Annals of B Pod - Acetaminophen Overdose
/History of Present Illness
The patient is a young female with history of depression and sleeve gastrectomy who presents to the emergency department after ingesting fifty 500 mg acetaminophen tablets (25 g) nine hours prior to presentation in a suicide attempt. She reports multiple episodes of non-bloody emesis that began one hour after the ingestion, without visible pill fragments in the emesis. The patient additionally reports left upper quadrant pain and fatigue. She denies other co-ingestions.
Past medical history: Chronic headaches, depressive episode 6 years ago with auditory hallucinations and suicidal ideation
Past surgical history: Laparoscopic sleeve gastrectomy
Medications: None
Allergies: No known drug allergies
Social history: None pertinent
Physical Exam
Vitals: T 98.7 HR 74 BP 124/84 RR 18 SpO2 100% on RA
The patient is oriented to person, place, and time. Abdomen is distended with tenderness to palpation in the left upper quadrant without rebound tenderness. Skin is dry without rashes, erythema, diaphoresis, or pallor. The patient’s remaining physical exam is unremarkable.
Diagnostics
AST 91 ALT 97 Alk Phos 79 T. Bili 0.7 D. Bili 0.2 Lipase 13
Ammonia 49
PT 17 INR 1.3
VBG: pH 7.46 PCO2 27 PO2 34 HCO3 19 BE -3.2
Lactate 0.7
Serum Pregnancy Test Negative
Acetaminophen (drawn approximately 10 hours after ingestion): 125 ug/mL
Salicylate < 3 μg/mL
HCV & HBV Ab negative
Hospital Course
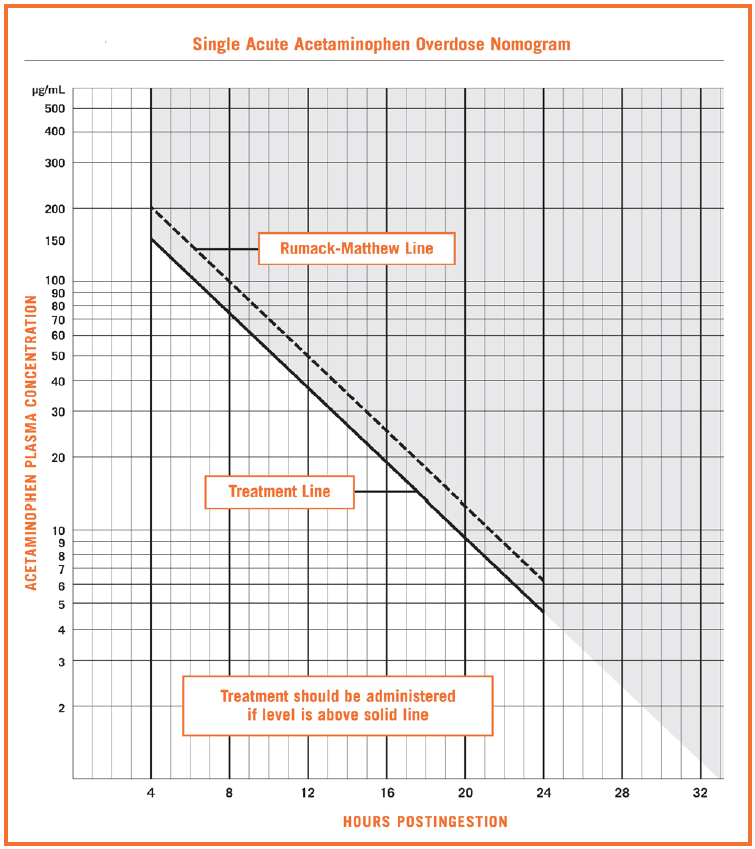
N-acetylcysteine (NAC) therapy was started given that the patient’s serum acetaminophen concentration was 125 ug/mL, 10 hours post- ingestion, above the treatment threshold on the Rumack-Matthew nomogram. She was evaluated in the ED by the psychiatry consult team and was deemed appropriate for outpatient psychiatric follow up. The patient was then admitted to the Hospital service for ongoing NAC administration and trending of labs. The patient suffered intractable vomiting that was refractory to antiemetic therapy and developed right upper quadrant pain on hospital day (HD) 1. On HD2, her liver enzymes peaked with AST 3908, ALT 4235, and INR 2.0, at which time the patient was transferred to the MICU. There, the patient received vitamin K supplementation for her elevated INR in conjunction with continuous NAC infusion per the antidotal protocol until HD3, when her liver enzymes began to downtrend. Given improvement in her liver function assays and stable vital signs, the patient was subsequently transferred back to the medicine floor. Due to concerns for impending liver failure, she was evaluated by the transplant social worker, and consents were signed to begin pre-operative assessments for a liver transplant. On HD4, however, the patient refused further therapy and workup and signed out of the hospital against medical advice.
