Grand Rounds Recap 9/14
/Dr. Darren Braude: Extraglottic Airways - Updates and Controversies
Rapid Sequence Airway (RSA): same idea as RSI, but intentionally using an extraglottic device for airway management rather than an endotracheal tube.
EGD culture at Dr. Braude’s practice:
- >85% of prehospital OHCA arrive with EGD, and EGD is generally left in place for initial resuscitation
- Some flight crews are utilizing “RSA”
- Did the patient code in the ED? Is there difficulty with 1st or 2nd endotracheal intubation? Is the patient's hypoxemia refractory to BVM?
- Place EGD.
- If the patient is hypoxemic and needs an intubation?
- Then DSI or RSA is utilized.
Myth Busting
- Controversy #1: ETT cuff prevents aspiration
- Reality: many of our patients have already aspirated
- In Dr. Braude’s opinion, intubation is more likely to cause aspiration than EGD placement
- Many EGDs provide some good protection against aspiration via gastric decompression
- A follow-up analysis of factors associated with head injury mortality after paramedic RSI: Conclusions showing out of hospital RSI by paramedics didn’t prevent aspiration pneumonia
- Ask yourself: Is it worth the added risk of endotracheal intubation if what we’re trying to prevent (aspiration) may have already occurred or may never occur?
- Controversy #2: EGDs compromise Cerebral Perfusion Pressure
- Swine data measuring carotid artery blood flow with EGD vs ETT, found significantly decreased cerebral blood flow
- Radiographic evaluation of carotid artery compression in patients with EGD in place. CT scan of 17 patients with EGD, looking for any sign of carotid compression in humans. No evidence of mechanical compression with king, LMA, and combitube
- Limitations: Patients weren’t in low flow state (cardiac arrest, ROSC, etc). Anatomy of swine in this regard is different
- Controversy #3: Do the ends justify the means? ie, Is the security of a definitive airway worth it at all costs?
- Complications associated with multiple laryngoscope attempts
- Study of Emergency tracheal intubation: complications associated with repeated laryngoscope attempts. Anesthesiologists responding to out of OR calls. Grouped into 2 or less attempts or >2 attempts. >2 attempts had higher complication rates (11% cardiac arrest)
- ICU: >1 attempt associated with higher complication rates
- ED: >1 attempt, adjusted odds ratio of 3.4 for hypoxemia
- Study of Emergency tracheal intubation: complications associated with repeated laryngoscope attempts. Anesthesiologists responding to out of OR calls. Grouped into 2 or less attempts or >2 attempts. >2 attempts had higher complication rates (11% cardiac arrest)
- By NEAR data, ED has around 87% first attempt success rate
- Consider your patients’ ability to tolerate more than one attempt, consider EGD as rapid backup
- Complications associated with multiple laryngoscope attempts
- Controversy #4: How best do you manage the Out of Hospital Cardiac Arrest (OHCA) airway?
- CARES registry Cincinnati paper: survival higher in ETT than EGD
- Problem with the data is that patients in EGD group include those that had multiple ETT attempts first, may be interfering with true outcome
- Dr. Braude’s opinion: if you feel you can successfully place ETT on first attempt during CPR, please do. If not, place an EGD.
- CARES registry Cincinnati paper: survival higher in ETT than EGD
- Controversy #5: RSA
- Give RSI drugs, then intentionally place EGD as your first choice
- In prehospital setting can use for keeping scene time short or in-flight difficulties
- Consider placing EGD in different clinical settings while training to gain some experience with them and become more comfortable with their use
- Keep lower airway predictors of difficulty with EGD in mind
- Don’t do RSA on a patient with predicted EGD difficulty
- The enemy of good is better: We may kill patients by trying to intubate when an EGD is perfectly adequate
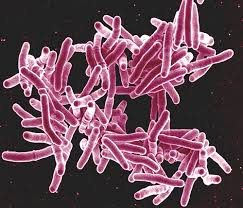
Case Follow-up with Dr. Devries: Tuberculosis
- 48 yo M, homeless, hx of alcoholism with increasing SOB/cough/sputum for 2 weeks, trouble swallowing, 10 lb weight loss.
