Grand Rounds Recap - 5/25
/M&M with Dr. Toth
Cryptogenic Strokes
30% of strokes have no ultimate cause determined. This is even higher for patient under the age of 55, but structural cardiac abnormalities and occult atrial fibrillation are still thought to play a significant role.
Septic Joints
The lifetime incidence of infection of a prosthetic joint is 0.5-2%. In the septic joint with an infection of unknown source, have a very low threshold to add imaging of a non-native joint to the broad workup for a source of infection. We already reflexively check the urine and chest xray of these patients, but at any point the joint may become infected and the exam is not sensitive for localization
Acute Ischemic Strokes
Multiple recent and ongoing trials suggest a benefit to many therapies beyond systemic administration of thrombolytics. These interventions include clot retrieval or directed intraarterial thrombolytics, and may be administered over a longer time frame than we are used to. Consider CT angiogram imaging, stroke team consultation, and possible intervention for large vessel occlusion with a normal non contrast head CT that fall outside of the traditional treatment window.
NSAIDs and renal function
Chronic NSAID use is correlated with decresase in renal function, particularly in patients who start with CKD. It is not part of a work flow, but before starting a long course of NSAIDs should have some assessment of their renal function. Anyone with a GFR < 60 should not be on a prolonged course of NSAIDs. The elderly are a particularly vulnerable population.
Calcium Channel Blocker Overdose
Amlodipine is heavily protein bound and not amenable to removal via traditional CRRT. The mainstay of treatment is supportive care with fluid resuscitation, calcium, and high dose insulin (1 U/kg bolus and then a drip at 1 U/kg/hr to up 10 U/kg/hr), and then vasopressors as needed. Intralipid and methylene blue are worth considering in a patient with refractory shock as they both have anecdotal evidence for support.
For more information on calcium channel blocker overdose, check out this podcast by Scott Weingart and Leon Gussow
Thyroid Storm
