INDICATIONS:
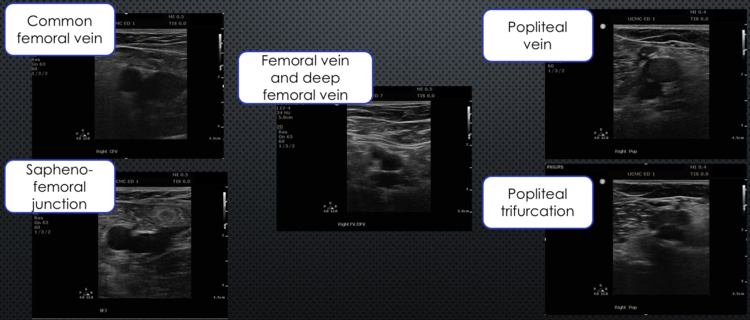
REQUIRED IMAGES:
Obtain clips demonstrating compression of the vein. Another option is to utilize dual mode and obtain side-by-side still images of each site uncompressed and compressed.
DVT
Lower Extremity Compression Ultrasonography to Assess for Deep Vein Thrombosis
Objectives - Assess for compressibility of:
The common femoral vein
The saphenofemoral junction
The femoral vein
The deep femoral vein
The popliteal vein and its trifurcation
The goal is to assess the compressibility of the femoral vein at the saphenous-femoral junction (SFJ), the common femoral vein (CFV) and the femoral vein/deep femoral vein (FV/DFV), as well as of the popliteal vein and the popliteal trifurcation. Inability to compress at any of these points is suggestive of deep vein thrombosis (DVT)in that vein.Clots may sometimes be visualized ashyperechoic density within the vessel, but since some are anechoic, failure to directly visualize a clot does not rule it out. However, regardless of its echogenicity, the vein will not compress when a clot is present.
Background:
Unilateral leg pain and/or swelling is a commonly seen complaint in the Emergency Department. Ultrasound is the gold standard for diagnosis of DVT. While this is non-invasive and relatively inexpensive compared to other imaging studies, it can be time consuming to send patients to the radiology or vascular lab for a formal full-length lower extremity study. Moreover, there are some institutions that do not have radiology-performed ultrasonography available at all hours. Emergency physicians performing bedside 2-point compression ultrasound can save time and expedite safe dispositions.A 2004 prospective, single-blind, observational study examinedthe time savings of ED bedside US vs radiology studies which showed that the mean time from triage to disposition in the former group (95 minutes) was significantly less (P<0.0001) than in the latter group (220 minutes) with excellent agreement between the studies.1
Numerous studies have demonstrated the validity of limited ultrasound imaging performed by emergency physicians. Burnside et al. performed a systematic review of studies on the diagnostic performance of emergency physicians in DVT ultrasound which found a pooled sensitivity and specificity of 95% [95% CI= 0.87 to 0.99]and 96%[95% CI = 0.87 to 0.99], respectively.2 In another systematic review and meta-analysis, Pomero et al. looked at the accuracy of emergency physician-performed ultrasound (EPPU) for the diagnosis of DVT compared to radiology performed US or angiography. They found a weighted mean sensitivity of EPPU of 96.1% (95% CI 90.6-98.5%) and weighted mean specificity of 96.8% (95% CI 94.-98.1%).3
The emergency-physician performed DVT study focuses only on proximal deep veins of the leg above the knee and does not evaluate for distal or calf vein thrombosis. The evaluation for and treatment of distal deep vein thrombosis varies among practitioners and institutions.
Anatomy:
Below the iliac ligament the iliac vein becomes the common femoral vein. As this vein travels distally, the saphenous vein joins it from its more medial and superficial position. The common femoral vein then bifurcates into the deep femoral vein and the femoral vein.
The femoral vein was previously known as the superficial femoral vein, but that terminology was dropped to maintain clarity that this is a deepvein. The femoral vein dives into the adductor canal and becomes the popliteal vein distally. The popliteal vein traverses the popliteal space behind the knee and trifurcates into the posterior tibial vein, anterior tibial vein and the peroneal vein. Venous anatomy can have many variants and the variation increases in distal veins.
How to perform the exam:
Patient Positioning:Have the patient lie supine or recumbent with leg of interest resting in external rotation at the hip with the knee slightly flexed. You may be able to improve visibility of vessels by placing patient in slight reverse Trendelenburg to encourage venous pooling/distention.When assessing the popliteal vessels, the knee should be more flexed with the hip in flexion and external rotation.
Probe selection:
High frequency linear transducer. Convention is to orient the probe so that the indicator is directed to the patient right in the transverse position.
The views:
In the groin the points of compression from proximal to distal are:
The saphenous-femoral junction (SFJ)
The common femoral vein (CFV)
The femoral vein/deep femoral vein (FV/DFV)
In the popliteal space the points of compression from proximal to distal are:
Popliteal vein proximal to the Popliteal trifurcation: where the popliteal divides into the anterior and posterior tibial veins and peroneal vein.
Begin with the probe in the transverse orientation just distal to the inguinal ligament. The femoral vessels are approximately at the midpoint between the pubic symphysis and anterior superior iliac spine. You can also palpate the femoral artery to identify a starting point.The veinwill typically lie medialand superficialto the artery. The vein will appear as a round, thin walled, hypoechoic structure, while the artery will appear similar but with a thick wall and often has visible pulsation. Using evenly applied pressure, push down with the transducer to visualize the compression (or lack thereof) of the vein. If the vein does not compress completely, an intraluminal thrombus is present.
