Diagnostics: MI in Left Bundle Branch Block
/Modified Sgarbossa Criteria
If any of the following criteria are present, consider immediate reperfusion:
Concordant ST elevation of 1 mm in any lead
Concordant ST depression of 1 mm in V1 - V3
Discordant ST/S ratio over 0.25 in any lead
Take Home Points
The Sgarbossa criteria have evolved since 1996 and are ready for clinical application
The modified Sgarbossa criteria have excellent sensitivity and specificity
These criteria can (probably) be applied to paced rhythms
What’s the big deal?
Left bundle branch block (LBBB) occurs in 6.7% of all patients presenting with acute myocardial infarction. [1] Presence of LBBB obscures many of the criteria used to determine whether an acute coronary occlusion (ACO) is present through changes to the ST-T segment and by altering ventricular depolarization. Patients with ACO in LBBB experience delays in treatment and worse outcomes when compared to patients without LBBB. [1,2] The criteria presented here allow immediate intervention, without the need for further workup or laboratory studies. As this is a “can’t miss” diagnosis that is relatively common in Emergency Medicine, it is imperative that we have validated tools for diagnosis.
A bit about the LBBB
The following are necessary for diagnosis:
Supraventricular rhythm
QRS > 120 ms
V1 must have a QS or rS complex
R wave peak time > 0.06 sec in lead I, V5, V6 without q-wave
Criteria 2 above is the direct result of slowed depolarization from right to left, as the normal conductive system is not functioning.
Criteria 3 and 4 above are directly related to the right-to-left depolarization pattern that occurs in LBBB. The dominant negative depolarization (S wave) in lead V1 occurs as electrical impulse moves away from the septum. The slow positive depolarization (R wave) in lead V6 occurs as the impulse moves toward the lateral aspect of the heart.
There are variations of the definition of a LBBB, these were used to develop the Sgarbossa criteria.
Sgarbossa Criteria
The Sgarbossa criteria were developed by comparing EKGs of 131 patients with LBBB and enzyme-proven myocardial infarction, to EKGs of patients with LBBB and angiography proven CAD but no active ischemia. LBBB was defined as meeting the criteria listed in the prior section. Patients with intermittent LBBB were excluded. The ST-segment deviation was measured at the J-point. [3]
Ten possible EKG criteria for ischemia were analyzed, and three of these criteria were selected as independent predictors of myocardial ischemia (table below). Weighted scores were assigned to each criterion, and a minimum score of 3 was found to have a specificity of 90%, but a sensitivity of 78% for myocardial ischemia. In a validation sample a score of three was demonstrated to have a specificity of 96%, but a sensitivity of just 36%. [3]
Later validation in a meta-analysis of 2100 patients yielded a similar specificity of 98%, but poorer sensitivity of 20%. [4] The third criteria adds little value as it alone does not trigger intervention, and the specificity of the other two criteria are already quite high. As CK-MB was used to define myocardial infarction, these criteria do not differentiate between STEMI and NSTEMI.
Modified Sgarbossa Criteria
Smith et al. attempted to improve the third criteria. Noting that patients could meet the criteria simply by having a higher amplitude EKG, and that repolarization voltages must be proportional to depolarization voltages, they proposed replacing the set ST elevation cut-off with a ST/S ratio. The image to the right demonstrates how these ratios can be calculated.
