More than a Sore Throat: Lemierre's Syndrome
/Throat pain is one of the most common chief complaints evaluated in many emergency departments across the country. While this is largely a minor medical complaint with no significant interventions required, there are a few life-threatening conditions that easily present as a throat pain. This article will address one of these life-threatening medical conditions: Infectious thrombophlebitis of the internal jugular vein commonly known as "Lemierre's Syndrome".
Before the advent of antibiotics, Lemierre's Syndrome was a common occurrence. With the use of antibiotics the occurrence rate is currently 1 in 1,000,000.
CASE
A 15 year-old male comes in with complaint of a sore throat for the past week. Mother states that the patient was seen at primary care provider’s office three days ago. They were told that he likely had a viral infection. Patient has become increasingly ill appearing, spiking fevers, and now has difficulty swallowing. Patient also states turning his head is making his sore throat worse.
Examination reveals a febrile young male temperature of 101.8 F, with tender right anterior cervical lymphadenopathy, erythema to the posterior pharynx, tonsillar enlargement on the right with exudate noted with uvula in the midline. There is asymmetry of the neck noted with mild swelling to the right compared to the left.
DISCUSSION
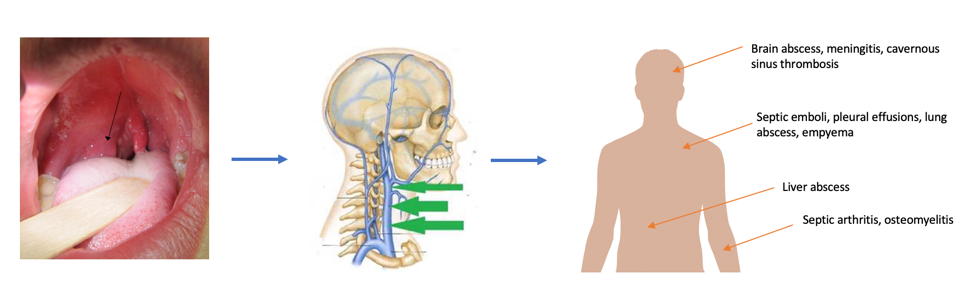
Clinically, these patients are usually more ill appearing than the more common viral sore throats. Common cause includes pharyngitis that has either been treated with antibiotics or at times been considered viral and symptomatically managed. Most of these patients will have a fever that is not responsive to antibiotic therapy. The spread of infection to involve the vasculature can be 5-7 days after the onset of pharyngitis. Prior to inflammation of the internal jugular vein, the initial insult is infection of the tonsils which progresses to involve the peritonsillar space and surrounding soft tissues.
The most common culprit is Fusobacterium necrophorum which is part of the normal microbial flora of the oropharynx. Anaerobic bacteria form an abscess and based on the duration of symptoms, the wall of the abscess can be penetrated which allows migration of the bacteria and their endotoxins.
With the proximity of the IJ to the posterior pharynx, inflammation secondary to the toxins can lead to development of prothrombotic conditions. Most of the signs for Lemierre's syndrome are nonspecific. Additional features include:
High fever
Rigors
Unilateral neck pain/swelling
Pleuritic chest pain
Dyspnea
Abdominal pain
Trismus
It is not uncommon for patients to present with the systemic septic findings which can mask the oropharyngeal symptoms.
Diagnosis
The diagnosis for Lemierre's syndrome is a highly clinical diagnosis. To confirm the presence of the condition in addition to the signs and symptoms listed above, a patient can have:
Anaerobic primary infection of the oropharynx
Positive blood culture (x1) to confirm septicemia
Metastatic infection of a distal site
Thrombophlebitis of the IJ
A CT scan of the neck is currently the best diagnostic modality to confirm soft tissue and vasculature involvement of the infection.
TREATMENT
As with every bacterial infection, prompt administration of antibiotics is necessary. Broad spectrum antibiotics such as Amp-Sulbactam (3g q6h) or Pip-Tazo (4.5g q6h) are preferred as they have beta-lactamase resistant coverage.
If the patient is hemodynamically stable and is able to tolerate a bedside I&D then drain any associated abscesses such as a peritonsillar abscess.
Regarding thrombophlebitis, there are no supportive studies or anti-coagulating these patients and the septic emboli are at risk of hemorrhage. It is rarely indicated.
Surgery is indicated at times when patients are failing antibiotic therapy. This is typically weeks later as the response to antibiotics takes time.