- Previous ICU admissions for withdrawal and history of cocaine abuse.
- Presents with both tachycardia and tachypnea. EKG with sinus tachycardia. CXR with bilateral opacities in upper lobes. Labs show hyponatremia with normal lactate, troponin, CBC, and respiratory alkalosis.
- Ddx including pneumonia, aspiration, COPD, ACS.
- CT chest shows upper lobe cavitary lesions--> Tuberculosis!
Cavitary lung lesions:
- Bacterial infections
- Fungi
- Septic emboli (endocarditis, lemierre’s)
- Non-infectious (malignancy, PE with infarctions
Tuberculosis:
- Estimated 1/3 of world population has the infection
- Leading cause of HIV related deaths worldwide
- Diagnosis: primary infection can often be clinically insignificant
- Interferon Gamma Release Assay (IGRA) is recommended for patients who have had TB vaccinations or for those with feared poor outpatient followup
- Quantiferon gold testing is immune testing.
- If test is indeterminate consider immunocompromise and further testing
- In our facility this test is only run on Mondays and Thursdays
- If test is indeterminate consider immunocompromise and further testing
- Acid fast bacilli smear
- Not specific for TB, any mycobacterium will result
- Directly correlates with the infectivity of the individual
- Dr. Haglund with TB clinic gets automatic updates for any AFB smear positivity
- Quantiferon testing does not cross over automatically
- Utilize the order set as multiple cultures are needed
- Nucleic acid amplification test (NAAT)
- Recommended by CDC on at least one of your cultures to increase sensitivity
- If smear positive and NAAT positive-->start therapy
- Smear negative and NAAT positive--> repeat NAAT and clinical judgment for empiric treatment
- If second NAAT positive, begin treatment
- Emergency KT flowsheet for tuberculosis
- If patient has symptoms suggestive of TB (hemoptysis, weight loss, etc) and risk factors for TB then testing should be masked and get a CXR
- If CXR negative then place PPD and arrange followup
- If CXR positive with another alternative diagnosis not more likely, admit for further workup (consider medical hold vs high risk discharge for patients wanting to leave AMA)
- If patient has symptoms suggestive of TB (hemoptysis, weight loss, etc) and risk factors for TB then testing should be masked and get a CXR
- TB noncompliance
- Some jurisdictions have authorized compulsory detainment/isolation for public health
Patient followup: CAP with r/o TB admission, fungal cultures negative, HIV negative, had a bout of ETOH withdrawal. Long hospital stay with multiple bouts of worsening hypoxia and delirium. PEA arrest on hospital day 42 when found off oxygen. ROSC achieved, but diffuse ischemic brain injury
Important points:
- Consider screening for TB in high risk patients
- Early Isolation if TB suspected
- Obtain HIV testing in TB patients
- Turn to EmergencyKT for assistance in workup
Operations Update with Dr. Loftus
We had a very high volume over the past 2 weeks. 295 patients in a single day. Your positive attitude is helping make this transition manageable
Our platform for 2016-2017: to move the level of our clinical care in STEMI, stroke, sepsis, trauma and patent experience from good to great
- STEMI
- 4 cases in July/August
- Average door to balloon time of 27.5 minutes
- keep pushing for door to EKG time of <10 minutes
- Stroke
- 10 acute strokes with treatment in August
- median door to needle time of 40 minutes
- Sepsis
- Clinical quality measure with CMS
- Severe sepsis starts the clock on 3 and 6 hour bundles
- at <3 hours
- Order and draw lactate
- blood cultures attempted prior to appropriate antibiotics
- Broad spectrum antibiotics
- Administer gram negative coverage first over 30 minutes
- at < 6 hours
- repeat lactate if initial lactate is >2
- Septic shock: SBP <90 or MAP <65 or 40 mm Hg drop from baseline
- Clinical quality measure with CMS
- OB STAT alone (584-4444) for:
- Delivering mom
- Sick mom (eclampsia, bleeding, abdominal pain, syncope, unstable)
- Can call OB STAT and Trauma STAT together
- 'ED follow up' system from the ED
- Get social work involved on every one of these patients
- If considering sweet transitions clinic: order hemoglobin A1c
- Hoxworth medicine and med/peds clinics are for established patients ONLY. No new patients
- Trauma
- Remember to document activation times and be aware of activation criteria
- Consider involving trauma early if you suspect a patient will be going to the OR with another service
- Patent experience
- Press Ganey scores are heavily scrutinized in pretty much every health care system
- We tend to have difficulty of having higher scores in communication
- Update your patients, protect their privacy
- Zika Virus update
- We can order it, 3 day turn around
Pediatric EM Simulation Session
At your community hospital you see a 4 week old boy, normal birth history at 39 weeks gestation. Nasal congestion x 2 days, increased vomiting beginning yesterday, 6-7 episodes today, described as “yellow and green”. Tachycardia and tachypnea, SpO2 in low 90s. Mild/moderate cap refill delay, flat fontanelle.