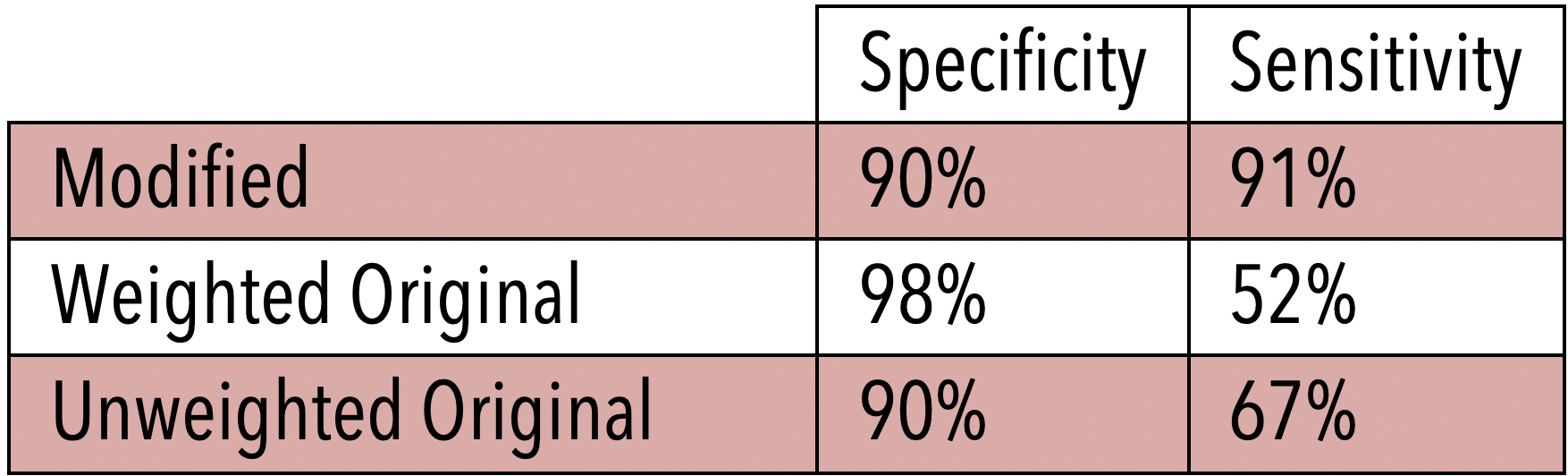
Initial EKGs for 33 patients with LBBB and ACO were compared with EKGs of 129 patients with LBBB and chest pain or dyspnea, but no ACO. Patients with hyperkalemia > 5.5, tachycardia > 130, hypertension with DBP > 120, and pulmonary edema with respiratory failure were excluded. Representative complexes were selected from each lead with > 1mm ST deviation and a dominant R or S wave of opposite polarity. ST deviation was measured at the J-point per ACC/AHA recommendations. [5] An ST/S ratio was calculated. A cut-point with >90% sensitivity was determined to be discordant ST/S ratio -0.25 mm in any lead. This new modified cut point was substituted for the last criteria used in the Sgarbossa study. The modified rule (without weights) was compared to both the weighted and unweighted versions of the original. The sensitivities and specificities are listed on the right. [6]
The increased sensitivity of the new rule was statistically significant when compared to either version of the original criteria. The specificity was not significantly different.
Algorithm using Smith-modified
Cai et al. proposed an algorithm for incorporation of the Smith modifications into clinical practice, which can be seen in the diagram here [7]:
This proposed algorithm is functionally equivalent to using an unweighted version of the original criteria with the Smith modification to the third criteria.
Validation of the combined criteria
In a retrospective case-control study, the original criteria (weighted and unweighted) were compared to the modified Sgarbossa criteria in the initial EKGs of LBBB patients with ACO (n=49) and without coronary occlusion (n=249). ACO was defined similarly to the criteria used in Smith et al. with: angiography demonstrating occlusion, culprit lesion with significantly elevated biomarker, new wall motion abnormality and elevated biomarker, or EKG findings and death. The sensitivities and specificities of each of the criteria can be seen in the table to the right. [8]
The modified criteria were more sensitive than both the weighted and unweighted original criteria (P< 0.001). The specificity of the modified criteria was greater than the unweighted original (P < 0.04), but not significantly different from the weighted original (P = 0.5). They conclude that the modified criteria are superior at identifying ACO.
Does this work in paced rhythms?
