Transient Synovitis or Septic Arthritis? Evaluating the Kocher Criteria
/When a child presents with atraumatic hip pain, the differential includes septic arthritis, transient synovitis, osteomyelitis, slipped capital femoral epiphysis, Legg- Calve-Perthes disease, juvenile idiopathic arthritis, acute rheumatic fever, post strep reactive arthritis, gonococcal arthritis, Henoch-Schoenlein purpura, sickle cell crisis, lyme arthritis, etc. The list is extensive. Fortunately, many of these complaints can be ruled out using a good history, physical exam, and basic laboratory/imaging tests. Two diagnoses, however, are notoriously hard to differentiate without an invasive procedure: septic arthritis and transient synovitis. Both present with an atraumatic, acutely irritable hip sometimes with associated limp, fever, refusal to bear weight, limited ROM, and/or joint effusion on x-ray and ultrasound. It is imperative to differentiate the two as the treatment and course of the two diseases are very different.
Septic arthritis most commonly affects children less than 3 years old and occurs when an organism invades the joint space and synovial fluid.
Clinical features may include acute onset of fever, joint pain, joint swelling, and limited range of motion, typically in a single joint. Early X-rays may be normal with late findings including joint effusion and distension.
Diagnosis is definitively made with an arthrocentesis that has a positive gram stain/culture or a high white blood cell count. The joint is treated with drainage and washout in the operating room with IV antibiotic administration. Septic arthritis commonly causes significant joint destruction but may also result in avascular necrosis, joint laxity or restriction, limb length discrepancy, and sepsis.
Transient Synovitis on the other hand is the most common cause of acute hip pain in children less than 10 years old. The cause is not always clear; however, it is often attributed to a viral illness. The joint pain occurs when the synovial membrane becomes inflamed and hypertrophies.
Common symptoms include unilateral hip pain, limp, and restricted range of motion due to pain from fluid accumulation in the joint. Imaging is inconclusive showing either normality or an effusion.
The diagnosis is made clinically after all other etiologies have been safely ruled out. Treatment includes NSAIDS, rest for 3-7 days until pain resolves, and re-evaluation in 2 weeks. Transient synovitis has a recurrence rate from 4-15%.
As you can see the clinical features and presentation of these two disease processes can be strikingly similar. So, how do we go about differentiating septic arthritis from transient synovitis?
Kocher Criteria
In 1999, Mininder S. Kocher, a pediatric orthopedic surgery fellow at Harvard, developed an interest in determining if there were certain variables of a child’s presentation that would allow for a more accurate differentiation of these two diseases. Dr. Kocher’s original paper was a retrospective review of 282 children from 1979-1996 who presented to the ED with complaints of an acutely irritable hip. (1) Kocher used univariate analysis and multiple logistic regression analysis to compare the two groups and then constructed and tested a probability algorithm using independent multivariate predictors.
He concluded there were four variables that could be combined to give good predictive probability of septic arthritis. These variables were later identified as the Kocher Criteria (Table 1).
Table 1: Kocher Criteria for Septic Arthritis
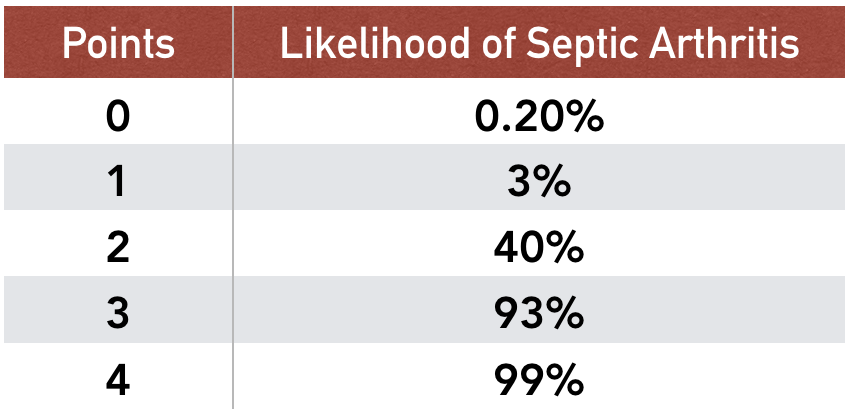
Table 2: Likelihood of Septic Arthritis with number of Kocher Criteria present. Based on data from Kocher and colleagues (1)
Each point is associated with a likelihood of the child having septic arthritis. Based on his paper, the likelihood of a child with 0 of the Kocher criteria having septic arthritis is 0.2%. This percentage increases with each additional point up to 99% likelihood at 4 points (Table 2).
What does everyone else think about the Kocher Criteria?
In 2004, the Kocher Criteria were prospectively validated at the same clinical site where the derivation of the criteria was performed. (2) In this validation study, the numbers changed a bit: Zero predictors: 2.0% risk, 1 predictor: 9.5%, 2 predictors: 35.0%, 3 predictors: 72.8%, 4 predictors: 93.0%.
