Anatomy of a Procedure - Subclavian Cannulation
/Anatomy
The subclavian vein (SCV) is an important site for central venous access. Cannulation of the SCV is associated with infectious and thrombotic complications to a lesser extent that the most common alternative sites (internal jugular vein [IJV] and femoral vein [FV]). Further, infraclavicular SCV access does not interfere with cervical immobilization in trauma patients and this location permits greater patient mobility after placement. However, access of the SCV is technically challenging due to the overlying clavicle and the proximity to the subclavian artery (SCA), phrenic nerve, brachial plexus, dome of the pleura/lung, and on the left side, the thoracic duct. The SCV is incompressible, rendering tamponade of bleeding by external pressure impossible. A detailed understanding of the SCV and its anatomic relationship to adjacent structures is critical if complications associated with cannulation are to be minimized. With the advent of ultrasound potential complications associated with the procedure are greatly reduced, but even with sonographic guidance it is critical to be familiar with the local anatomy to facilitate efficient cannulation and avoid injury to adjacent structures.
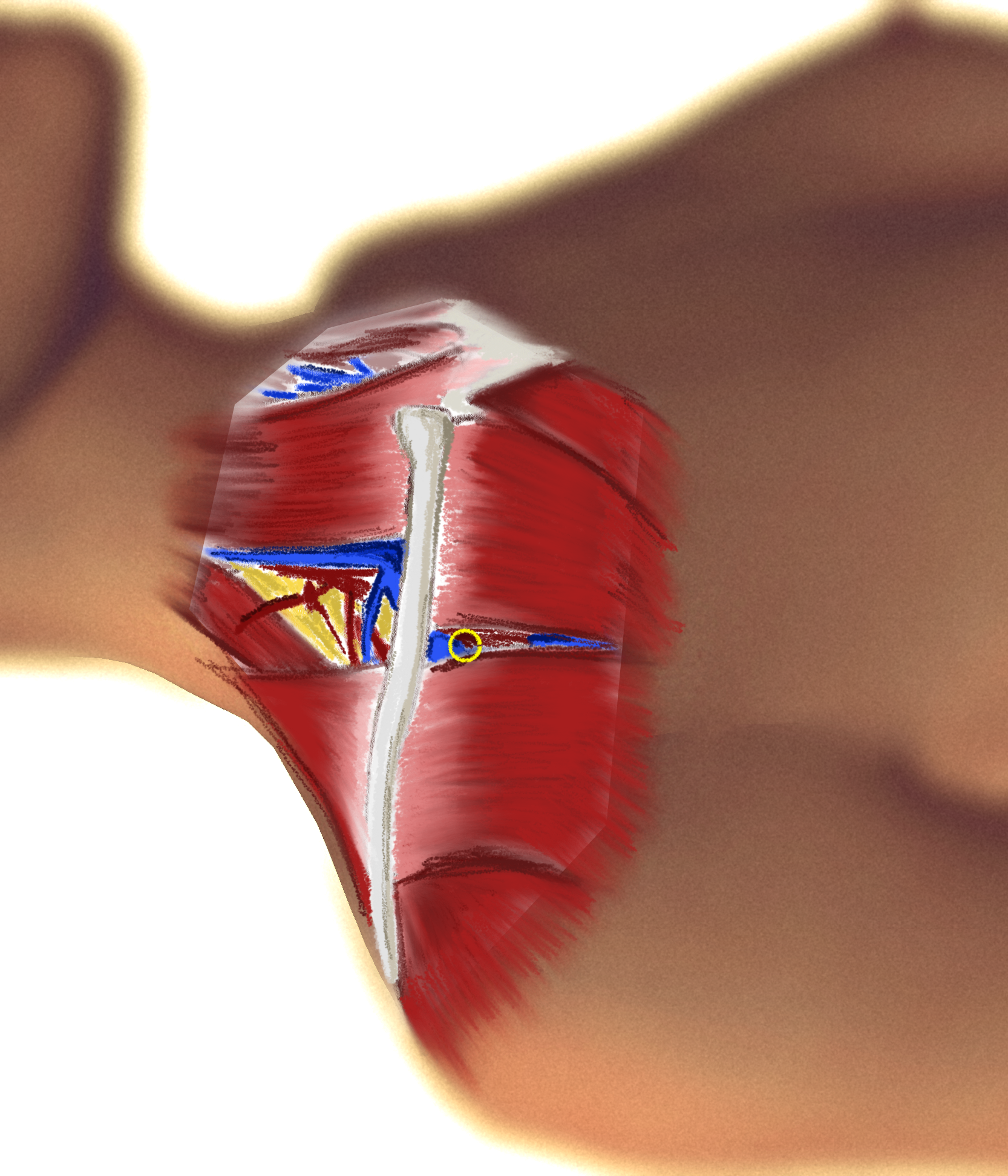
The axillary vein (AV) is redesignated the SCV at the lateral margin of the first rib, posteroinferior to the middle-third of the clavicle and the subclavius muscle. At its origin, the SCV lies in a shallow groove superficial to the medial portion of the first rib. From the medial border of the rib to the termination of the SCV at its juncture with the IJV, the vein lies directly on the dome of the parietal pleura. This pleural dome is slightly higher on the left than on the right, increasing the potential for lung puncture and pneumothorax during cannulation of the vein on that side.