Right ventricular pacemakers produce a LBBB pattern on EKG because the electrical impulse is moving from right to left as it would if the left bundle was damaged. This should allow the use of the modified Sgarbossa criteria in a paced rhythm. Unfortunately, no studies have been published demonstrating this. Maloy et al. investigated the Sgarbossa criteria in 57 patients with ventricularly paced rhythms. They found that discordant ST elevation > 5mm was 10% sensitive, but 99% specific for ACO. ST segment depression > 1mm in V1-V3 was 19% sensitive and 81% specific. No EKGs in this study demonstrated concordant ST-segment elevation >1 mm. This study demonstrates that the Sgarbossa criteria are very specific for ACO in a ventricularly paced rhythm. Unfortunately, no studies have investigated the modified criteria in paced rhythms, but the concept of improved sensitivity with a ratio should still apply.
Limitations
The Sgarbossa criteria cannot be used in every situation, and their utility has some limitations. Smith et al. and the validation study by Meyers et al. excluded patients with hyperkalemia > 5.5, tachycardia > 130, hypertension with DBP > 120, and pulmonary edema with respiratory failure. [6,8] Smith notes in his study that wandering baseline and ectopic beats can cause errors in interpretation of ST/S ratios. It should be noted that all studies cited here are retrospective designs. Though there is some evidence for the use of the original Sgarbossa criteria in paced rhythms, no study has investigated the use of the modified criteria.
Conclusions
The modified, unweighted Sgarbossa criteria are highly specific, and fairly sensitive for acute coronary occlusion. Performance of these criteria is well validated. In patients with LBBB and symptoms of ischemia, intervention is warranted in those who are positive for any of the modified criteria. Acute coronary occlusion cannot be ruled out in patients who do not meet criteria, and they should receive further workup with serial EKGs, serial troponins, and non-invasive evaluation of ischemia.
Article by Logan Walsh, MD
Dr. Walsh is a rising PGY-2 in Emergency Medicine at the University of Cincinnati
Peer Editing and Post by Jimmy Summers, MD and Ryan LaFollette, MD
Dr. Summers is a graduating PGY-4 in Emergency Medicine at the University of Cincinnati. Dr. LaFollette is an Assistant Program Director at the University of Cincinnati
References
Go AS, Barron H V, Rundle AC, Ornato JP, Avins AL. Bundle-branch block and in-hospital mortality in acute myocardial infarction. National Registry of Myocardial Infarction 2 Investigators. Ann Intern Med. 1998;129(9):690-697. http://www.ncbi.nlm.nih.gov/pubmed/9841600.
Mozid AM, Mannakkara NN, Robinson NM, et al. Comparison of clinical characteristics and outcomes in patients with left bundle branch block versus ST-elevation myocardial infarction referred for primary percutaneous coronary intervention. Coron Artery Dis. 2015;26(1):17-21. doi:10.1097/MCA.0000000000000156
Sgarbossa ELB, PInski SEL, Barbagelata AL, et al. Electrocardiographic Diagnosis of Evolving Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block. N Engl J Med. 2002;334(14):931-931. doi:10.1056/nejm199604043341421
Tabas JA, Rodriguez RM, Seligman HK, Goldschlager NF. Electrocardiographic Criteria for Detecting Acute Myocardial Infarction in Patients With Left Bundle Branch Block: A Meta-analysis. Ann Emerg Med. 2008;52(4). doi:10.1016/j.annemergmed.2007.12.006
Mason JW, Hancock EW, Gettes LS. Recommendations for the Standardization and Interpretation of the Electrocardiogram. Circulation. 2007;115(10):1325-1332. doi:10.1161/CIRCULATIONAHA.106.180201
Smith SW, Dodd KW, Henry TD, Dvorak DM, Pearce LA. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified sgarbossa rule. Ann Emerg Med. 2012;60(6):766-776. doi:10.1016/j.annemergmed.2012.07.119
Cai Q, Mehta N, Sgarbossa EB, et al. The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? Am Heart J. 2013;166(3):409-413. doi:10.1016/j.ahj.2013.03.032
Pendell Meyers H, Limkakeng AT, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: A retrospective case-control study. Am Heart J. 2015;170(6):1255-1264. doi:10.1016/j.ahj.2015.09.005