Acetaminophen Overdose
Pathophysiology
N-acetyl-para-aminophenol (acetaminophen, APAP) is widely used in the United States for its analgesic and antipyretic properties, and is widely available over the counter in an oral formulation. The mechanism of action of acetaminophen remains unclear, but is postulated to inhibit COX pathways in the central nervous system inhibiting synthesis of prostaglandins. [1] The maximum recommended APAP dose in adults is 4 g/day and 50-75 mg/kg/day in children. In therapeutic doses, APAP is metabolized in the liver, where it is converted to inactive glucuronide and sulfate conjugates (90-95%), which are excreted in the urine. [2] The remaining fraction of APAP (5-10%) is metabolized via the cytochrome P-450 CYP2E1 pathway to a reactive metabolite called N-acetyl-p-benzoquinone imine (NAPQI). In supratherapeutic doses of APAP, the typical metabolism mechanism is overwhelmed and more and more APAP is shunted into the NAPQI pathway. NAPQI is highly reactive due to its free radical properties and causes oxidative damage to hepatocytes. In therapeutic doses of APAP, NAPQI is metabolized to an inactive metabolite (APAP-GSH) by binding the sulfhydryl group of glutathione present in hepatocytes. However, at toxic doses of APAP, the liver’s glutathione reserves are rapidly depleted, causing NAPQI to accumulate in the perivenous hepatic cells where it induces DNA fragmentation, mitochondrial dysfunction, and hepatocyte necrosis. Hepatic damage begins when about 70% of glutathione is depleted. In a healthy, 70 kg patient with normal liver function, this typically does not occur until exposure exceeds 16 g of APAP. [3] However, for patients with existing liver dysfunction, malnutrition, concurrent use of P450 inducing agents (e.g., rifampin, phenobarbital, phenytoin, or carbamazepine) or other hepatotoxic medications (INH, TMP-SMX, zidovudine), the toxic threshold may be significantly reduced.
Testing
In 1975, Drs. Barry H. Rumack and Henry Matthew created a nomogram to outline treatment thresholds for serum APAP levels measured between four and twenty-four hours after ingestion, as this is when serum levels typically reach their peak. [4] At the request of the FDA in 1981, a second line was added to include a 25% margin of error to account for variability in serum APAP measurements or uncertainty about timing of ingestion. [5] This second line has now been adopted as the standard for treatment threshold on the nomogram, which begins at serum APAP concentrations of greater than 150 ug/mL at 4 hours post-ingestion. Concentrations below this line indicate low risk for hepatotoxicity. Some variations of the nomogram contain a “massive intoxication” threshold, which resembles a treatment line that begins at 300 ug/mL at 4 hours and decreases at the same slope of the standard line to 24 hours. This designation carries different treatment goals, which will be discussed in the next section. Serum acetaminophen levels obtained prior to the four-hour threshold are typically viewed as unreliable as the drug may still be in transit within the stomach and the assay may not reflect a peak measurement. Importantly, clinicians must pay attention to the units of their institution’s serum APAP assay and verify that they correlate with the units on the Rumack-Matthew Nomogram as to avoid over- or under-estimating the treatment threshold.
Despite its widespread use, the Rumack-Matthew Nomogram does present some limitations. The nomogram cannot be used for multiple APAP ingestions and is only validated for one acute ingestion presenting within twenty-four hours. As previously mentioned, concurrent use of medications that induce P450 metabolism, or use of hepatotoxic medications may allow clinically significant toxicity to occur at levels below the treatment threshold. Lastly, altered pharmacokinetics including extended-release APAP formulations or alterations to gastric emptying (stemming from concomitant opioid use or gastroparesis, for example) should preclude the use of the nomogram due to unpredictable variations in the rate of APAP absorption. [6] There are data to suggest that sleeve gastrectomy and other bariatric surgeries may increase gastrointestinal motility and thus potentially increase APAP bioavailability. The clinical relevance of this finding in the setting of toxic ingestion is still uncertain. [7-9] It has been demonstrated that extended release formulations of APAP exhibit similar rates of elimination as the immediate release form after four-hours. However, there are case reports to suggest that delayed absorption and peak concentrations after four hours can also occur. [10-12] If there is concern for extended release formulation, serial testing should be considered. [13]
Treatment
Treatment of acute APAP overdoses should be prompted by the serum APAP level and never by estimated ingestion quantity, as estimations have been demonstrated to correlate poorly with serum levels. [14-15] For patients with known single ingestion and reliable ingestion time less than 24-hours, the Rumack-Matthew Nomogram should be used to determine the need for treatment. For patients with unknown ingestion time, history of alcoholism or malnutrition, use of synergistic drugs (P450 inducers or hepatotoxins), or delayed gastric emptying, some treatment approaches advocate for empiric NAC treatment - given the unpredictable alterations to APAP absorption and metabolism - while trending of serum APAP concentrations and ALT. Treatment with NAC beyond 24-hours is controversial, but some argue that there is a role for NAC in patients with ALT > 50 with delayed presentation.
