Introduction to Emergency Medical Services
The University of Cincinnati Emergency Medicine Residency was the first Emergency Medicine Residency program. We carry a strong legacy in excellent clinical and leadership training. The Division of EMS has hosted an EMS Fellowship since 1996 and obtained full accreditation by ACGME in 2013, the first year it was offered. Residents have many educational experiences and leadership opportunities. This Introduction to EMS is meant to make you aware of the opportunities our program offers and to give you basic introductory knowledge about EMS.
Longitudinal EMS Curriculum
PGY-1 Gain exposure to ground EMS during ride-along shifts with Cincinnati Fire Department. This is a great way to experience the culture of our prehospital colleagues and learn from them. Taking care of patients in these settings is very different than the Emergency Department and the paramedics and EMT’s love having a physician around as well. You will also begin orientation flights on Air Care.
PGY-2 You are now an official flight physician! Air Care transports critically ill and injured patients through scene calls and interfacility transports. Our Air Care nurses and pilots are awesome partners and you will have the chance to experience clinical autonomy while providing critical care in the prehospital setting.
PGY-3 Provide online Medical Control for Southwest Ohio in between resuscitating critically ill patients in the SRU and seeing A-Pod patients. Our paramedic and EMT colleagues appreciate your advice and guidance when they have questions. Continue flying as a flight physician with Air Care and mastering critical care in the prehospital setting.
PGY-4 Consider using some of your elective time on EMS activities. Our program values leadership and provides mentorship and resources to complete projects. If you enjoyed your EMS experiences, consider applying for an EMS Fellowship.
Additional EMS Opportunities
EMS Elective
A dedicated two week dive into EMS. Ride with ground EMS supervisors, attend administrative meetings, join EMS fellow didactics, experience dispatch, and more. You will also complete the Ohio ACEP EMS Medical Director course.
Assistant Resident Medical Director
The Division of EMS provides medical direction to over 30 departments in our local community. Team up with faculty and senior residents to provide education to members of these departments. It is also possible to get involved with operations, quality improvement, and protocol development. They are always welcoming and happy to have you ride along.
Tactical EMS
Train and go on SWAT activations with Cincinnati Police Department SWAT Team. Stay fit, obtain weapons training, and provide medical care in a tactical EMS environment.
FOAMed
TamingtheSRU.com is our program’s FOAMed resource. We encourage residents to author and edit articles that are published and shared with the world. The Air Care Series is focused on critical care patient transport and explores topics such as cardiogenic shock, ARDS, ECMO, stroke, trauma, and more!
Research
Our faculty are active in EMS research and create multiple publications every year. Consider joining a project and producing scholarly activity.
Education and Simulation The Division of EMS has a simulation center and a simulation vehicle with state-of-the-art equipment. There are opportunities to provide continuing education to local community emergency department staff and fire departments. Our department plays a large role in medical school education. First year medical students go through a first responder course taught by our faculty, residents, and advanced practice providers. There are also opportunities to teach disaster medicine through tabletop exercises for third year medical students.
Event Medicine
Navigate large crowds and coordinate medical care for ill athletes and observers at sporting events such as the American Heart Association Heart Mini, Flying Pig Marathon, or Western & Southern Open tennis tournament.
History of EMS
Learning Objectives
Review the origins of modern EMS
Understand why EMS developed in the United States
Reflect on the role of EMS experiences in emergency medicine training
Beginning of Modern EMS
Humans have cared for the injured throughout the entirety of human history. There are references to triage and care of the injured through multiple civilizations. During the Napoleonic Wars, Napolean’s chief military physician, Jean Dominique Larrey, is often cited as the root of modern prehospital medical care. He created a system where injured soldiers were initially treated on the battlefield and then transported off site by ambulance volantes (“flying ambulances”).
The Civil War was the beginning of US emergency medical services (EMS) system development. Joseph Barnes and Jonathan Letterman were Union military physicians who built upon Larrey’s work. The Union army trained medical corpsman to provide medical care in the field. In addition to ambulances, railroads were used to transport the injured to medical facilities.
