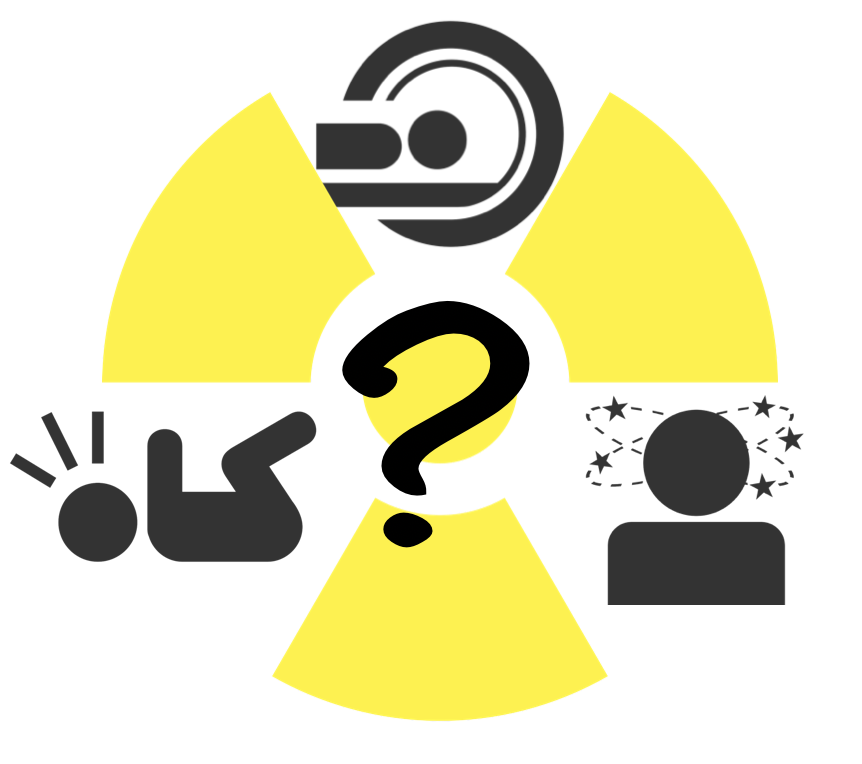
To Scan or Not to Scan? PECARN for Pediatric Head Trauma.
/What are the Key Takeaways from this Article?
The Pediatric Emergency Care Applied Research Network (PECARN) head trauma clinical decision tool has been validated numerous times by external studies and has repeatedly been shown to have a sensitivity nearing 100% for clinically significant TBI when any of the six factors are present. The Children’s Head injury Algorithm for the prediction of Important Clinical Events (CHALICE) and The Canadian Assessment of Tomography for Childhood Head Injury (CATCH)are similar clinical predictor tools to PECARN, however both have a more limited age range (< 16 years old), lower sensitivity than PECARN, and are not as widely validated as PECARN. A thorough history and physical should be performed on every child presenting after head trauma and physician gestalt should never be disregarded. However, the PECARN clinical prediction tool has impressive sensitivity and NPV which has been repeatedly externally validated. Therefore, physicians can be reassured that patients classified as ‘low risk’ can safely forego a head CT with a very low risk of missing a clinically significant TBI.
PECARN Clinical Prediction Tool
The Pediatric Emergency Care Applied Research Network (PECARN) is a research collaboration of pediatric emergency departments across the U.S. which was established in 2001. In 2009 PECARN derived and validated two clinical predictions rules (one for children <2 years old and one for children 2-18 years old) for children who present within 24 hours of head trauma with an initial Glasgow Coma Score (GCS) of 14-15 (3). Their goal was to identify child at very low risk of a clinically significant TBI in whom head CT may be unnecessary. Clinically significant TBI was defined as follows:
Death from TBI
Neurosurgical intervention due to TBI
Intubation for >24 hours for TBI
Hospital admission of 2+ nights for TBI in association with TBI on CT
This was a multicenter prospective cohort study involving 42,412 patients (33,785 in the derivation cohort and 8627 in the validation cohort). Patients who presented with trivial injury mechanisms, penetrating head trauma, known brain tumors, pre-existing neurological disorders, or patient's with neuroimaging from an outside hospital were excluded from the study (3).