NAC serves as the primary treatment for acute APAP overdose, and multiple dosage protocols exist, including a 72-hour oral protocol and the 20-hour IV protocol. The oral regimen includes a loading dose of 140 mg/kg, and is followed by 70 mg/kg every four hours for a total of 17 doses. This can be difficult to endure for patients, as it may cause nausea, has a foul odor and is often not well tolerated by patients, and therefore the IV regimen is more commonly employed than the PO regimen. The 20-hour IV regimen includes an initial loading dose of 150 mg/kg over one hour, followed by an infusion of 50 mg/kg over four hours, and finally a dose of 100 mg/kg over 16 hours. Treatment should be continued at 6.25 mg/kg per hour IV until the serum APAP concentration is undetectable, the ALT is clearly decreasing or within the normal range, and the INR < 2.
For patients with massive intoxication (four-hour level above 300 ug/mL or suspected ingestions of greater than 500 mg/kg), there is data to support increased dosing of NAC. These dosing regimens likely will not change ED management, as the first two doses are unchanged, corresponding to the first five hours of treatment. The third dose is increased to 12.5 mg/kg/hr to 25 mg/kg/hr depending on the four-hour APAP concentration. [16]
Some patients may experience an anaphylactoid reaction with administration of NAC that can manifest as flushing, urticaria, angioedema, and potentially respiratory distress and hypotension. These reactions occur within the first six hours of administration, most often within the first two hours. [17] NAC should only be held in the setting of respiratory distress, hypotension or angioedema, and antihistamines and steroids can be considered for symptomatic treatment.
Activated charcoal should be considered as adjunctive therapy for patients that present within 1-3 hours of ingestion and are able to protect their airway. Activated charcoal provides the greatest benefit to those presenting after massive APAP ingestions. [18] Dialysis is able to remove APAP and NAPQI from circulation. The Extracorporeal Treatment in Poisoning (EXTRIP) suggests that dialysis is recommended if the patient has altered mental status, metabolic acidosis, elevated lactate, and serum APAP concentration of greater than 900 mg/dL, with or without NAC administration. [18] For patients on hemodialysis, the dose of NAC needs to be increased; there are no prospectively validated algorithms and alternative dosing should be administered under the direction of local poison control experts. Fomepizole, a cytochrome P450 inhibitor, can be considered a potential adjective therapy given its ability to shunt APAP metabolism away from NAPQI and towards more benign metabolites; however, larger studies are required to validate its efficacy. [19]
Prognosis
APAP toxicity is the leading cause for fulminant hepatic failure in the United States, accounting for approximately 39% of all cases. [20] Acute APAP overdose carries high morbidity and mortality if it goes undiagnosed or is not treated in a timely fashion. In a 1995 review of 295 cases of liver transplant for acute liver failure, APAP toxicity was the leading cause for liver transplantation, representing 20% of that cohort. [21] Fortunately, 65% of patients with acute APAP toxicity survive the event without need for transplantation if appropriate treatment is provided early. [22]
Summary
Acute APAP overdose is a disease with high morbidity and mortality. The Rumack-Matthew Nomogram should be utilized to guide treatment decisions, though providers should be aware of its limitations, particularly given the potential for inaccurate timing of ingestion, multiple ingestions, existing liver dysfunction, GI dysmotility, or concurrent use of hepatotoxic or P450 inducing medications. NAC antidotal therapy is safe and effective and should be employed early in patients with elevated serum levels or evidence of organ dysfunction. Providers should familiarize themselves with their institutional treatment protocols. Patients may experience anaphylactoid reaction to NAC; as this is not a true allergic response, patients may be treated symptomatically with antihistamines and continuation of NAC therapy if the patient is stable. Adjunctive therapies, including hemodialysis, activated charcoal, and fomepizole, may be employed at the discretion of toxicologists or poison control experts in the context of massive ingestions.
AUTHORED BY Arthur Broadstock, MD
Editing BY the Annals of B Pod Editors
References
Smith HS. Potential analgesic mechanisms of acetaminophen. Pain Physician. 2009;12(1):269-280.
Mazaleuskaya LL, Sangkuhl K, et al. PharmGKB summary: Pathways of acetaminophen metabolism at the therapeutic versus toxic doses. Pharmacogent Genomics. 2015;25(8):416-426.
Rumack BH. Acetaminophen Hepatotoxicity: The First 35 Years. J Toxicol Clin Toxicol. 2002; 40(1):3-21.
Rumack BH, Matthew H. Acetaminophen Poisoning and Toxicity. Pediatrics. 1975;(55):871-876.
Rumack BH, Peterson RC, Koch GG, Amara IA. Acetaminophen overdose: 662 cases with evaluation of oral acetylcysteine treatment. Arch Intern Med. 1981;141(3):380-385.
Raffa RB, Pergolizzi JV, Taylor R, et al. Acetaminophen (Paracetamol) Oral Absorption and Clinical Influences. Pain Practice. 2014; 14(7):668-677
Sioka, E. