Air Care Series: Machines Inside of Machines - CPR in flight
/Introduction:
Helicopter Emergency Medical Services (HEMS) often transport patients who are critically ill and at risk for cardiac arrest. The management of patients who suffer cardiac arrest in flight, and specifically the delivery of high-quality cardiopulmonary resuscitation (CPR), presents a particular challenge for HEMS providers. The depth and rate of closed chest compressions directly affect patient survival (1), however space limitations in many airframes make performance of quality compressions extremely difficult. (2,3) The confined space may also make changing compressors impractical, forcing a single provider to perform manual compressions for an extended period of time (2), while significant decay in the quality of closed chest compressions occurs in as little as two minutes. (4,5) Prolonged pauses in chest compressions are also associated with decreased survival. (6) For safety reasons, FAA regulations require crew members to be seated and secured during critical phases of flight, including takeoff and landing, however providers must typically be out of safety restraints to deliver adequate compressions. Continuing manual CPR during take-off or landing exposes crew members to increased risk, and potentially places them in violation of FAA regulations; alternatively, interrupting chest compressions compromises the resuscitation effort.
Mechanical CPR Devices:
Mechanical CPR devices have emerged as a potential alternative to manual chest compressions. The two devices in widest use are the AutoPulse and the Lund University Cardiopulmonary Assist System (LUCAS). The AutoPulse is battery-powered and consists of a rigid backboard and a load-distributing band that encircles a patient’s chest, delivering compressions by rhythmically constricting. The LUCAS device employs a silicone rubber suction cup mounted on a piston that compresses the chest against a rigid backplate; the LUCAS-1 device was pneumatic, while the newer LUCAS-2 and LUCAS-3 are battery-powered.
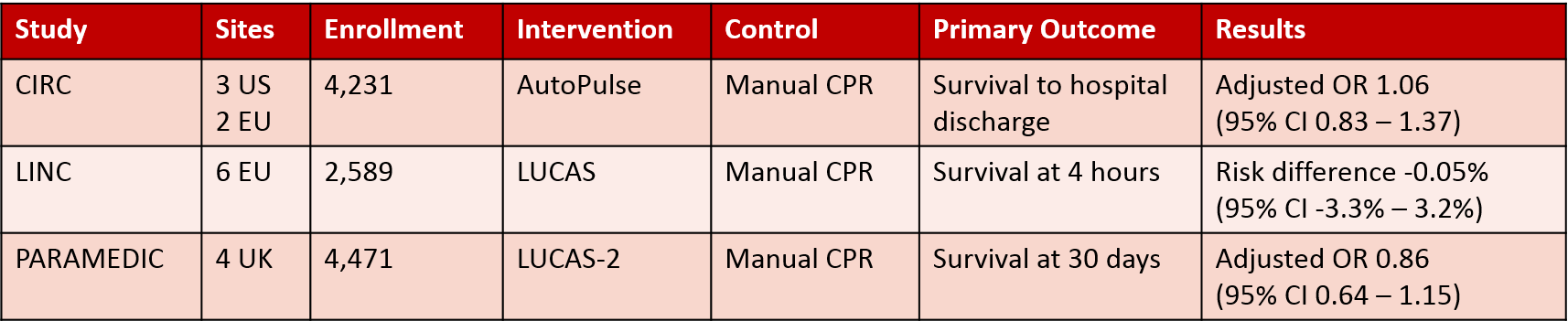
Three large, randomized-controlled trials have examined the efficacy of mechanical CPR relative to manual compressions in patients suffering non-traumatic out-of-hospital cardiac arrest. The CIRC trial, conducted across several US and European sites, found no difference in survival to hospital discharge or in rates of injury between patients treated with the AutoPulse and those who received manual compressions. (7) The multi-center European LINC trial demonstrated equivalent outcomes in patients treated with the LUCAS device and manual CPR, including survival at 4 hours and neurologically-intact survival at 1 and 6 months. (8) The UK-based PARAMEDIC trial found no difference in 30-day survival or in serious adverse events between patients treated with the LUCAS-2 device versus manual compressions. (9) Notably, the quality of manual CPR reported in all three studies (as measured by compression fraction, or the percentage of time compressions were performed during the resuscitation) was markedly higher than has previously been reported for out-of-hospital cardiac arrest. (10) A subsequent Cochrane review concluded that “CPR protocols involving mechanical chest compression devices produce similar clinical outcomes compared to manual CPR protocols involving very high-quality chest compressions.” (11)
Given this, mechanical CPR devices may be of particular value in the helicopter transport setting where performing very high quality chest compressions is difficult to impossible; mechanical CPR devices can deliver high quality compressions in limited space, unaffected by rescuer fatigue, and while crew members remain seated and secured. The feasibility of employing both the AutoPulse and LUCAS in helicopters has been examined in manikin studies as well as in clinical practice. Gässler et. al. found both devices could be loaded/unloaded and used without difficulty in a BK-117. The LUCAS-2 met all guidelines for compression rate, depth, and hands-off time during a simulated arrest scenario; the AutoPulse failed to meet guidelines for depth and rate; and performing adequate manual compressions was characterized as “barely possible” during loading, unloading, and simulated flight. (2) However, the AutoPulse does chest compressions different from manual chest compressions, because it squeezes the entire chest in a circumferential