next few years he published the first EKG recorded, discussed commercial production of his device, transmitted EKG through telephone wires, and presented normal and abnormal EKG recordings. Eventually, he won a Nobel Prize in physiology and medicine in 1924.
Why EKG?
Thankfully, our EKG machines today are much less complicated. The EKG is an extremely valuable tool in the evaluation of poisoned patients for the following reasons:
- Not an expensive test
- Available in almost all clinical settings
- Quick and can provide information before blood work is resulted
- Can screen for potentially lethal arrhythmia
- Can monitor progress of treatments
- Help determine disposition
A Brief Physiology Flashback
The cardiac action potential is composed of four phases where multiple ions move across membranes causing depolarization and repolarization. Many cardiac medications target channels to have a desired clinical effect. However, many other medications may also affect these channels even if they are not meant to treat heart conditions.
Phase 0 of the cardiac action potential occurs when a rapid influx of sodium ions into the cell. Certain drugs have sodium channel blocking properties. Class I anti-arrhythmic medications purposely block sodium channels for a desired effect, however other drugs, such as tricyclic antidepressants, also block sodium channels. Blocking sodium channels decreases the slope of phase 0 of the action potential resulting in a widening of the QRS on the EKG.
Phase 2 and phase 3 of the action potential are affected by potassium channel blockade. Preventing the efflux of potassium ions prolongs cardiac repolarization. As a result, we see QT interval prolongation on the EKG. Class III anti-arrhythmic medications are potassium channel blockers which specifically target this mechanism. Many other medications such antipsychotics, antidepressants, antihistamines, and antimicrobials also have potassium channel blocking effects and can lead to a prolonged QT interval. Torsades de pointes is a dangerous phenomenon that can occur with QT interval prolongation.
Let’s work through a case!
When we approach a poisoned patient, identifying symptoms or toxidromes is the key first step to help guide our interpretation of EKGs. Having a high suspicion for toxicities and recognizing patterns on EKGs is essential for treating poisoned patients who may be undergoing a cardiotoxic process.
A 57 year old female is brought in by EMS. Report reveals that she was found down at home by family and has been bradycardic and hypotensive. There was an empty pill bottle at the scene, but it was left at the patient’s home. Patient refuses to reveal what medications she takes and family is unsure as well. Patient is from a different state and the electronic medical record is unhelpful.
Vitals: HR 45, BP 85/50, SpO2 99% on RA, Temp 98 F
A EKG is done immediately and is shown below:
How would you interpret this?
What additional “vital sign” could be helpful in an overdose patient who is bradycardic and hypotensive?
Besides bradycardia, what other findings are common EKG findings in CCB toxicity?
How does CCB toxicity affect cardiac physiology?
You have the EKG and finger stick glucose in this clinical picture, what would be your management strategy?
What is HIET?
EKG Changes and Toxicities to Consider
Author: James Li, MD
Editing and Uploading: Jeffery Hill, MD MEd
References
- Alghatrif, Majd, and Joseph Lindsay. “A Brief Review: History to Understand Fundamentals of Electrocardiography.” Journal of Community Hospital Internal Medicine Perspectives, vol. 2, no. 1, 2012, p. 14383., doi:10.3402/jchimp.v2i1.14383.
- Bernstein, Jeff, and Jeff Burgess. “Treatment of 150 Cases of Life-Threatening Digitalis Intoxication with Digoxin-Specific Fab Antibody Fragments.” Annals of Emergency Medicine, vol. 19, no. 12, 1990, pp. 1476–1477., doi:10.1016/s0196-0644(05)82635-6.
- Burns, Edward. “ECG Features of Digoxin Toxicity - LITFL ECG Library.” LITFL • Life in the Fast Lane Medical Blog, 4 Apr. 2017, lifeinthefastlane.com/ecg-library/basics/digoxin-toxicity/.
- Burns, Edward. “ECG Features of Tricyclic Antidepressant (TCA) Overdose - LITFL ECG Library.” LITFL • Life in the Fast Lane Medical Blog, 13 Apr. 2017, lifeinthefastlane.com/ecg-library/basics/tca-overdose/.
- Delk, Christopher, et al. “Electrocardiographic Abnormalities Associated with Poisoning.” The American Journal of Emergency Medicine, vol. 25, no. 6, 2007, pp. 672–687., doi:10.1016/j.ajem.2006.11.038.
- “Electrophysiologic and Electrocardigraphic Principles.” Goldfrank's Toxicologic Emergencies, by Lewis R. Goldfrank et al., McGraw-Hill Education, 2015.
- Klabunde, Richard. “Cardiac Glycosides (Digitalis Compounds).” Ardiac Glycosides (Digitalis Compounds), 3 Sept. 2015, www.cvpharmacology.com/cardiostimulatory/digitalis.
- “Lithium.” Rosen's Emergency Medicine: Concepts and Clinical Practice, by Peter Rosen et al., Elsevier, 2018.
- Mehta, Nikhil, and Robert Vannozzi. “Lithium-Induced Electrocardiographic Changes: A Complete Review.” Clinical Cardiology, vol. 40, no. 12, 2017, pp. 1363–1367., doi:10.1002/clc.22822.
- Nickson, Chris. “ECG in Toxicology • LITFL • Life in the Fast Lane Medical Blog.” LITFL • Life in the Fast Lane Medical Blog, 16 May 2013, lifeinthefastlane.com/ccc/ecg-in-toxicology/.
- Nickson, Chris. “Verapamil Overdose and High-Dose Insulin Euglycemic Therapy.” LITFL • Life in the Fast Lane Medical Blog, 24 May 2016, lifeinthefastlane.com/toxicology-conundrum-028/.
- Prosser, Jane M., et al. “Inaccuracy of ECG Interpretations Reported to the Poison Center.” Annals of Emergency Medicine, vol. 57, no. 2, 2011, pp. 122–127., doi:10.1016/j.annemergmed.2010.09.019’
- Wenzel-Seifert, Katharina, Markus Wittmann, and Ekkehard Haen. "QTc prolongation by psychotropic drugs and the risk of Torsade de Pointes." Deutsches Ärzteblatt International 108.41 (2011): 687.
- Yates, Christopher, and Alex F. Manini. “Utility of the Electrocardiogram in Drug Overdose and Poisoning: Theoretical Considerations and Clinical Implications.” Current Cardiology Reviews, vol. 8, no. 2, 2012, pp. 137–151., doi:10.2174/157340312801784961.