Also in 2004, Luhman and colleagues performed a retrospective review of the 4 Kocher Criteria at a different institution and found the predicted probability of the patient having septic arthritis to be only 59% compared to Kocher’s 99.6%. (3) The paper found that the best predictors of septic arthritis were history of fever, WBC > 12,000, and a previous health care visit giving a predicted probability of 71%.
In 2006, Caird and colleagues prospectively investigated CRP levels in children for whom joint aspiration was performed. (4) They found that a CRP greater than or equal to 20 mg/L, as well as the Kocher criteria being present had a predicted probability of 98%. Their cohort of patients, however, included only 12 patients with an end diagnosis of transient synovitis. Caird and his colleagues found that fever was the best predictor of a septic joint followed closely by CRP. Singhal and colleagues looked more extensively at CRP’s role in the differentiation of the two diseases and found that CRP > 20 mg/L was the best independent predictor of a child having septic arthritis. (5) This combined with the child’s weight bearing status were able to differentiate septic arthritis from transient synovitis. With both absent, the patient had a <1% chance of having septic arthritis.
In 2010, Sultan and colleagues performed a retrospective study of Kocher’s Criteria with the addition of CRP. (6) They found that the predicted probability of septic arthritis when all 5 criteria were present was only 59.9% compared to Kocher’s 99.6%. They also found that if all 5 criteria were absent, the patient did not have septic arthritis. Notably, this study, unlike the three previously mentioned studies, did not take place at a tertiary referral center and had a much lower prevalence of septic arthritis. The authors hypothesized that the variables were less predictive in a population with a lower prevalence of disease. They also found that fever was the best predictor overall for a septic joint.
What does all this mean?
Investigators at many different institutions have not been able to agree on which criteria are the most predictive of a septic joint. There has yet to be a high quality and affirmative external validation of the Kocher Criteria. The positive predictive value of the Kocher criteria depends on the prevalence of disease with lower positive predictive value with lower prevalence of disease. Most importantly, absence of all 5 criteria (Kocher Criteria + CRP) confers a very low probability of having septic arthritis.
SUMMARY
A detailed history and physical exam are critical in the assessment of pediatric hip pain. Subsequent investigations including laboratory and imaging studies should be guided by your pre-test probability of septic arthritis. The Kocher criteria, especially when used in conjunction with CRP, can help guide the need for arthrocentesis and consultation of orthopedic surgery however the positive predictive value of the criteria is variable.
Ultimately, a patient with 0 of 4 Kocher criteria, a negative CRP, and a low pre-test probability of septic arthritis can reasonably be managed as an outpatient with NSAIDS and strict return precautions for worsening hip pain and/or fever. Increasing uncertainty, either by history and/or the presence of Kocher criteria, mandates the need for further investigation with arthrocentesis and/or consultation with orthopedics as misdiagnosis of septic arthritis can have dire consequences.
References
Kocher MS, Zurakowski D, Kasser JR (1999). "Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm". J Bone Joint Surg Am. 81 (12): 1662–70.
Kocher MS, Mandiga, R, Zurakowski D, Barnewolt C, Kasser JR (2004). “Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children”. J Bone Joint Surg Am. 86A (8):1629-35.
Luhmann SJ, Jones A, Schootman M, Gordon JE, Schoenecker PL, Luhmann JD (2004). “Differentiation between septic arthritis and transient synovitis of the hip in children with clinical prediction algorithms”. J Bone and Joint Surg. 86(5):956-962.
Caird MS, Flynn JM, Leung YL, Millman JE, D’Italia JG, Dormans JP (2006). “Factors distinguishing septic arthritis from transient synovitis of the hip in children. A prospective study”. J Bone Joint Surg Am. 88 (6): 1251-7.
Singhal R, Perry DC, Khan FN, Cohen D, Stevenson HL, James LA, Sampath JS, Bruce CE (2011). “The use of CRP within a clinical prediction algorithm for the differentiation of septic arthritis and transient synovitis in children”. J Bone Joint Surg Br. 93(11): 1556-61.
Sultan J, Hughes PJ (2010). “Septic arthritis or transient synovitis of the hip in children; the value of clinical prediction algorithms”. The Bone and Joint Journal. 92B (9):1289-93.
Goldenberg DL, Sexton DJ. Septic arthritis in adults. In: UpToDate, Calderwood SB (Ed), UpToDate, Waltham, MA, 2018.
Klein-Gitelman M. Joint aspiration or injection in children: indications, technique, and complications. In: UpToDate, Sundel R (Ed), UpToDate, Waltham, MA, 2018.
Tintinalli JE, Stapczynski JS, Ma OJ, Yealy DM, Meckler GD, Cline DM. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 8th ed. New York, N.Y.: McGraw-Hill Education LLC., 2016: (929-934).
Zamzam MM (2006). “The role of ultrasound in differentiating septic arthritis from transient synovitis of the hip in children.” Journal Pediatric Orthopedic B. 15(6): 418-22.
Written by: Payton Leach, MD, PGY-1 University of Cincinnati Department of Emergency Medicine
Peer Review and Editing: Jeffery Hill, MD MEd