In the majority of persons the vein lies anterior to the insertion of the anterior scalene muscle (ASM) on the first rib. This muscle then separates the vein and the parallel subclavian artery (SCA); in a minority, though, the vein is posterior to the ASM and there is little space between the two vessels. The SCA lies posterior and superior to the SCV through their lengths. The SCV averages 6 cm in length and has a luminal diameter that is variable depending on the volume status and size of the individual - calibers of 0.7 mm to 20 mm are commonly seen in adults. The medial portion of the SCV is thought to be non-distensible with a diameter fixed by a surrounding connective tissue investment that blends between the adventitia of the vein, the periostia of the clavicle and first rib, and the fasciae of the costoclavicular ligament and subclavius and anterior scalene muscles. Lateral to this the caliber of the SCV and AV can be increased by Trendelenberg. Various head and arm positions also have been purported to influence the diameter of the SCV, but the studies show inconsistent results; some. There is consensus agreement, however, that placing a roll between the shoulders reduces the space between the underlying first rib and the overlying clavicle, and may compress the vein.
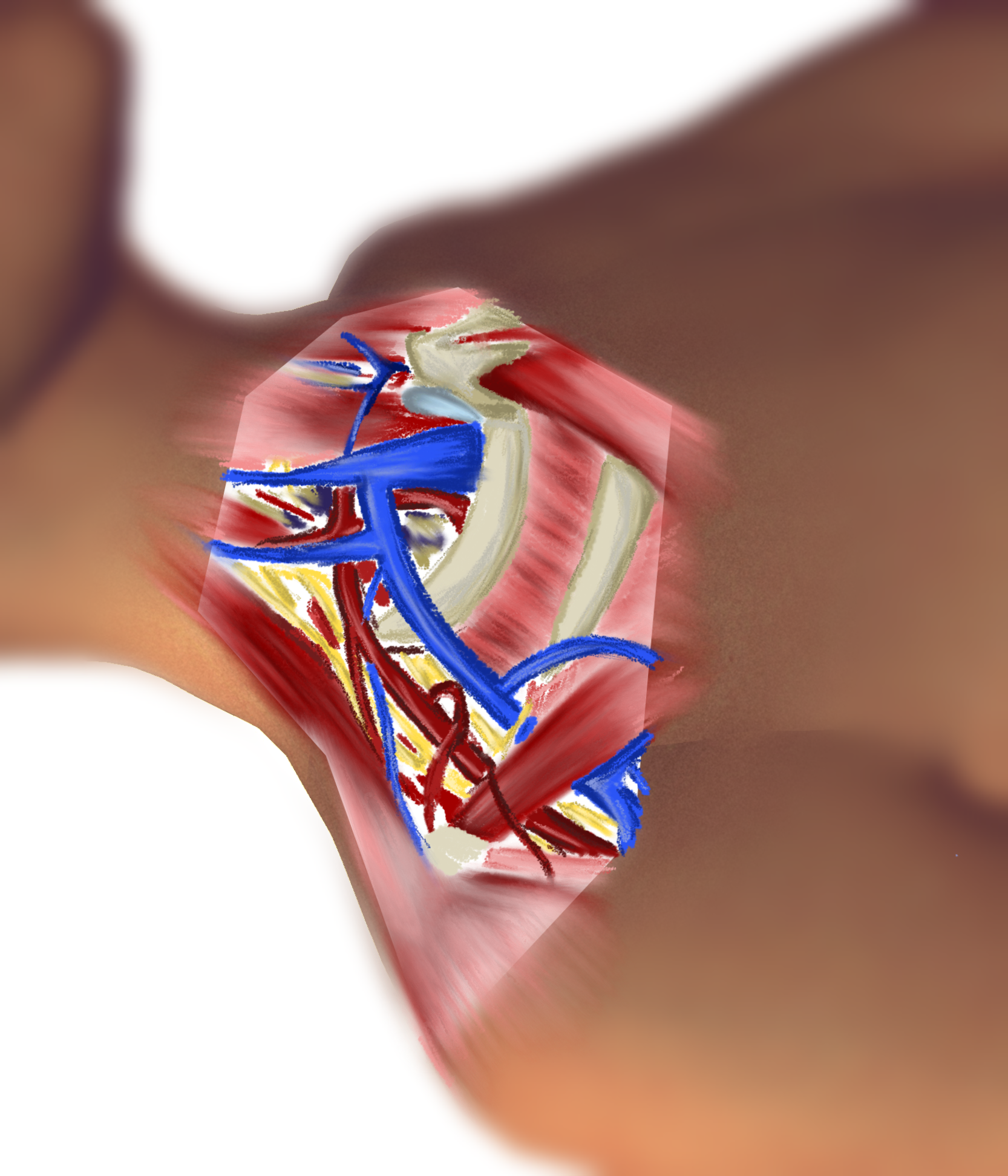
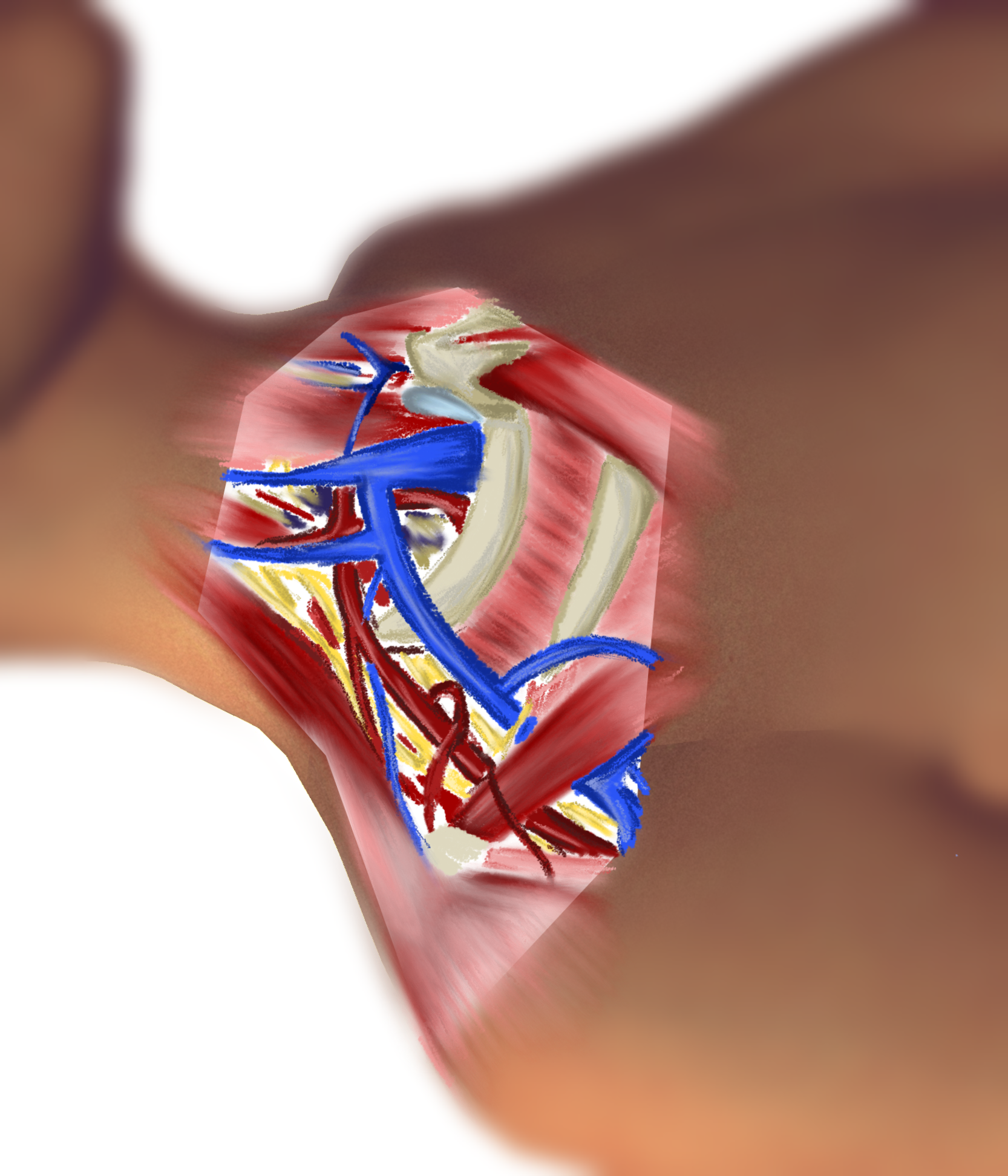
The SCV ends at its junction with the IJV, where the two veins combine to form the brachiocephalic vein immediately posterior the sternoclavicular joint. At this juncture there are usually two valve cusps within the terminal portion of the SCV. These may interfere with guide-wire passage during cannulation. On the right, the angle at which the SCV joins the IJV is very nearly 90 degrees. This can predispose a guide wire to pass cephalad into the IJV during insertion, particularly when the curve of the J-wire tip is oriented concave-upward. Some reports that suggest that shrugging the shoulders during insertion of the guidewire on the right may open the angle slightly, facilitating caudal passage of the wire. On the left, the brachiocephalic vein is oriented almost in-line with the terminus of the SCV and guidewire passage into the superior vena cava is much more consistent.
The SCV most commonly receives a single venous tributary, the external jugular vein (EJV), in its mid-portion near the top of its arc posterior to the clavicle. Less commonly, it also receives the transverse cervical and suprascapular veins. On the left the SCV receives the thoracic duct as it joins with the IJV. Injury of the thin-walled thoracic duct can occur during insertion or redirection of the needle on this side, resulting in the serious complication of chylothorax.