- VBG shows 7.09/32/-12, Na 136, K 6.0, Hct 45, glucose 31, lactic acid 4.1
- Xray with dilated proximal bowel, paucity of distal small bowel gas
- Found to weigh only 1 ounce above birth weight
- REMEMBER: infants will drop 10-15% of weight after birth, should be back to birth weight by 1-2 weeks post partum
- The 6 P’s of weight loss in newborns
- Poop
- Pee
- Pump
- Pyloric stenosis
- Pulmonary
- Parents
- REMEMBER: babies and young children have precipitous decompensation, blood pressure dropping is a late sign
- Consider stress dose steroid administration, particularly if labs support adrenal insufficiency. If patient is not fluid responsive after 40-60 cc/kg consider administration of stress dose steroids as well
- Xray and history in this case is concerning for volvulus, that combined with these labs is ominous. Consider NG gastric decompression before transport as well
Oral Boards Case:
- 14 month old girl, brought to community hospital by EMS for seizure 19 minutes in duration thus far, actively seizing on arrival, no pharmacology administered thus far. Afebrile at home, no past medical history, normal birth history, no history of maternal HSV. Seizures cease with single dose of diazepam in ED. Temperature in ED 39.6. Withdraws to noxious stimuli, normal respirations. Unremarkable physical examination
- Criteria for simple febrile seizure:
- Age, 6 months to 6 years
- <15 minutes in duration
- No more than one episode in 24 hours
- Generalized seizure pattern
- Workup considerations
- iSTAT (7.29/46/-4)
- Urinalysis (negative for blood or protein, positive for nitrites, white count present)
- CBC (WBC 18)
- Complex febrile seizure
- Early assessment for glucose, airway monitoring, vitals
- If early response to pharmacotherapy and no GI symptoms consider less likely to have metabolic cause
- If good source for infection identified, further discussion regarding lumbar puncture and CT scan can be made in light of the patient's clinical presentation. Generally these are not needed, however if adjunctive physical examination findings such as bulging fontanelle or not returning to neurologic baseline consider adding these studies to workup
- 1/3 kids will have repeat febrile seizure in the future
- Consider sending parents home with diazepam if patient had complex febrile seizure
Oral Boards Case:
- 12 month old girl, presenting to ED with fever and fussiness for the past 2 days, worsening over the past 24 hours. Vitals: HR 180, BP 80/61, RR 35, Temp 40.1, 98% on room air, weighs 10 kg. Mom describes that patient has been “clingy”, difficulty with sleeping, decreased PO intake, decreased wet diaper production (3-4 over past 24 hours). No cough present, congestion present. Full term birth history with no complications. Patient attends daycare, no known sick contacts. Up to date on all vaccinations.
- Fussy during exam, mildly consolable by mom. MMM, erythema to TM but no bulging or effusion, full neck ROM, tachycardia, cap refill 3-4 seconds, good breathing, soft belly, no skin findings, good tone, tense fontanelle
- CBC with white count of 18 and 2 bands
- CSF has 199 WBC and 10 RBC
- Gram stain shows no organisms
- Protein 77, glucose 55
- Tx with acyclovir 20/kg q8hrs
- Ceftriaxone 100 mg/kg
- Vancomycin
- The results here suggest viral source, but in a clinically sick child, few would fault you for treating empirically and admitting to follow cultures.