Common femoral vein and artery without Compression
Common femoral vein and artery with compression
After identifying the femoral artery and vein and ensuring complete compression, move the transducer caudad until you find the great saphenous-femoral junction. The saphenous joins the common femoral vein from a more superior position at the saphenofemoral junction. Compress to ensure complete compressibility. If there is lack of compression in the proximal great saphenous vein suggesting thrombosis this is also treated as a deep vein thrombosis and as these have a high risk of propagating into the femoral vein.
The saphenofemoral junction: CFA = common femoral artery, CFV = common femoral Vein, GSV = great saphenous vein
Continue to slide caudad until the common femoral artery and vein are visualized alone and repeat the compression test. Lastly, slide the probe until the common femoral vein separates and the femoral and deep femoral veins are seen in the same image. Finding this bifurcation can be occasionally be difficult. Typically, the common femoral artery will bifurcate in a more cranial position than the common femoral vein. Visualizing the common femoral vein in the long axis can often assist in identifying the bifurcation of the femoral vein.
At the level of the femoral vein and deep femoral veins; CFA = common femoral artery, FV = femoral vein, DFV = deep femoral vein
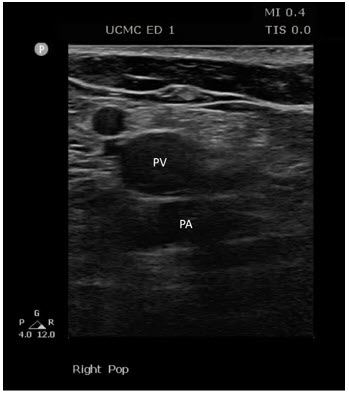
Move the probe to the popliteal fossa for evaluation of the popliteal vein and trifurcation. Maintain the probe in the transverse orientation with the indicator directed to the patient’s right. The vein normally lies superficial to the artery (Remember: “Pop on top” meaning that the popliteal vein is more superficial to the artery in your image). It can sometimes be challenging to find the popliteal vein and doing so can be facilitated by placing the patient in the prone position and passively flexing the knee. If the operator is applying too much pressure, it can be difficult to visualize the vein as it may already be compressed. Once the vein is identified and compressed, the final view is obtained by sliding the probe distally until the vein divides into three smaller vessels.
In the popliteal space; PV = popliteal vein, PA = popliteal artery
Troubleshooting:
As mentioned above, patient positioning can help improve the ability to visualize the vessels. Options include placing patient in reverse Trendelenburg or having them hand the leg over the edge of the bed.
Finding the appropriate anatomy in obese patients can be difficult. In these patients you may need to use the curvilinear probe.
Beware the thrombus mimics!
Rouleaux formations are an accumulation of red blood cells overlying venous valves and can easily be mistaken for DVT. This is sometimes referred to as the “sludge sign.” However, unlike DVT, rouleaux formations are compressible and compression of distal veins will clear the formation, while DVT will not clear.
Lymph nodes will appear as round structures with echogenic centers that appears like a DVT. However, these are non-compressible, discrete ovoid structures and usually do not have an associated artery adjacent to them the way a vein will.
Pathology:
The appearance of echogenic material within the vessel lumen is indicative of probable thrombus. If the thrombus is chronic you still may seem some degree of compressibility of the lumen. Chronic DVTs are of less concern, however, unless the patient has a known prior DVT in the vessel in question, it is best to treat as acute.
Pattie’s Pearls:
The indicator is imperative. Remember: NAVEL. Nerve, artery, vein, empty space, lymphatics
For finding the great saphenous vein, remember that it has a medial placement relative to the common femoral vein
Try to be as perpendicular as you can when compressing.
If you are not sure if you are compressing the vein adequately, check for compression of the artery.
Two compressions per clip ensure that anyone viewing your images has a chance to appreciate full compression of the vein.
For a difficult body habitus, decrease the frequency to increase the penetration.
Adequately remove clothing. Don’t compromise your exam battling boxers or Spanx.
Having trouble seeing the popliteal vein? Let up on your pressure and increase the depth.
Having trouble compressing or keeping the popliteal on the screen while you do? Try putting on hand on the patient’s knee while compressing, place the patient on their side or lay them prone.
Last but not least, don’t forget to label your images!!
References:
Theodoro D, Blaivas M, Duggal S, Snyder G, Lucas M. Real-time B-mode ultrasound in the ED saves time in the diagnosis of deep vein thrombosis (DVT). The American journal of emergency medicine. 2004;22(3):197-200.
Burnside PR, Brown MD, Kline JA. Systematic review of emergency physician-performed ultrasonography for lower-extremity deep vein thrombosis. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine. 2008;15(6):493-498.
Pomero F, Dentali F, Borretta V, et al. Accuracy of emergency physician-performed ultrasonography in the diagnosis of deep-vein thrombosis: a systematic review and meta-analysis. Thrombosis and haemostasis. 2013;109(1):137-145.
Ultrasound for Deep Venous Thrombosis. EB Medicine https://www.ebmedicine.net/topics.php?paction=showTopicSeg&topic_id=252&seg_id=4864, 2018.
Ultrasound Guidelines: Emergency, Point-of-Care and Clinical Ultrasound Guidelines in Medicine. Annals of emergency medicine. 2017;69(5):e27-e54.
Lars J Grimm M, MHS. Bedside Ultrasonography in Deep Vein Thrombosis. Medscape 2017; https://emedicine.medscape.com/article/1362989-overview#a3.
Kobner S. PV Card: Focused Deep Vein Thrombosis (DVT) Ultrasound. ALiEM 2015; https://www.aliem.com/2015/03/pv-card-focused-deep-vein-thrombosis-dvt-ultrasound/.