fashion. As such, good blood flow can be demonstrated from AutoPulse CPR without meeting traditional depth and rate guidelines from the AHA. Putzer et al. similarly found that, compared to manual chest compressions, LUCAS-delivered compressions were of higher quality with less hands-off time in a simulated resuscitation, also performed in a BK-117, although time to defibrillation was higher in the LUCAS group due to the time required for device application. (12) In terms of patient outcomes, a retrospective study of out-of-hospital cardiac arrest patients in Japan found a significant increase in ROSC (30.6% vs. 7.0%, p = 0.007) after the introduction of the AutoPulse device in a physician-led HEMS system utilizing EC145s; there was no difference in survival to hospital discharge, however. (13)
While these studies suggest mechanical CPR devices are a safe an effective option for in-flight CPR, they all specifically addressed scenarios in which mechanical CPR was initiated on scene, before patients were loaded for transport. In the case of a cardiac arrest occurring mid-flight, deploying either the AutoPulse or LUCAS would be prohibitively difficult and time-consuming. For a mechanical CPR device to be of utility in an in-flight arrest, it would need to be pre-loaded prior to take-off and ideally at the time the patient is transferred to the stretcher. This could be done based on pre-determined indicators of hemodynamic instability, for patients at risk of re-arrest following ROSC, and/or on the basis of provider gestalt.
At Air Care, we do not typically fly patients who suffer refractory cardiac arrest prior to transport. There are several circumstances, however, in which transport of a patient with ongoing CPR should be considered. Good neurologic recovery is possible in cases of hypothermic cardiac arrest, even with prolonged low- or no-flow times. (14) A number of case reports describe the use of continuous mechanical CPR during HEMS transport to ECMO-capable facilities, allowing extracorporeal rewarming of patients following accidental hypothermic arrest. (15-18) In at least two of these cases (17,18), the patients survived without neurologic impairment, including one who received mechanical compressions for more than 3.5 hours.
In select patients, prolonged CPR may also serve as a bridge to percutaneous coronary intervention (PCI) or extracorporeal cardiopulmonary resuscitation (ECPR). The 2015 CHEER trial reported a neurologically-intact survival rate of 45% among patients with refractory out-of-hospital cardiac arrest who were treated with AutoPulse-delivered compressions, therapeutic hypothermia, and ECPR, which was followed by emergent PCI in patients with suspected coronary artery occlusion. (19) As the time interval between cardiac arrest and initiation of ECPR is an independent predictor of survival (20), rapid HEMS transport of patients with refractory cardiac arrest could provide clinically-significant benefit to patients who arrest in locations remote from an ECMO-capable facility. (21) In addition, Forti et al. reported the case of a euthermic patient with refractory cardiac arrest who was transported by HEMS with LUCAS-assisted CPR, underwent PCI with ongoing mechanical compressions, and survived neurologically-intact after 115 minutes in cardiac arrest (22); this suggests that, in very select patients, there may be benefit to transport under continuous compressions even if ECPR is not available.
Conclusion:
HEMS crews often care for patients at risk for cardiac arrest, however providing high quality CPR during helicopter transport is extremely challenging. Closed chest compressions performed in flight are often sub-optimal due to space limitations, rescuer fatigue, and safety considerations. Mechanical CPR devices are an alternative to manual chest compressions, producing equivalent clinical outcomes, that can be used during HEMS transport to improve CPR quality. To be of utility in an in-flight arrest, mechanical CPR devices must be pre-loaded on high risk patients as they cannot be quickly or safely deployed during transport. There are also select patients who may benefit from transport with ongoing CPR as a bridge to PCI or ECMO.
AUTHORed by KATHERINE CONNELLY, MD
Katherine Connelly, MD is a second year resident in the Department of Emergency Medicine.
Posted by ADAM GOTTULA, MD
Adam Gottula, MD is a third year resident in the Department of Emergency Medicine.