On both sides, when the SCV lies in its most common position superficial to the ASM, the posterior wall of the vein lies in close apposition to the phrenic nerve as it passes down the lateral margin of the muscle. The nerve is vulnerable to injury during needle insertion and redirection.
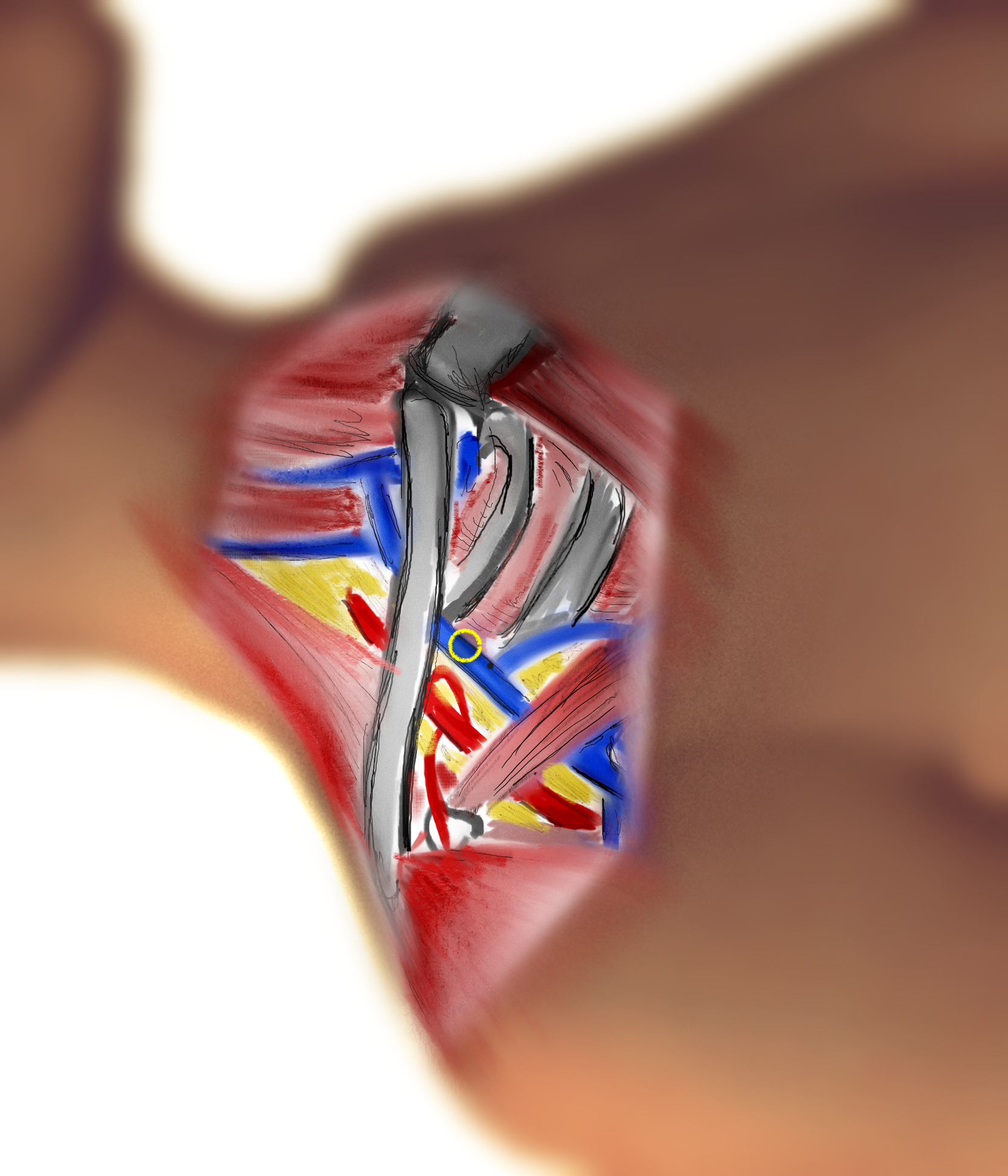
Parasagittal sectional images of the upper thorax and root of the neck best demonstrate the relative positions and anatomical relationships of the subclavian vessels and surrounding structures. In the following figure adapted from (Kitigawa, et al. Anesthesiol 2004; 101(6): 1308, Fig 2), the left-hand column shows images at the level of the clavicular head of the sternocleidomastoid muscle. The right-hand column shows images at the level of the mid-clavicle. Each row shows the relative positions of the vessels and surrounding structures with the ipsilateral shoulder elevated, neutral, and depressed, respectively. Note that the SCV and SCA are more closely related to the clavicle in the medial images, and that the first rib forms a “backstop” at both locations. Note also that a shoulder-elevated position appears to offer greater exposure of the SCV by the infraclavicular approach.
Approaches
Two approaches are employed in SCV cannulation: Infraclacvular and supraclavicular. Each approach can be performed using visible and palpable surface landmarks. Each approach is greatly augmented by ultrasound visualization but there are uncommon circumstances where time may not permit the use of sonographic guidance and landmark methods must suffice. In particular, central venous access during the resuscitation of trauma patients with critical hemodynamic compromise may require cannulation based on surface landmarks. The infraclavicular approach is the most common due to familiarity and because it does not require removal of cervical immobilization. However, this approach can be hampered by the overlying clavicle and the multiple tissue layers that must be traversed en route to the target. The infraclavicular approach is also extremely difficult or impossible during CPR. The supraclavicular approach accesses the vein at a much more superficial location than the infraclavicular approach, and is less likely to be complicated by SCA puncture. It can be performed with some difficulty during CPR, but cannot be accomplished with a cervical collar in place. Studies exist that argue both ways regarding the relative incidence of pneumothorax with each method.
