Liquid Plasma aka "Never Frozen Plasma"
/I recently had the pleasure of sitting down with my co-EMS fellow, Dr. Ryan Gerecht, to discuss his experience with the implementation of a new blood product on our HEMS service: Liquid Plasma. Ryan was responsible for this implementation while serving as a Resident Assistant Medical Director during his last year of EM training at UC (2013-2014).
Here is what Ryan has to say…
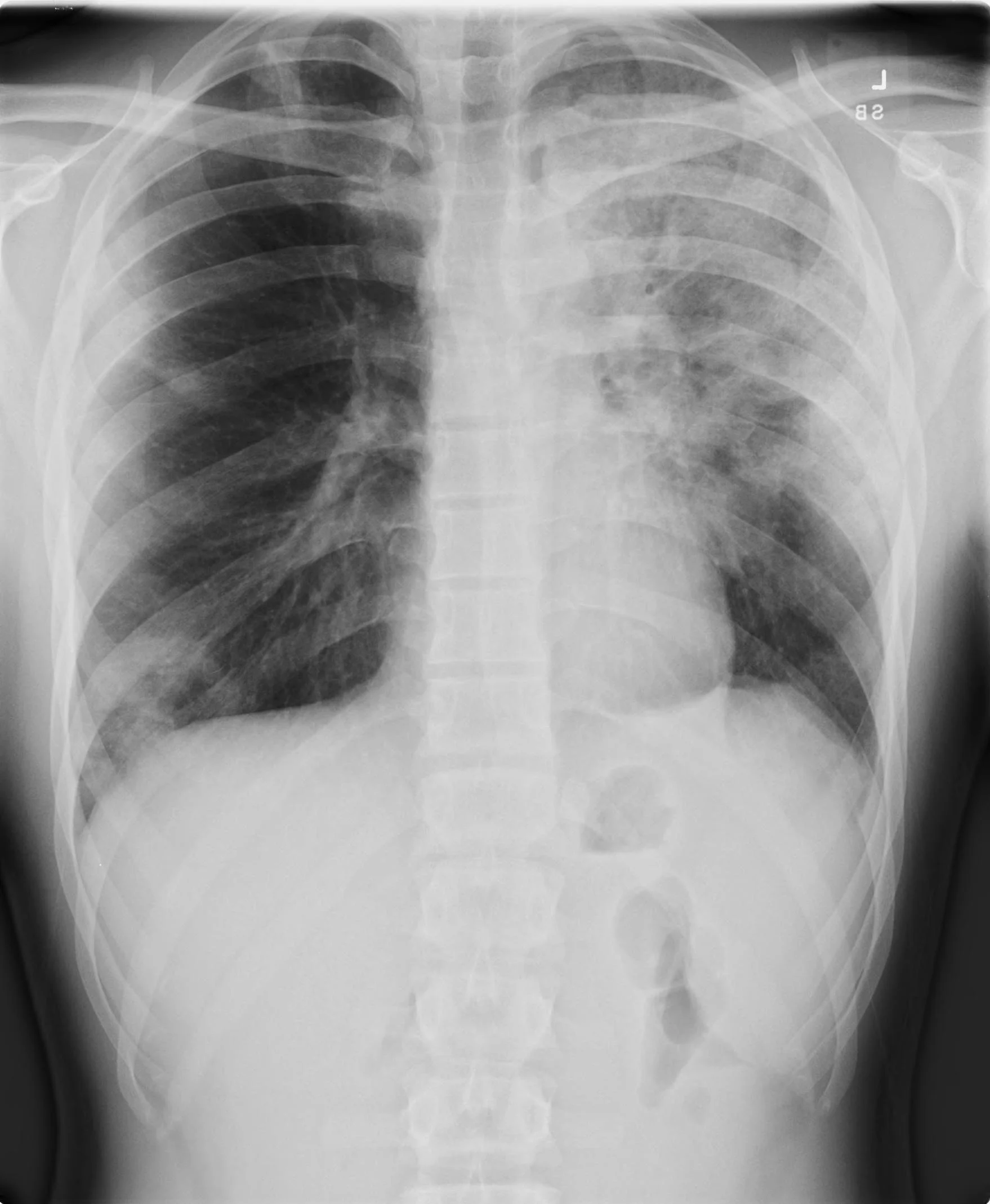
In the Emergency Department, ICU, or operating room what do you resuscitate the hemodynamically unstable, bleeding trauma patient with? What about the patient with a massive GI bleed or ruptured AAA? How do you manage the patient with an intracerebral hemorrhage on Coumadin? (assuming you don’t have PCC’s readily available)
Read More