Clinical Presentation:
- Latent TB: Latent TB is diagnosed with positive Tuberculin skin tests or newer ELISA tests, with negative symptoms and negative CXR
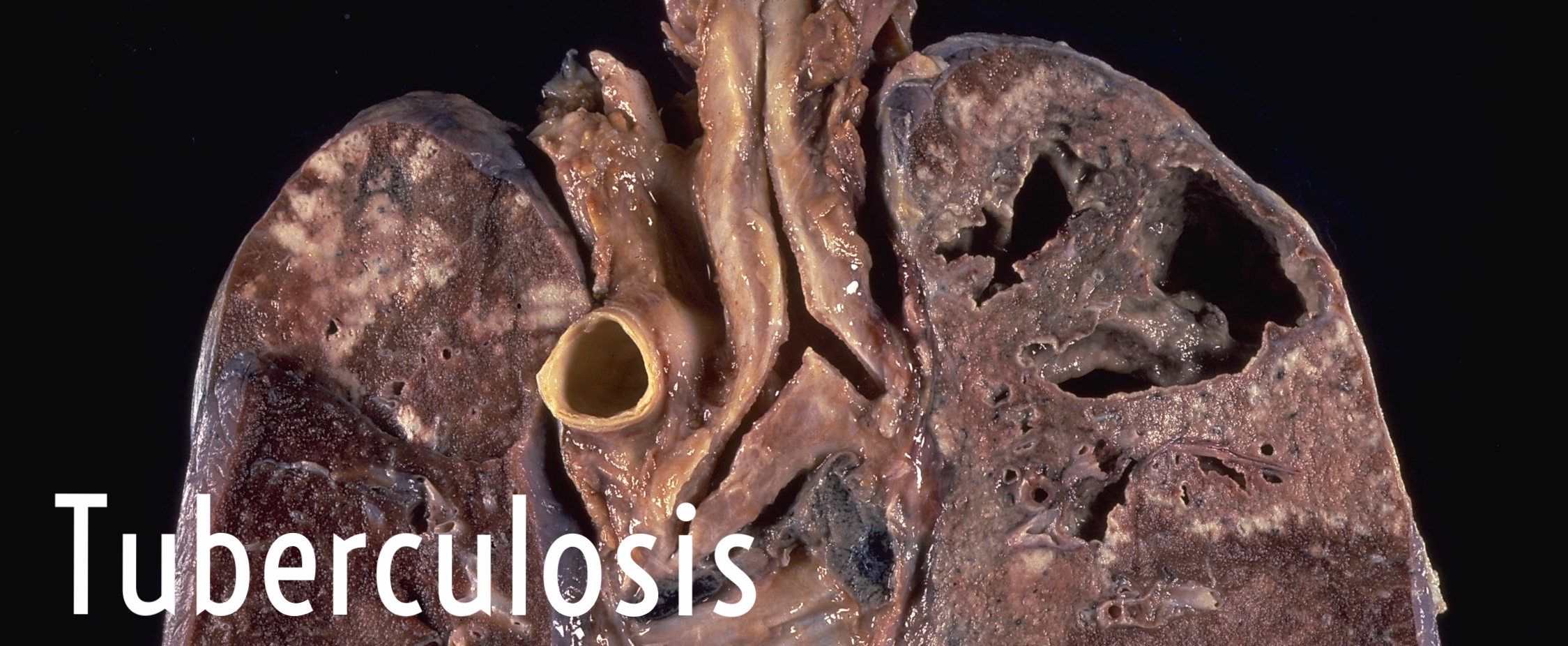
- Pulmonary Tuberculosis: Active pulmonary disease is characterized by 3 weeks of cough, chest pain, productive sputum or hemoptysis as well as weakness, weight loss, fevers and night sweats
- Extra-Pulmonary Tuberculosis:
- Lymphadenitis - the most common form of extra pulmonary tuberculosis. Cervical adenopathy is most common, but inguinal, axillary, mesenteric can occur
- Skeletal - bone and joint tuberculosis = 35% of extrapulmonary TB. Tuberous arthritis is commonly in knees and hips, involving one joint, while spine (Pot’s disease), present as back pain, progressing to paralysis in ½ patients
- Central nervous system - includes tuberculous meningitis (the most common presentation), intracranial tuberculomas and spinal tuberculous arachnoiditis. Present with headache for 2-3 weeks, AMS, fever and with focal CNS findings dependent on location
- Abdominal tuberculosis - may involve the gastrointestinal tract, peritoneum, mesenteric lymph nodes. Present with peritonitis, perforated bowel, abdominal pain, and diarrhea
- Miliary TB - progressive, disseminated form of tuberculosis, that can presents as septic shock, acute respiratory distress syndrome, and multiorgan failure. Classically, CXR can reveal numerous nodules scattered throughout the lung in > 85 percent of patients
THE STATE OF TB IN THE WORLD
According to data from 2012, an estimated 27 % of all tuberculosis infected patients live in sub-Saharan Africa, with the highest prevalence being in South Africa, Botswana, Swaziland, Zimbabwe and Mozambique. The high prevalence correlates directly with HIV prevalent areas. The majority of TB is not active TB, but latent TB, when a patient is infected with M tb, but does not have symptoms and is not able to infect other individuals. ~10% of latent TB will progress to active TB
Diagnosis
Active TB is a diagnosis starting with clinical suspicion of physical exam or imaging. The gold stand confirmatory test of AFB stain/culture of sputum, tissue or fluid from site of infection is available but delayed, and if suspicion of pulmonary infection is considered, isolation measure need to be ensured. Quantiferon gold is a serum test with increased specificity. When treating in developing countries, We do not have testing, so our diagnosis will be based mainly on symptoms and risk factors, as well as history, with high index of suspicion and referral
Treatment
Active TB
Preferred Regimen
- Initial Phase - Daily rifampin, isoniazid, pyrazinimide, ethambutol for 8 weeks
- Continuation Phase - Daily rifampin, isoniazid for 18 weeks or twice weekly rifampin, isoniazid for 18 weeks
Alternate Regimen
- Initial Phase - Daily rifampin, isoniazid, pyrazinimide, ethambutol for 2 weeks, then twice weekly for 6 weeks
- Continuation Phase - Twice weekly rifampin, isoniazid for 18 weeks
Latent TB
- Isoniazid for 6-9 months
- Isoniazid, Rifapentine for 3 months
- Rifampin for 4 months
Written by Bret Betz, MD