The first hospital based ambulance was based out of Commercial Hospital in Cincinnati, Ohio in 1865. Bellevue Hospital in New York City shortly followed in 1869. As technology evolved, electric, gas, and steam powered carriages began to be used as ambulances and mobile radios began to be used for dispatch. Unfortunately, there was still a large number of poorly trained and poorly equipped units and there was very little regulation of ambulance services.
“Neglected Disease of Modern Society”
In 1966, President Lyndon B. Johnson received a report from the National Academy of Sciences National Research Council titled “Accidental Death and Disability: The Neglected Disease of Modern Society”. This is commonly known as “the White Paper” and it pointed out that the US had an epidemic of traumatic injuries and lacked appropriate prehospital resources to treat these patients. It is considered the catalyst of improving EMS care in the US.
The Highway Safety Act was passed which led to the creation of the Department of Transportation. DOT was given the responsibility to help improve EMS and provided funding as well. The 1970s was a period of rapid growth and recognition for EMS. In 1972, the US Department of Labor recognized Emergency Medical Technician (EMT) as an official occupation. The EMS Systems Act of 1973 provided federal funding to develop regional EMS systems and approximately 300 programs were established and eligible for funding. The television show Emergency! portrayed prehospital care by paramedics showed Americans the type of advanced prehospital care while also encouraging people to pursue a career in this field.
In 1981, the Omnibus Budget Reconciliation Act was signed which eliminated direct federal funding of EMS systems and transitioned funds to be given to states in block grants. This led to decreased funding and coordination among EMS systems which resulted in great variation among EMS systems throughout the country.
In 2006, the Institute of Medicine (IOM) published a report titled “The Future of Emergency Care in the United States Health System” which highlighted the fragmented and poorly funded state of EMS.
Emergency Medicine and EMS
EMS is a required in the curriculum of emergency medicine residency training programs in the United States. The American Board of Medical Specialties recognized EMS as an official subspecialty in 2010. The core content areas include clinical aspects of EMS medicine, medical oversight of EMS, quality management and research, and special operations. Emergency medicine is well equipped to help address the problems identified by the IOM report.
Resources:
“A Brief History of Emergency Medical Services in the United States.” EMRA, www.emra.org/about-emra/history/ems-history/.
“Chapter 1 Emergency Medical Services.” Tintinalli's Emergency Medicine: a Comprehensive Study Guide, by J. Stapczynski, McGraw-Hill Medical Publishing Division, 2015.
“Chapter 190 Emergency Medical Services: Overview and Ground Transport.” Rosen's Emergency Medicine: Concepts and Clinical Practice, by Ron M. Walls et al., Elsevier, 2018.
“Chapter 1: History of EMS.” Emergency Medical Services: Clinical Practice and Systems Oversight, by David C. Cone et al., John Wiley & Sons Inc., 2015.
Edgerly, Dennis. “Birth of EMS: The History of the Paramedic.” JEMS, 2 Sept. 2019, www.jems.com/2013/10/08/birth-ems-history-paramedic/.
“The History of the National Registry and EMS in the United States.” National Registry of EMTs, www.nremt.org/rwd/public/document/history.
“IOM Report: The Future of Emergency Care in the United States Health System.” Academic Emergency Medicine, vol. 13, no. 10, 2006, pp. 1081–1085., doi:10.1197/j.aem.2006.07.011.
EMS Providers
Learning Objectives:
Review general capabilities of different EMS providers
Understand that scope of practice can vary depending on local protocol
Scope of Practice:
The National Highway and Traffic Safety Administration (NHTSA) provides guidelines and standards for the scope of practice of different prehospital certification levels. Individual states provides legislation that determines which provider levels are used in the state and their respective scopes of practice. States also determine CME requirements, recertification timelines, and other administrative requirements.
