Background
Salmonella enterica is a common cause of enteric fevers in developing nations. The CDC estimates more than 20 million cases yearly worldwide with just around 5000 cases in the US ( with the majority due to travel). The bacteria lives solely in humans and is transmitted via the fecal-oral route. Children and the elderly most often experience severe symptoms and are at highest risk for serious sequelae of the illness.
Clinical Presentation
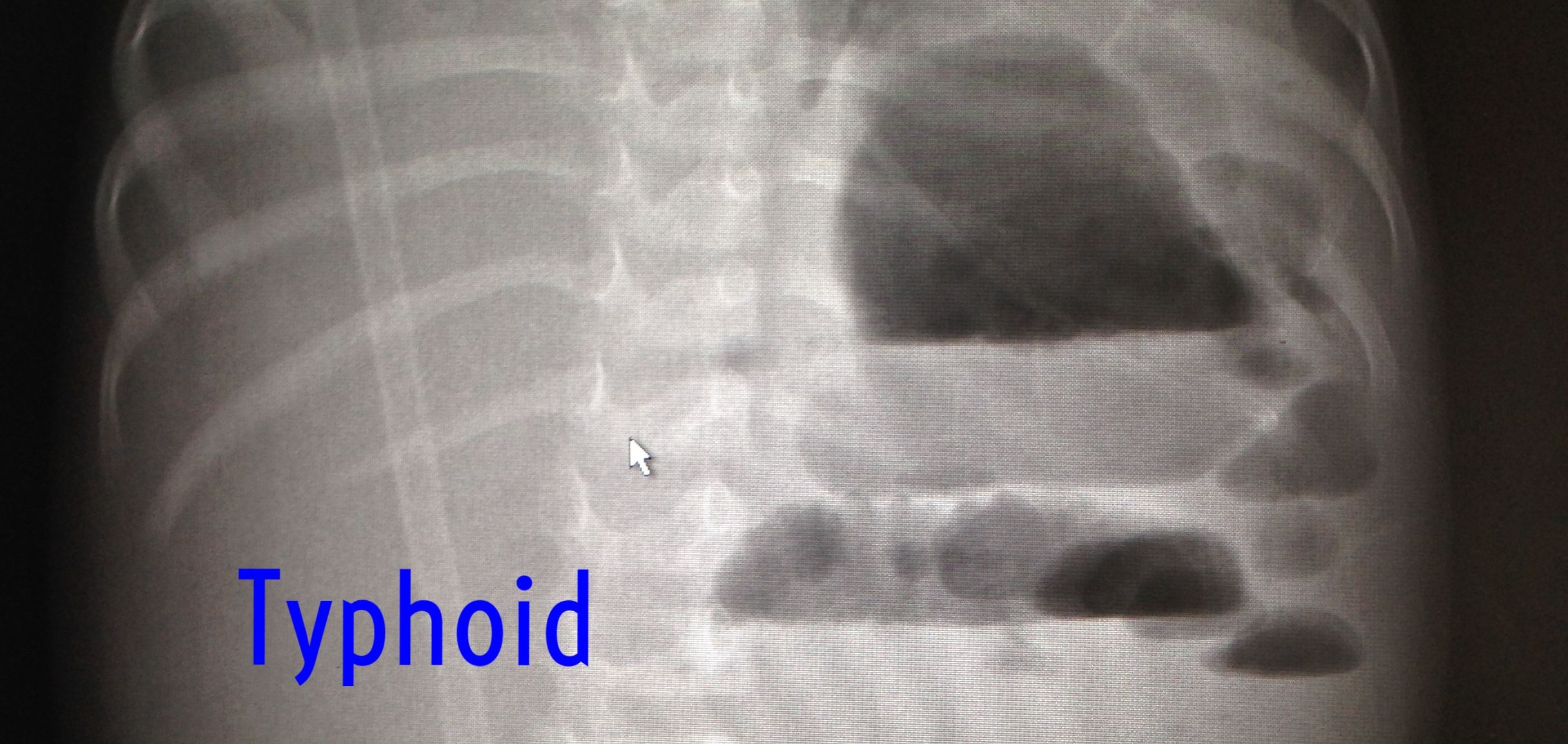
Typhoid fever, true to its name, often presents with high fevers. Between 5-21 days after inoculation, patients will develop GI symptoms and fevers that increase in a stepwise manner. Interestingly, typhoid may present with diarrhea or constipation. Diarrhea is more common at approximately 70% of cases, but constipation certainly is not uncommon. Classically, the illness progresses to intestinal bleeding and may be associated with a rash and hepatosplenomegaly. One complication to consider in patients presenting with typhoid fever is intestinal perforation. Hyperplasia and necrosis at Peyer’s patches is believed to be the underlying pathology. Rates of perforation vary between 1-20% depending on the study quoted.
Prevention
Consumption of clean food and drink is obviously key. Utilizing bottled water and avoiding ice made from non-potable water are easy to follow recommendations. Ensure foods are adequately cooked and maintain good hand washing and hygiene practices.
Vaccinations are also available. There are both a live attenuated vaccine that is administered orally and a intramuscular polysaccharide vaccine. Both have been shown to be useful, although the parenteral version is more efficacious as it offers 70% protection at 1 year. Passive immunity dwindles quickly, and repeat vaccination is recommended for frequent travelers
Treatment
Antibiotic therapy has significantly decreased the mortality rate of Typhoid fever since their introduction. Resistance patterns have led to a shift toward the third generation cephalosporins, azithromycin, and fluoroquinolones as empiric therapy, although cultures are recommended as drug-resistant strains are becoming more common. Some common drug regimens:
- Ciprofloxacin: 500 bid po or IV x 7-10 days
- Cefixime (20 mg/kg per day orally in two divided doses) for 7 to 14 days (alt: ceftriaxone 2g IV daily)
- Azithromycin (1 g orally once followed by 500 mg once daily for 5-7 days or 1g po daily for 5 days)
Monitoring for complications is crucial as well. Perforation is most common during the 3rd week of illness, and as previously stated, as many as 1 in 5 cases may experience this event. Prompt surgical intervention coupled with broadened antibiotics targeting gut colonizers is recommended.
Article by Tyler Winders, MD