The predictors derived for the two groups were as follows:
Table 1: Predictors of Clinically significant TBI in pediatric patients
For children under 2 years of age with zero of the six predictors, the risk of clinically significant TBI was less than 0.02%, and no child classified as low risk (n=1175) had a clinically significant TBI, ultimately demonstrating a sensitivity of 100% and an NPV of 100% (3).
For children aged 2-18yo with zero of the six predictors, the risk of clinically significant TBI was less than 0.05%. 2 of 3698 with no risk factors ended up having a clinically significant TBI, giving this prediction rule a sensitivity of 96.8% and an NPV of 99.95% (3).
Further analysis for risk of TBI based on the presence of individual predictors demonstrated the following:
Table 2: Risk of clinically significant TBI in children less than 2 years of age based on predictor.
Table 3: Risk of clinically significant TBI in children aged 2 years old to 18 years old based on predictor
This allowed them to stratify patients into a high risk group, a moderate risk group, and a low risk group. From this the following recommendations came to be:
- Those in the high risk group should Receive a Head CT
- Those in the low risk group do not need a CT
- Those in the moderate risk group should either undergo CT or a period of observation, with the ultimate decision resting on other factors such as clinician judgement and shared decision making
What other tools exist for head trauma in pediatric patients?
The Canadian Assessment of Tomography for Childhood Head Injury (CATCH) rule is another clinical decision tool for pediatric head traumas. This study enrolled a total of 3866 aged 16 years old and under. The studied included those who presented within 24 hours of head trauma with a GCS ≥ 13 and at least one of the following: blunt head trauma with witnessed LOC, definite amnesia, disorientation, two or more episodes of vomiting at least 15 minutes apart, persistent irritability in children under the age of 2 years. The study excluded those patients with a penetrating skull injury, depressed fractures, focal neurological deficits, chronic general developmental delay, suspected child abuse, pregnant patients, or those returning for re-evaluation after having a previous head injury. The primary outcome of the study was neurologic intervention defined as any of the following within 7 days: Death from head injury, craniotomy, elevation of skull fracture, monitoring of intracranial pressure, or intubation after head injury (4). The predictors that were evaluated by this study are as follows:
Table 4: CATCH High Risk and Moderate Risk Predictors for clinically significant TBI
The high risk factors were 100% sensitive for predicting the need for neurological intervention, while the presence of any of the risk factors were 98.1% for the prediction of brain injury on CT (4).
Another tool is the Children’s Head injury Algorithm for the prediction of Important Clinical Events (CHALICE) rule. This was derived from a prospective multicenter diagnostic cohort study which enrolled 22,772 children aged 16 or younger. Inclusion criteria were broad and encompassed any patient aged 16 years or younger with a history or signs of head injury. It did not require LOC for inclusion and was not limited to those with ‘mild’ head injury, meaning those with head injuries considered moderate or even severe were included. Primary outcomes included death from head injury, requirement for neurosurgical intervention, or marked abnormalities on head CT (5). The predictors evaluated are as follows:
CHALICE demonstrated a sensitivity of 98% and a specificity of 87% for the prediction of clinically significant head injury when any 1 of the evaluated factors was present (5).
What does everyone else think about these tools?
In 2014, Schonfeld et. alexternally validated the PECARN traumatic brain injury clinical prediction rule in a cross sectional study performed at two pediatric emergency departments, one in the U.S. and one in Italy. This study included 2439 children, all of whom presented to the ED within 24 hours of head injury with a GCS of 14 or 15. They found that none of the children with a clinically important TBI were classified as very low risk by the PERCAN TBI prediction rule. Furthermore, their study demonstrates the PECARN TBI prediction rule had an overall sensitivity of 100%, a specificity of 55%, and a negative predictive value of 100% (6).
Also in 2014, a study conducted by Easter et. alin the Annals of Emergency Medicine evaluated the diagnostic accuracy of 3 decision rules: PECARN, CATCH, and CHALICE, focusing on the performance of the low risk criteria for each tool. Furthermore, they assessed the diagnostic accuracy of 2 measures of physician judgment: physician estimated <1% risk of TBI, and physician head CT ordering practices. It was a prospective cohort study of 1009 children under the age of 18 who presented within 24 hours of head trauma with a GCS of 13-15. The study was conducted at a single level II trauma pediatric emergency department in Denver, CO. The prediction tools were assessed for accuracy in predicting clinically important TBIs defined as death from TBI, need for neurosurgery, intubation for more than 24 hours due to TBI, or hospitalization for more than 2 days due to TBI. The results of this study can be seen in table 5. Of the five modalities (PECARN, CHALICE, CATCH, Physician judgment, Physician CT practices) only physician judgment and PECARN identified all clinically important TBI (7).
Table 5: Comparison of prediction tools for predicting TBI in pediatric patients, adapted from Easter et. al 2014.
In 2016, Lorton et alset out to validate the PECARN clinical decision rule for children with minor head trauma. They conducted a multicenter, prospective cohort study across three emergency departments in France. The study included 1499 children under the age of 16 who presented to the emergency department within 24hours of head trauma with a GCS of either 14 or 15. This study found a sensitivity of 100%, specificity of 69.9%, and an NPV of 100% (8).
In 2017 a prospective cohort study by Babl et alevaluated the accuracy of PECARN, CATCH, and CHALICE. The study enrolled 20,137 children under the age of 18 years old who presented with a head injury of any severity. They assessed the diagnostic accuracy of these three decision rules to predict a clinically important TBI as defined by PECARN.CHALICE was applicable to 99% of the patients included in the studied, PECARN was applicable to 75-76% (depending on age), and CATCH was applicable only to 25% of patients. Of these tools, PECARN had the highest sensitivity with 100% and 99.0% in children 2 years and under, and 2-18 years old respectively. CATCH had a sensitivity of 95.2%, and CHALICE had a sensitivity of 92.3% (9).
References
Faul M, Xu L, Wald MM, et al.Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002–2006. 2010.Atlanta, Ga.: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control.
Brenner, David J., et al."Estimated risks of radiation-induced fatal cancer from pediatric CT." American journal of roentgenology 176.2 (2001): 289-296.
Kuppermann, Nathan, et al."Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study." The Lancet 374.9696 (2009): 1160-1170.
Osmond, Martin H., et al."CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury." Canadian Medical Association Journal 182.4 (2010): 341-348.
Dunning, J., et al. "Derivation of the children’s head injury algorithm for the prediction of important clinical events decision rule for head injury in children." Archives of disease in childhood 91.11 (2006): 885-891.
Schonfeld, Deborah, et al. "Pediatric Emergency Care Applied Research Network head injury clinical prediction rules are reliable in practice." Archives of disease in childhood 99.5 (2014): 427-431.
Easter, Joshua S., et al. "Comparison of PECARN, CATCH, and CHALICE rules for children with minor head injury: a prospective cohort study." Annals of emergency medicine 64.2 (2014): 145-152.
Lorton, F., et al."Validation of the PECARN clinical decision rule for children with minor head trauma: a French multicenter prospective study." Scandinavian journal of trauma, resuscitation and emergency medicine 24.1 (2016): 98.
Babl, Franz E., et al. "Accuracy of PECARN, CATCH, and CHALICE head injury decision rules in children: a prospective cohort study." The Lancet 389.10087 (2017): 2393-2402
Written by Meaghan Frederick, MD, PGY-1, University of Cincinnati Dept of Emergency Medicine
Peer Review/Editing/Posting: Jeffery Hill, MD MEd, Associate Professor, University of Cincinnati Department of Emergency Medicine