The National EMS Scope of Practice Model by the NHTSA was created because there was a need to streamline and standardize EMS provider levels. In 1996, there was at more than 40 different levels of EMS provider certification in the United States. In addition to public and professional confusion, it made it difficult for reciprocity of certification between states which led to decreased professional motility. They set levels of certification of prehospital providers and recommended skills.
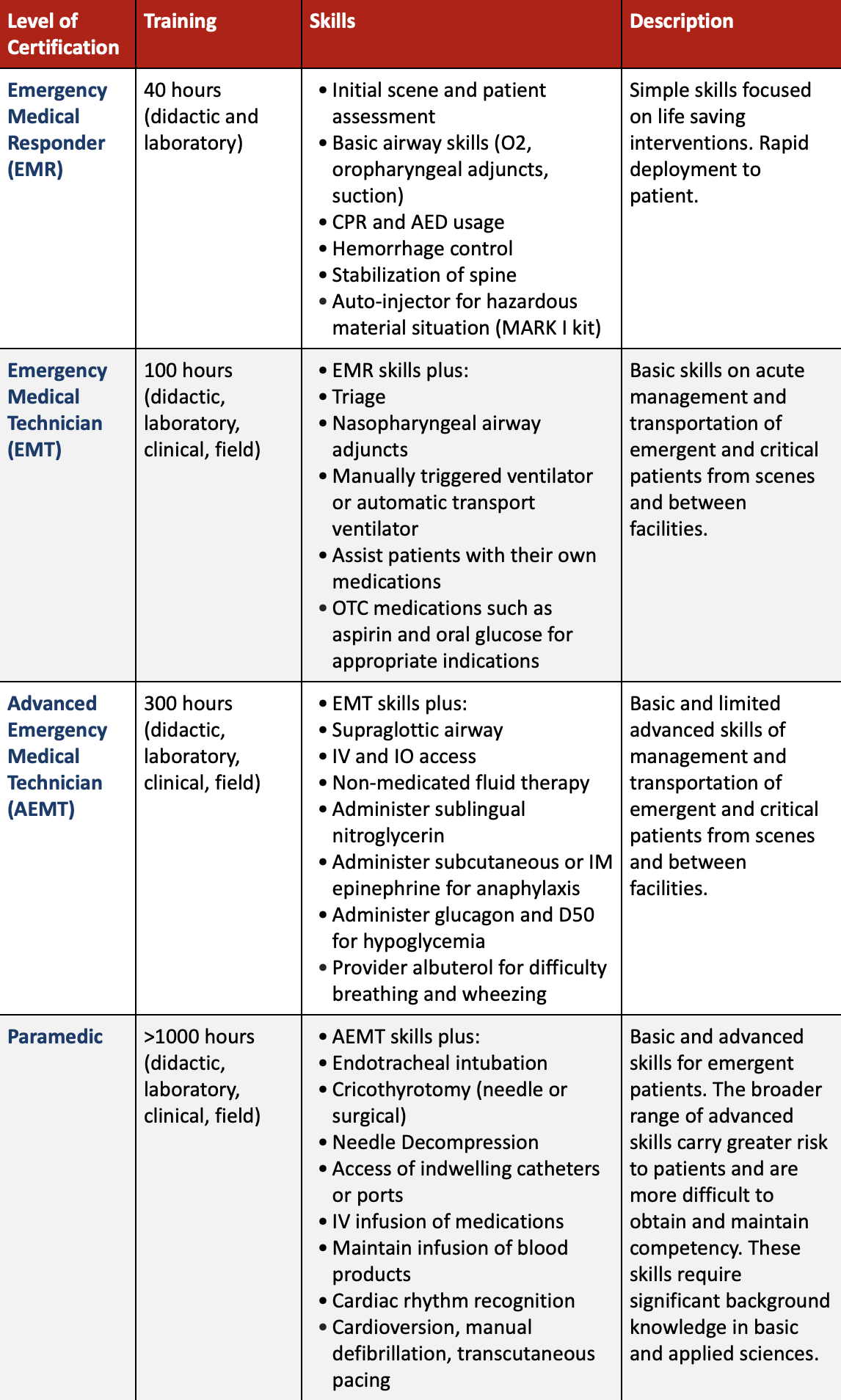
This table shows approximate training time and example of skills at each certification level. The scope of practice and personnel levels will vary state by state. The protocols will also vary among each EMS system to best serve their local communities.
