Background
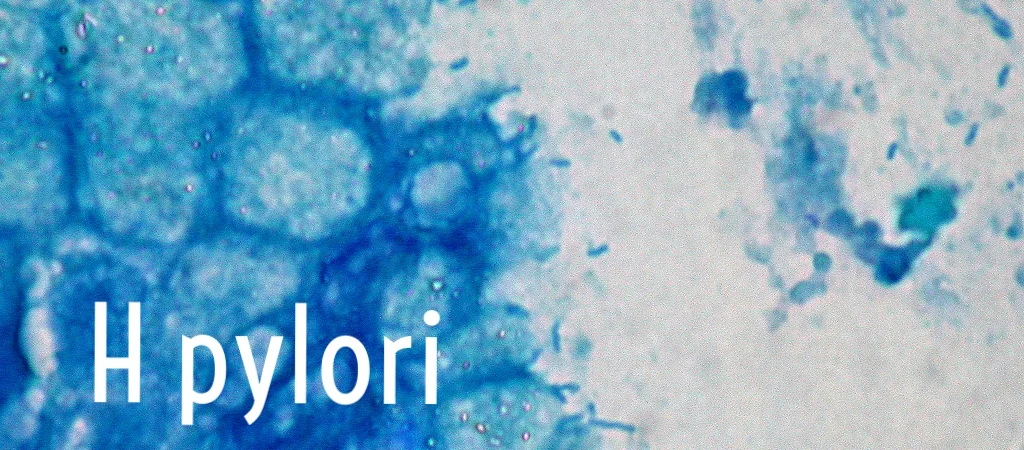
US - The Helicobacter pylori prevalence in the US is estimated to be 32% with a disproportionate amount affecting low income African Americans and Whites. Infection, transmitted the fecal-oral route, increases risk for both gastric and duodenal ulcers, gastric lymphoma and cancer, and GI bleeding. In a prospective cohort of over 80,000 patients in the Southern Community Cohort Study (across 12 states in the South East), serum studies were performed indicating that 89% of low income African Americans and 69% of low income whites were infected or had previously been infected with H pylori (serology testing doesn’t necessarily indicate active infection). Odds ratio for African Americans to be infected compared to Whites was 3.5. This inverse association with socioeconomic status and H pylori infection has been replicated across studies and is likely reflected in our EDs.
Developing Countries - H pylori affects approximately 50% of the world’s population. That is an estimated 3.5 billion people, with prevalence average 60% in Central America and reaching as high as 90% in many parts of Africa and Asia. Some experts purport that the only way to address it large scale is by creating vaccines, which are currently under investigation.
Current guidelines
American College of GI (updated 2005)
- In populations where H pylori is >10%, test and treat is preferable to empirical PPI.
- Logic would carry that when practicing internationally, test and treat given the high disease burden
- If patient is failing a PPI, use Urea Breath Testing (UBT) before endoscopy
- In populations with high H pylori prevalence, 40% of patients positive via UBT had duodenal ulcers and only 2% negative via UBT had ulcers
- Level of evidence for empiric PPI and 'Test and Treat' are both level A
- 'Test and Treat' is cost effective vs PPI with endoscopy
Note that serologic testing is, in general, a poor option as it has lower sensitivity and may remain positive after the patient has cleared any active infection
Treatment
Eradication of Helicobacter pylori is associated with healing of ulcers as well as decreased risk of future ulcers and healing. Meltzer et al recently studied the utility of the C13 Urease breath test out of the emergency department and found a prevalence of 25% active H pylori infections. These patients were tested and given triple therapy for H pylori. This took place at George Washington University and a study is currently underway to follow the symptoms of the patients who were tested and treated.
The key to treatment is compliance for the full regimen. Triple therapy and quadruple therapy often cause significant nausea, but stopping treatment early causes high rates of bacterial resistance.
References
- Meltzer AC, Pierce R, Cummings DA, Pines JM, May L, Smith MA, Marcotte J, McCarthy ML. Rapid (13)C Urea Breath Test to Identify Helicobacter pylori Infection in Emergency Department Patients with Upper Abdominal Pain. West J Emerg Med. 2013 May;14:278-82.
- Epplein M, Signorello LB, Zheng W, Peek RM Jr, Michel A, Williams SM, Pawlita M, Correa P, Cai Q, Blot WJ. Race, African ancestry, and Helicobacter pylori infection in a low-income United States population. Cancer Epidemiol Biomarkers Prev. 2011 May;20:826-34.
- Delaney BC, Qume M, Moayyedi P, Logan RF, Ford AC, Elliott C, McNulty C, Wilson S, Hobbs FD. Helicobacter pylori test and treat versus proton pump inhibitor in initial management of dyspepsia in primary care: multicentre randomised controlled trial (MRC-CUBE trial). BMJ. 2008 Mar 22;336:651-4.
- Talley, Nicholas. "Management of Dyspepsia." American College of Gastroenterology. Am J of Gastroenterology, 2005. Web. 21 Aug. 2014.
Written by Tyler Winders, MD