Infraclavicular Approach
The infraclavicular approach attempts to exploit the close anatomical relationship between the posterior surface of the clavicle and the SCV, where the vein is immobile and predictable in location. However, the clavicle can also be the principal impediment to reaching the vein, potentially deflecting the needle posteriorly during insertion or tethering the needle if it traverses its periosteum or the fascia of the closely applied SCM. Different needle insertion points are advocated by different authors, though most favor skin puncture 1 cm caudal to the junction of the medial- and middle-thirds of the clavicle (indicated by the yellow circle in the images to the right). At this point, the vein will be tightly related to the deep surface of the clavicle and the first rib will lie deep to the SCV at the point of puncture, acting as a “backstop” that reduces the possibility of pleural puncture.
The needle is directed medially toward the index fingertip of the non-dominant hand which is placed in the suprasternal notch.
The needle should be kept in the coronal plane (parallel to the floor) to further reduce the possibility of pleural puncture.
The thumb of the non-dominant hand can be used to depress the hub of the needle to facilitate passage of the needle tip beneath the clavicle.
As the needle is advanced, vacuum is maintained on the syringe plunger. Free flow of dark blood heralds puncture of the vein.
The depth of the needle at which the vein is encountered is usually between 3 cm and 4 cm unless the patient is extremely muscular or has a high BMI.
The bevel of the needle (aligned with the mL scale on the syringe) is then rotated to face inferiorly, and the guide wire is passed with the convex curve of the tip facing cephalad. After passage of the dilator over the guide wire, the catheter is placed by Seldinger technique with the tip the superior vena cava. The depth if insertion on the right is often stated to be 14 cm, while that on the left is 17 cm. It should be obvious that these numbers may vary for individuals of different stature. The surface projection of the target point is slightly caudal to the angle of Louis (sternomanubial joint) near the second sternocostal joint. The depth can be empirically determined by holding the catheter in a curve from the planned skin puncture site to this target after the patient has been prepped and draped.
More lateral skin puncture sites (Mid-clavicle, junction of the middle- and lateral-thirds of the clavicle, deltopectoral groove) have the advantage of the skin and soft tissue being more easily depressed at these locations, easing passage of the needle toward the sternal notch. In addition, the pulsations of the SCA can often be felt as the inferior margin of the clavicle is explored, providing an additional landmark. These locations have the disadvantage of targeting the vein when it is actually the terminal portion of the AV rather than the SCV. If successful, accessing the vein at this more lateral location is of little or no clinical consequence. However, the vein is less closely related in location to the clavicle in this area and therefor somewhat more difficult to find. Further, the vein is encountered at a point where the first rib offers no protection against pneumothorax, and the anterior scalene muscle does not provide a “spacer” between the SCV and SCA.
At the favored, medial insertion point, the needle traverses skin, subcutaneous fat, fibers of the platysma, the lateral margin of the clavicular head of the pectorals major muscle, and likely the subclavius muscle before encountering the vessel.
If the SCV is missed during insertion and the needle passes more medially, it may strike the SCA as it arcs from the innominate artery. The needle may even reach the airway. Prior to needle insertion, determine the maximal, safe depth of insertion and do not violate that depth.
Supraclavicular approach
The supraclavicular subclavian approach attempts to enter the SCV at, or just medial to, the point the vein reaches the highest point of its arc posterior to the clavicle. At this point the vein is very superficial in comparison to the infraclavicular location. Layers traversed to reach the SCV here are only skin, subcutaneous fat, and the thin transverse cervical fascia. The depth to the vein usually 1 cm to 3 cm. Landmarks for the skin puncture site are lines 1 cm lateral to the posterior margin of the clavicular head of the sternocleidomastoid muscle, and 1 cm posterior to the superior border of the clavicle. The puncture site is the crossing point of these lines.
The needle is aimed just caudal to the contralateral nipple, or at an angle of about 45 degrees off the mid-sagittal plane (bisecting the angle formed between the clavicle and sternocleidomastoid muscle.
The syringe is then depressed so the needle passes at an upward angle of 10 to 15 degrees as it is inserted. This approach directs the needle away from the SCA and pleural dome as the depth of insertion increases.
Needle insertion that misses the SCV and passes more deeply will eventually strike the ipsilateral sternoclavicular joint. The Seldinger technique employed for guidewire and catheter insertion is identical to that in the infraclavicular apporoach. Catheter insertion depth is similar to that in the alternative approach; 14 cm on the right and 18 cm on the left.