TEE Advanced: Cardiac Arrest Evaluation
The following guide is meant to provide a general framework for targeted evaluation with transesophageal echocardiography (TEE) during cardiac arrest. This post is a follow-up to the Introduction to TEE post which covers techniques for TEE probe insertion and basic view acquisition in greater detail.
INTRODUCTION
The quality of transthoracic echocardiography (TTE) images during cardiac arrest can be limited by ongoing cardiopulmonary resuscitation (CPR), defibrillator pads, body habitus, subcutaneous air, or gastric insufflation from positive pressure ventilation. By imaging the heart from the vantage point of the esophagus, transesophageal echocardiography (TEE) bypasses intervening thoracic structures and more reliably produces high-quality images. Studies have demonstrated emergency medicine physicians were able to obtain interpretable intra-arrest TEE images ~98% of the time vs 75-80% for TTE [1,2,3,4]. Additionally, TEE can be performed continuously during a resuscitation, avoiding the prolongation of pulse check duration that has been observed with TTE [5]. TEE can also provide new information to the resuscitation team, with ~50% of exams identifying information that would not be easily seen on TTE [4]. While data demonstrating an impact on resuscitation outcomes is predominantly limited to single-centered observational studies, such studies have shown that TEE can establish a likely etiology for arrest in ~30-40% of cases and was found to have diagnostic or therapeutic impact ~70-97% of the time [3,6].
The remainder of this guide will describe how to use TEE to optimize CPR quality by determining the area of maximal compression, detect cardiac activity and subtle rhythms, and evaluate for potential causes of arrest.
Evaluate for the Area of Maximal Compression (AMC)
High-quality chest compressions are an essential component of CPR. Ideally, chest compressions simulate the cardiac pumping activity of spontaneous circulation by compressing the left ventricle, forcing aortic valve opening and ejection of blood into the aorta. However, according to cross-sectional imaging data, the central chest or inter-nipple line compression location endorsed by the American Heart Association was correctly aligned over the LV only 20-50% of the time [7–10]. In up to 80% of patients (particularly patients with cardiac disease), these recommended chest compression locations more commonly compresses the left ventricular outflow tract (LVOT) or aorta, inappropriately closing the aortic valve and preventing the ejection of blood from the left ventricle (LV) with compressions [8–10]. In a retrospective study of 19 refractory OHCA cases being evaluated for ECPR, no patients with LVOT compression during CPR achieved return of spontaneous circulation (ROSC) [11].
To determine whether the area of maximal compression (AMC) is located over the LV rather than the LVOT or aortic valve, use the mid-esophageal long axis view, which shows the LV, LVOT, aortic valve, and aortic root in the same plane. On TEE, the vector of compression should originate from near the RV (as the RV is anatomically closest to the chest wall) and progress toward the LV. Once the AMC is determined, evaluate whether the aortic valve is opening with each compression.
In radiologic studies of patients with cardiac disease, the optimal point of compression was actually located around 3 cm to the left and 1-2 cm caudally to the standard hand positioning location [10]. Therefore, if the AMC is over the LVOT or aorta, try relocating CPR hand positioning or Lucas placement more caudally or slightly leftward.
Analyze the following still images from CPR cycles demonstrating the AMC.
Relaxation
Compression
In this compression cycle, the AMC (arrow) is over the LVOT, note there is no aortic valve opening with compression.
Relaxation
Compression
In this compression cycle, the AMC (arrow) is just proximal to the aortic valve, with no apparent aortic valve opening with compression.
Relaxation
Compression
In this compression cycle, the AMC (arrow) is appropriately located over the left ventricle, note aortic valve opening with compression.
Now you practice! Evaluate the following clips for the AMC.
-
In this patient the initial AMC is over the proximal aorta. Notice that aortic valve opening does not reliably follow each compression.
-
AMC appears to be over the LVOT and proximal aorta. The aortic valve does not appear to open with compressions.
-
In a similar patient after repositioning the Lucas device, the AMC is located more over the LV with consistent aortic valve opening with each compression.
-
In this clip there is compression over the LV and there appears to be aortic valve opening with each compression. The Lucas device had just been repositioned in this patient. On the next pulse check, this patient got ROSC!
Evaluate for Organized Cardiac Activity and Rhythm
On a pulse check, check the rhythm on the patient’s monitor and compare this with visualized cardiac movement on ultrasound. This may be best done in the mid-esophageal 4 chamber view or mid-esophageal long axis view where the right and left ventricles can be visualized simultaneously.
Organized Cardiac Activity
While the definition of organized cardiac activity is not universally defined, our institution looks for cardiac movement with myocardial thickening that correlates with subsequent valve opening. By this definition, minimal myocardial movement that does not result in a change in chamber cavity size, isolated valve fluttering, or twitching is not considered cardiac activity [1]. Other findings such as extreme bradycardia or very weak contractions are considered cardiac activity if the myocardial activity correlates with valve movement.
Practice evaluating for Cardiac Activity on the following clips of patients presenting in cardiac arrest!
-
In this clip showing a mid-esophageal long axis view, there appears to be organized cardiac activity with LV wall thickening and subsequent aortic valve opening.
-
In this clip showing a mid-esophageal 4 chamber view, there seems to be some occasional valve fluttering but no apparent coordinated movement of the myocardium. This was interpreted by the care team as no organized cardiac activity.
-
This mid-esophageal 4 chamber view shows very weak organized ventricular contractions with some associated valve movement. Notice the smoke-like appearance of blood in the left atrium. This is known as spontaneous echo contrast and is associated with red blood cell aggregation at low flow rates. This is generally observed with prolonged CPR and is associated with resuscitation failure.
Pulseless electrical activity (PEA) vs Pseudo-PEA
PEA arrest refers to electrical activity on the monitor without organized cardiac activity on ultrasound, or electromechanical dissociation. Patients in PEA arrest generally have a lower rate of survival than patients with a shockable rhythm [11]. However, studies performed using TTE have shown that patients in PEA on the monitor with organized cardiac activity on ultrasound may have higher rates of ROSC and survival to discharge than patients without such organized cardiac activity on ultrasound [1,12,13]. This has been termed “pseudo-PEA” and may represent organized mechanical activity that is too weak to generate a palpable pulse, or profound cardiogenic shock. Using TTE data in a multi-institutional prospective observational study of 953 patients, 54% of patients in PEA on the monitor had organized cardiac activity on ultrasound, or were in pseudo-PEA [13]. When compared to patients in true PEA, patients in pseudo-PEA tended to have a higher rate of ROSC (51% vs 14%) and survival to discharge (3.8% vs 0.6%) [1]. When patients in pseudo-PEA patients were treated as patients in profound shock with continuous pressor infusions, there were higher rates of ROSC than patients in true PEA treated with continuous pressor infusions (90% vs 47%) [1].
-
In this mid-esophageal long axis view clip of a patient with presumed PEA on the monitor and no palpable pulse, there was organized cardiac activity on ultrasound. This was treated as pseudo-PEA and the patient was started on an epinephrine infusion and later achieved ROSC.
Fine Ventricular Fibrillation (VF) vs Asystole
Another point of distinction is differentiating asystole from fine ventricular fibrillation. In one case series of 33 OHCA patients, 4 patients who were thought to be in asystole were actually found to be in fine ventricular fibrillation and were subsequently treated with defibrillation [3].
-
In this mid-esophageal 4 chamber view on TEE, this appeared to be fine VF which was treated with defibrillation.
Evaluate for Reversible Causes of Arrest
Similar to TTE, TEE can be used to evaluate for potential reversible causes of arrest.
Hypovolemic vs Distributive or Obstructive Shock
The mid-esophageal 4 chamber view can be used to evaluate relative RV and LV size. A poorly filled RV and/or LV may indicate hypovolemia, distributive, or obstructive shock. Be mindful that in the setting of cardiac arrest, relative chamber size may be unreliable for estimating volume status due to inherently poor cardiac output. Similarly, IVC diameter and collapsibility are less reliable as measures of volume status given the lack of spontaneous breathing and spontaneous circulation.
Gross Systolic Function
Similar to TTE, during periods of ROSC, evaluate the RV and LV for gross systolic function. This can be done using a combination of mid-esophageal 4 chamber view, mid-esophageal parasternal long axis view, and the transgastric view. Note that myocardial stunning and reduced systolic function (involving LV, RV, or both) are common in the peri-arrest period due to global cardiac ischemia and may be a sequelae rather than cause of the arrest.
-
In the transgastric short axis clip (left), the systolic function appears to be moderately reduced globally. This is again demonstrated in the mid-esophageal long axis clip (right). Global hypokinesis is a common finding post-ROSC.
Regional Wall Motion Abnormalities (RWMA)
RWMA are generally only visible with organized cardiac activity, so are most likely to be found with ROSC or in pseudo-PEA. Interpret these with caution in the peri-arrest period. While RWMA can be a sign of a poorly perfused cardiac segment from an acute occlusive infarction, they can also be sequelae of global cardiac ischemia from poor perfusion during the arrest. RWMA can also be old from prior ischemic insults, so comparing to an old echocardiogram is recommended. Several post-ROSC TTE-based studies comparing echocardiography with catheterization findings have demonstrated RWMA to have sensitivity of 7-90% and specificity ~50% for acute coronary syndrome as the etiology of arrest [14–16].
-
The septal and posterior walls do not seem to be thickening to the same extent as the anterior and lateral walls concerning for septal and posterior regional wall motion abnormalities (RWMA).
Pericardial Effusion and Cardiac Tamponade
Evaluate for a pericardial effusion on multiple views. Look for possible findings of tamponade such as right atrial or right ventricular collapse. Evaluate for potential etiologies of the effusion such as aortic dissection or myocardial free wall rupture.
Pulmonary Embolus (PE)
An enlarged or akinetic RV may raise concern for possible PE, but note that this finding is not specific to PE, particularly in the peri-arrest setting. In one intra-arrest TEE case series, RV dilation was present on emergency department arrival in 57% of cases, but this persisted in only 8% post-ROSC [3]. Moreover, patients receiving bystander CPR and suffering less total downtime were less likely to have RV dilation on intra-arrest TEE. Even post-ROSC, in a series of patients with persistent RV dilation, only 50% were ultimately found to have a PE on computed tomography or autopsy [16]. This demonstrates that RV enlargement is frequently visualized peri-arrest, potentially due to poor forward flow and RV volume overload. An enlarged RV with a relatively empty LV may raise greater suspicion for obstructive shock from a PE than a simultaneously enlarged RV and LV, although there is a paucity of studies evaluating intra-arrest chamber diameter and subsequent confirmation of PE. Generally, it is advised to also consider the clinical context of the arrest and potential VTE risk factors before treating with thrombolytics. A quick evaluation of the femoral vessels for proximal deep venous thrombosis (DVT) may also be considered.
Thrombi in the right atrium (RA) or RV may indicate a “clot in transit” and raise further suspicion for PE, but this is an uncommon finding [17]. When PE is being considered, evaluate the RA and RV for thrombi using the mid-esophageal 4 chamber view. The main pulmonary artery can also be evaluated for proximal emboli using a upper- to mid-esophageal aortic short axis view [18]. From the mid-esophageal 4 chamber view, withdraw the probe to ~20-25 cm and adjust the omniplane to an angle of ~70-90°. In the near field will be a cross-section of the aortic arch, while on the left side of the screen there will be a long-axis view of the pulmonary artery.
Aortic Dissection
Given the close proximity of the aorta to the esophagus, TEE can produce a more comprehensive assessment of aorta anatomy and is more accurate in evaluating for thoracic aortic dissection than TTE [19-21]. One systematic review found a sensitivity of 98% of TEE for thoracic aortic dissection, although as with any ultrasound study, these results are likely operator-dependent [19]. While TEE has inferior sensitivity to helical CT (which can achieve up to 100% sensitivity), it can be a rapid and efficient means of evaluating suspicion for aortic dissection in post-ROSC patients too unstable to leave the resuscitation bay [19-21].
While dedicated aortic views can be obtained (see Introduction to TEE post), a rapid means to evaluate for dissection during a resuscitation can be to “run the aorta” (see clips on the right for examples). Start with a transgastric or mid-esophageal 4 chamber view and rotate the entire shaft of the probe toward the patient’s left to visualize the descending aorta. Slowly back out the probe to evaluate for an intimal flap. As the aortic arch comes into view, rotate the probe back to the anterior of the patient, gradually rotating rightward to see the arch and ascending aorta. Of note, the air within the trachea and left main bronchus that lies between the aorta and esophagus can make it difficult to visualize the distal ascending aorta and proximal aortic arch, producing a “blind spot” in this region. Omniplane can be used throughout the exam to visualize that aorta in long and short-axis. It it is recommended to view the aorta in multiple angles to avoid missing obliquely oriented dissection flaps. Evaluating for any associated aortic regurgitation, pericardial effusion, or left pleural effusion can raise suspicion.
-
In the left clip, showing a mid-esophageal long axis view, a pericardial effusion is visible. In the right clip, the aortic valve and proximal ascending aorta are visible. There appears to be a wispy, waving dissection flap within the proximal aorta, suggesting a proximal aortic dissection. The providers appropriately decided against thrombolytics!
Frequently Asked Questions
Can you defibrillate the patient (or dual-sequence defibrillate the patient) with the TEE probe inserted?
Multiple studies have shown that as long as the probe undergoes appropriate testing between use (leak testing), there does not appear to be any harm to the patient or provider when defibrillating a patient with the TEE probe in place. Our TEE probes go through this electrical safety and leak testing with each use and with their weekly processing.
Can you perform other ultrasounds at the same time as a TEE?
You can, but if the other ultrasound is being performed on the patient’s chest, you will get interference.
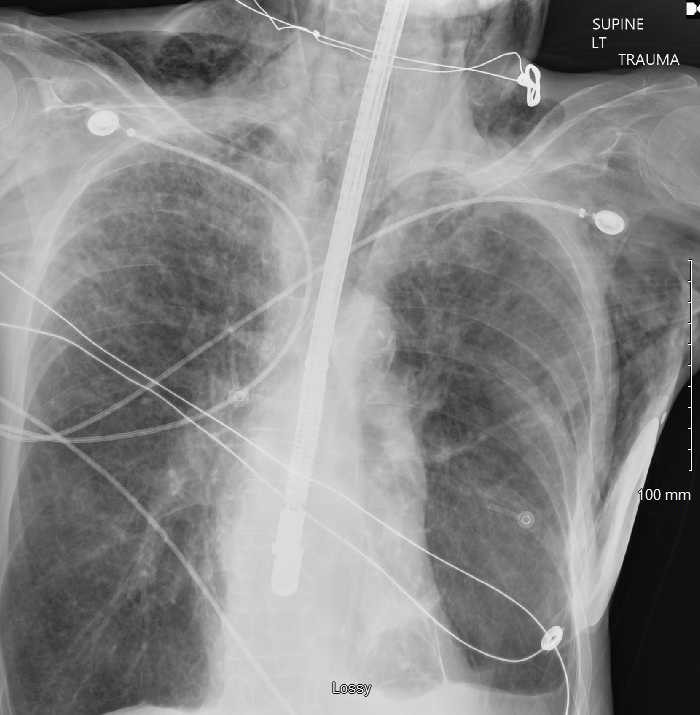
Can you get a chest xray with the TEE probe in place?
Yes, but expect to see the TEE probe on the Xray.
Can you perform compressions and/or use a Lucas with the TEE probe inserted?
Yes, there does not appear to be any harm, but some studies have chosen to avoid obtaining transgastric views with CPR in progress. However, there are no studies demonstrating transgastric TEE views have any increased risk compared to transesophageal views during ongoing CPR.
References
Gaspari R, Weekes A, Adhikari S, et al. A retrospective study of pulseless electrical activity, bedside ultrasound identifies interventions during resuscitation associated with improved survival to hospital admission. A REASON Study. Resuscitation. 2017;120:103-107. doi:10.1016/j.resuscitation.2017.09.008
Balderston JR, You AX, Evans DP, Taylor LA, Gertz ZM. Feasibility of focused cardiac ultrasound during cardiac arrest in the emergency department. Cardiovasc Ultrasound. 2021;19:19. doi:10.1186/s12947-021-00252-3
Teran F, Dean AJ, Centeno C, et al. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140-147. doi:10.1016/j.resuscitation.2019.02.013
Arntfield R, Pace J, Hewak M, Thompson D. Focused Transesophageal Echocardiography by Emergency Physicians is Feasible and Clinically Influential: Observational Results from a Novel Ultrasound Program. J Emerg Med. 2016;50(2):286-294. doi:10.1016/j.jemermed.2015.09.018
Fair J, Mallin MP, Adler A, et al. Transesophageal Echocardiography During Cardiopulmonary Resuscitation Is Associated With Shorter Compression Pauses Compared With Transthoracic Echocardiography. Ann Emerg Med. 2019;73(6):610-616. doi:10.1016/j.annemergmed.2019.01.018
Hussein L, Rehman MA, Jelic T, et al. Transoesophageal echocardiography in cardiac arrest: A systematic review. Resuscitation. 2021;168:167-175. doi:10.1016/j.resuscitation.2021.08.001
Shin J, Rhee JE, Kim K. Is the inter-nipple line the correct hand position for effective chest compression in adult cardiopulmonary resuscitation? Resuscitation. 2007;75(2):305-310. doi:10.1016/j.resuscitation.2007.05.003
Hwang SO, Zhao PG, Choi HJ, et al. Compression of the left ventricular outflow tract during cardiopulmonary resuscitation. Acad Emerg Med Off J Soc Acad Emerg Med. 2009;16(10):928-933. doi:10.1111/j.1553-2712.2009.00497.x
Nestaas S, Stensæth KH, Rosseland V, Kramer-Johansen J. Radiological assessment of chest compression point and achievable compression depth in cardiac patients. Scand J Trauma Resusc Emerg Med. 2016;24:54. doi:10.1186/s13049-016-0245-0
Catena E, Ottolina D, Fossali T, et al. Association between left ventricular outflow tract opening and successful resuscitation after cardiac arrest. Resuscitation. 2019;138:8-14. doi:10.1016/j.resuscitation.2019.02.027
Chan PS, McNally B, Tang F, Kellermann A. Recent Trends in Survival from Out-of-Hospital Cardiac Arrest in the United States. Circulation. 2014;130(21):1876-1882. doi:10.1161/CIRCULATIONAHA.114.009711
Flato UAP, Paiva EF, Carballo MT, Buehler AM, Marco R, Timerman A. Echocardiography for prognostication during the resuscitation of intensive care unit patients with non-shockable rhythm cardiac arrest. Resuscitation. 2015;92:1-6. doi:10.1016/j.resuscitation.2015.03.024
Gaspari R, Weekes A, Adhikari S, et al. Emergency department point-of-care ultrasound in out-of-hospital and in-ED cardiac arrest. Resuscitation. 2016;109:33-39. doi:10.1016/j.resuscitation.2016.09.018
Liu L, Karatasakis A, Kudenchuk PJ, et al. Scoping review of echocardiographic parameters associated with diagnosis and prognosis after resuscitated sudden cardiac arrest. Resuscitation. 2023;184:109719. doi:10.1016/j.resuscitation.2023.109719
Lee SE, Uhm JS, Kim JY, Pak HN, Lee MH, Joung B. Combined ECG, Echocardiographic, and Biomarker Criteria for Diagnosing Acute Myocardial Infarction in Out-of-Hospital Cardiac Arrest Patients. Yonsei Med J. 2015;56(4):887-894. doi:10.3349/ymj.2015.56.4.887
Elfwén L, Hildebrand K, Schierbeck S, et al. Focused cardiac ultrasound after return of spontaneous circulation in cardiac-arrest patients. Resuscitation. 2019;142:16-22. doi:10.1016/j.resuscitation.2019.06.282
Jung WJ, Cha KC, Kim YW, et al. Intra-arrest transoesophageal echocardiographic findings and resuscitation outcomes. Resuscitation. 2020;154:31-37. doi:10.1016/j.resuscitation.2020.06.035
Hahn RT, Abraham T, Adams MS, et al. Guidelines for Performing a Comprehensive Transesophageal Echocardiographic Examination: Recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964. doi:10.1016/j.echo.2013.07.009
Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y. Diagnostic Accuracy of Transesophageal Echocardiography, Helical Computed Tomography, and Magnetic Resonance Imaging for Suspected Thoracic Aortic Dissection: Systematic Review and Meta-analysis. Arch Intern Med. 2006;166(13):1350-1356. doi:10.1001/archinte.166.13.1350
Kim YW, Jung WJ, Cha KC, et al. Diagnosis of aortic dissection by transesophageal echocardiography during cardiopulmonary resuscitation. Am J Emerg Med. 2021;39:92-95. doi:10.1016/j.ajem.2020.01.026
Tanaka Y, Sakata K, Sakurai Y, et al. Prevalence of Type A Acute Aortic Dissection in Patients With Out-Of-Hospital Cardiopulmonary Arrest. Am J Cardiol. 2016;117(11):1826-1830. doi:10.1016/j.amjcard.2016.03.015