Other Healthcare Workers in EMS:
It is important to note that physicians, nurses, and advanced practice providers may also work in the prehospital setting. Many helicopter EMS or ICU level ground transport utilize registered nurses as part of the transport team. In our program, resident physicians and nurse practitioners fly with Air Care. Many other countries utilize physicians in the prehospital setting more than the United States currently does.
Resources:
“Chapter 1 Emergency Medical Services.” Tintinalli's Emergency Medicine: a Comprehensive Study Guide, by J. Stapczynski, McGraw-Hill Medical Publishing Division, 2015.
“Chapter 190 Emergency Medical Services: Overview and Ground Transport.” Rosen's Emergency Medicine: Concepts and Clinical Practice, by Ron M. Walls et al., Elsevier, 2018.
National Highway Traffic Safety Administration. "National EMS scope of practice model." DOT HS 810 (2007): 657. (https://www.ems.gov/pdf/education/EMS-Education-for-the-Future-A-SystemsApproach/National_EMS_Scope_Practice_Model.pdf)
Medical Direction
Learning Objectives:
Review the role of medical director
Differentiate between indirect and direct medical oversight
Medical direction is recognized as an essential component of any EMS system. In the EMS Systems Act of 1973, there was no reference for the need for medical direction. Regardless, medical direction became a standard for advanced life support systems. In 1988, the National Highway Traffic Safety Administration made EMS medical direction one of ten essential components for state assessments. Through national groups such as the National Association of EMS Physicians and the American College of Emergency Physicians, the role of the EMS medical director has become more clearly defined.
Medical Director
A medical director is usually a physician with emergency medicine and EMS training. However, state laws and regulations affect the role of medical director. Generally, a medical director will have board certification, a state medical license, understanding of state/regional EMS operations, and experience with all components of an EMS system. Medical directors are usually required to be involved with education, quality assurance, protocol development, and more.
Indirect Medical Oversight
This is also be referred to as “offline medical direction”. The majority of work for an EMS medical director is indirect medical oversight. This is how a medical director shapes prehospital care in their system. Medical directors will often work with multiple agencies in fields such as healthcare and public safety.
EMS provider education is an important aspect of indirect medical oversight. There are educational requirements for EMS providers to maintain certification. There is quality assurance and process improvement work to ensure clinical skills are retained and kept up to date. Assessing competency of these skills and having the authority in the credentialing process are important for a medical director.
The medical director is essential towards assessing and improving an EMS system through field clinical supervision, review of runs on an electronic medical record, and access to hospital records to evaluate patient outcomes. Conducting or reviewing research can also aid in protocol development for patient care and for transport to specialty centers. Most of the EMS agencies in our area use the Southwest Ohio Protocol.
Direct Medical Oversight
This is also called “online medical direction”. Think of it as real time medical decisions and guidance. At our program, the third year residents carry a telemetry phone. EMS in the Southwest Ohio region can call this phone at any time to ask clinical questions or obtain permission to provide treatment that deviate from established protocol. The online medical direction physician should be experienced in emergency medicine and understand the EMS protocols.
In some cases, direct medical oversight can also happen on scene. The physician can gain valuable prehospital experience while also conduct ‘bedside’ teaching. If needed, physicians can provide direct patient care in the field for more advanced procedures or rare clinical scenarios that are beyond the scope of the EMS providers.
Resources:
“Chapter 8: Medical Oversight of EMS Systems.” Emergency Medical Services: Clinical Practice and Systems Oversight, by David C. Cone et al., John Wiley & Sons Inc., 2015.
James Li, MD