FACULTY EDITOR JUSTIN BENOIT, MD, MS
Justin Benoit, MD is an attending in the Department of Emergency Medicine and specializing in cardiac arrest research and EMS.
ReferenceS:
1. Talikowska M, Tohira H, and Finn J. Cardiopulmonary resuscitation quality and patient survival outcomes in cardiac arrest: A systematic review and meta-analysis. Resuscitation. 2015;96:66-77.
2. Gässler H, Kümmerle S, Ventzke M, et al. Mechanical chest compression: An alternative in helicopter emergency medical services? Intern Emerg Med. 2015;10:715-720.
3. Hoffman DB, Figeuroa A, Shaw M, et al. The efficacy of chest compressions in the Bell 407. Air Med J. 2019;38:281-284.
4. Hightower D, Thomas SH, Stone CK, et al. Delay in quality of closed-chest compressions over time. Ann Emerg Med. 1995;26(3):300-303.
5. Sugerman NT, Edelson DP, Leary M, et al. Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: A prospective, multicenter study. Resuscitation. 2009;80:981-984.
6. Brouwer TF, Walker RG, Chapman FW, et al. Association between chest compression interruptions and clinical outcomes of ventricular fibrillation out-of-hospital cardiac arrest. Circulation. 2015;132:1030-1037.
7. Wik L, Olsen J, Persse D, et al. Manual vs. integrated automatic load-distributing band CPR with equal survival after out of hospital cardiac arrest. The randomized CIRC trial. Resuscitation. 2014;85:41-748.
8. Rubertsson S, Lindgren E, Smekal D, et al. Mechanical chest compressions and simultaneous defibrillation vs conventional cardiopulmonary resuscitation in out-of-hospital cardiac arrest. JAMA. 2014;311(1):53-61.
9. Perkins GD, Lall R, Quinn T, et al. Mechanical vs. manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): A pragmatic, cluster randomized controlled trial. Lancet. 2015;385:947-955.
10. Wik L, Kramer-Johansen J, Myklebust H, et al. Quality of cardiopulmonary resuscitation in out-of-hospital cardiac arrest. JAMA. 2005;293(3):299-304.
11. Wang PL and Brooks SC. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev. 2018;8.
12. Putzer G, Braun P, Zimmerman A, et al. LUCAS compared to manual cardiopulmonary resuscitation is more effective during helicopter rescue: A prospective, randomized, crossover manikin study. Am J Emerg Med. 2013;31:384-389.
13. Omori K, Sato S, Sumi Y, et al. The analysis of efficacy for AutoPulse system in flying helicopter. Resuscitation. 2013;84:1045-1050.
14. Walpoth BH, Walpoth-Aslan BN, Mattle HP, et al. Outcome of survivors of accidental deep hypothermia and circulatory arrest treated with extracorporeal blood warming. N Engl J Med. 1997;337(21):1500-1505.
15. Tazarourte K, Sapir D, Laborne FX, et al. Refractory cardiac arrest in a rural area: Mechanical chest compression during helicopter transport. Acta Anaesthesiol Scand. 2013;15:71-76.
16. Pietsch U, Lischke V, Pietsch C, et al. Mechanical chest compressions in an avalanche victim with cardiac arrest: An option for extreme mountain rescue operations. Wilderness Environ Med. 2014;25:190-193.
17. Forti A, Brugnaro P, Rauch S, et al. Hypothermic cardiac arrest with full neurologic recovery after approximately nine hours of cardiopulmonary resuscitation: Management and possible complications. Ann Emerg Med. 2019;73(1):52-57.
18. McCormack J and Percival D. HEMS advanced trauma team retrieval of a patient with accidental hypothermic cardiac arrest for ECMO therapy. Resuscitation. 2016;105:e23.
19. Stub D, Bernard S, Pellegrino V, et al. Refractory cardiac arrest treated with mechanical CPR, hypothermia, ECMO, and early reperfusion (the CHEER trial). Resuscitation. 2015;86:88-94.
20. Kim DH, Kim JB, Jung S, et al. Extracorporeal cardiopulmonary resuscitation: Predictors of survival. Korean J Thorac Cardiovasc Surg. 2016;49:273-279.
21. Rauch S, Strapazzon G, Broadman M, et al. Implementation of a mechanical CPR device in a physician-staffed HEMS: A prospective observational study. Scand J Trauma Resusc Emerg Med. 2018;26:36.
22. Forti A, Zilio G, Zanatta P, et al. Full recovery after prolonged cardiac arrest and resuscitation with mechanical chest compression device during helicopter transportation and percutaneous coronary intervention. J Emerg Med. 2014;47(6):632-634.