The diagnosis of this is aided by the Burch Wartofsky score scoring system, with a score > 45 highly suggestive of thyroid storm. This indicates a severe level of disease with a 10-30% mortality. The score is based on objective measurements of GI symptoms, vital sign derangements, and signs of end organ dysfunction (high output cardiac failure). Initial treatment is blocking the peripheral effects with beta blockers and steroids, blocking the release of thyroid hormone with iodine, and blocking hormone production with propylthiouracil or methimazole.
Chest CT with Dr. Colmer
See Dr. Colmer's post about Chest CT
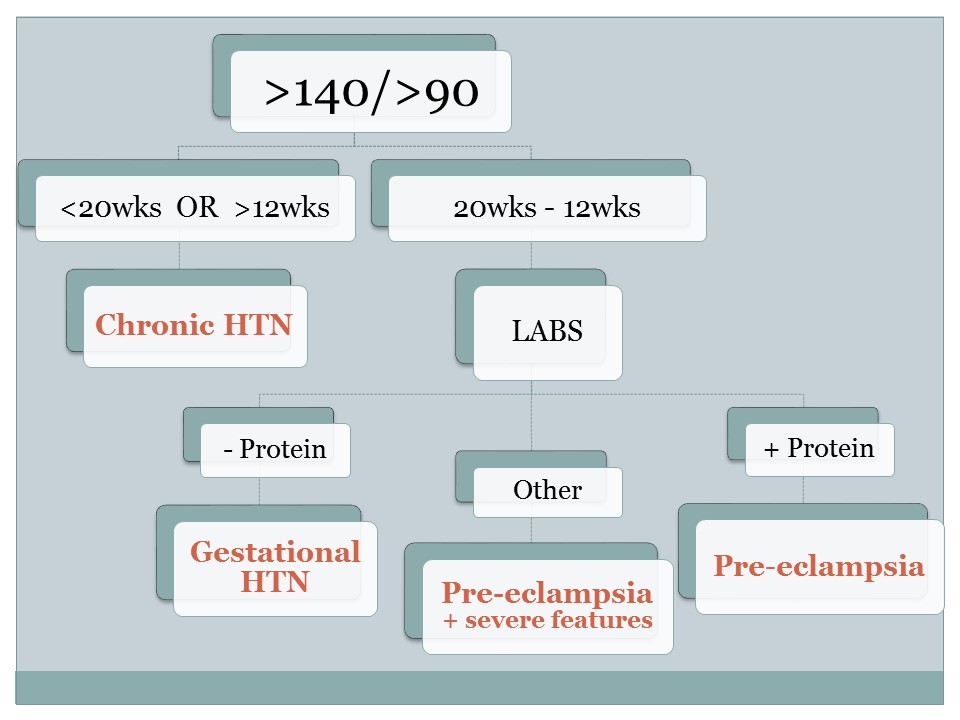
Pregnancy-Induced Hypertension with Dr. Bernardoni
The first step in treatment of hypertension of the pregnant patient is recognize it! Our ED demographic mostly lives in the 180s, but it is important and life saving once a pregnancy is identified
- BP >140/90 and 20wks gestation-12 weeks post-partum = labs
- BP >160/110 treat the hypertension
These patients are at risk of complications and pre-term delivery. Consider aspirin in high risk early pregnancy, it's the right thing for the patient even if not all OBs here are doing it. (Also most of these high risk patients will be followed by MFM who will prescribe aspirin)
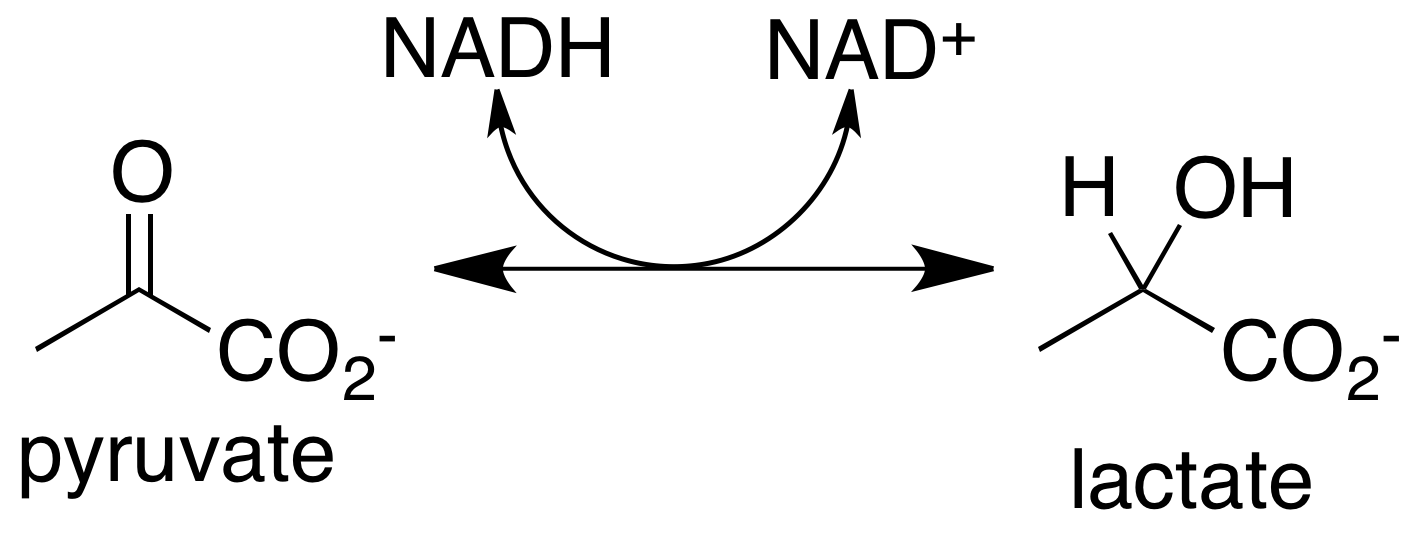
R4 Capstone with Dr. Betz - Demystifying lactate
Lactate is an organic compound formed by anaerobic metabolism as well as catecholamine and epinephrine surge from a "metabolically stressed state"
- A study by Shapiro et el 2005 showed that in patients presenting to the emergency department and admitted to the hospital with concern for infection, initial lactate in the ED > 4 has a 28d mortality of 28%. In this study patients admitted to the hospital with a normal lactate had a 28d mortality of 4.9%
- In patients with severe traumatic injury admitted to surgical ICU, initial lactate > 4.7 and lactate clearance of < 18% between 0 and 2h was associated with statistically significant increase in mortality. When normotensive patients were analyzed separately, neither lactate nor lactate clearance was predictive of mortality. Reignier et al, 2012.
- In a study by Dugas et al 2012, 20% of patients presenting with septic shock requiring vasopressors presented with a normal lactate. The mortality rate of this normal lactate group was 25%.
- Lactate has no evidence for predicting acute abdomen above clinical gestalt in patients presenting to the emergency department with abdominal pain and is neither sensitive nor specific for predicting mesenteric ischemia.
In summary, lactate does predict mortality admitted septic patients or trauma patients with severe mechanism of injury with initial lactates > 5, but it is unknown how much this additional lab value adds to the clinical picture. There is no evidence currently for using lactates in patients discharged from the emergency department.
Case Followup with Dr. Curry - Pediatric bleeding diatheses
- Pediatric bleeding diatheses can generally be thought of as either purpuric or coagulopathic.
- Purpuric bleeding disorders present as bleeding into the skin and mucous membranes whereas coagulation disorders present as bleeding into the soft tissue, muscles and joints
- The most common purpuric bleeding disorders in children are vonWillebrand’s disease and ITP
- The most common coagulopathic disorder is Hemophilia A or B
- ITP is now called Immune ThrombocytoPenia to indicate that it has an immune cause (rather than idiopathic) and that is is not always associated with purpura
- ITP can be acute or chronic. The acute form is most common in children aged 2-5 years, often results in profound thrombocytopenia (platelet counts <20) and more than 90% of cases end with spontaneous remission
- Not all cases of ITP require treatment. Some asymptomatic patients can be discharged with close follow-up and instructions on limiting activities that cause bleeding and, specifically, those that could result in head trauma
- IVIG or steroids (1mg/kg/day predisone) are both indicated for those cases requiring treatment. Each has their benefits and are indicated in certain scenarios, although there is wide practice pattern variation so get your hematology group involved early
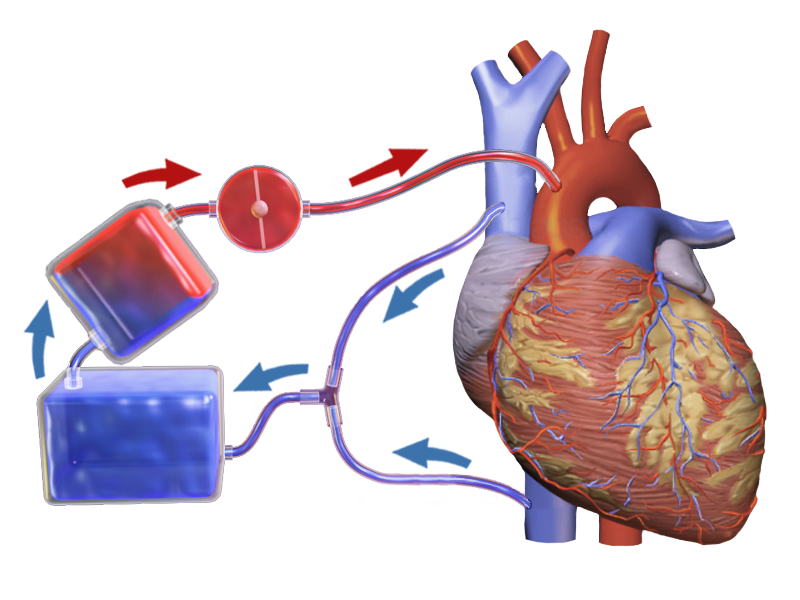
ECMO Fundamentals with Dr. Bonomo
Let's start with an ECMO Glossary
ECLS/ECMO -
- VA - primarily heart support
- VV - no cardiac support, pulmonary only
- VVA - both cardiac and pulmonary support
ECPR - Intra-arrest resuscitation (what we get pumped about)
VV ECMO / Pulmonary Support
- Candidacy contingent upon reversibility of the primary process (i.e. not your end stage COPD)
- Severe hypoxemia (P/F < 80) despite appropriately high PEEPs (15-20)
- Uncompensated hypercapnea with acidemia (<7.15)
- High plateau pressures despite ventilator strategies
Relative contradindications
- High pressure > 7 days (type II pneumocyte damage)
- High FiO2 > 7 days (type II pneumocyte damage)
- Limited vascular access (chest tube sized arterial cannulation is hard enough)
But does it work?
Peek et al. showed that regionalization and randomization to ECMO was efficacious in England with 63% vs 47% functional outcome at 6 months
18 patients were enrolled in the San Diego study, with 5/8 having neuro intact outcomes, large studies are needed and coming
ECPR (VA-ECMO) - Current indications UCMC
- Indications include young patients with refractory VFib/VTach arrest < 30 minutes
- Poisonings with cardiogenic shock
- Severe hypothermia with arrest
- Massive PE with arrest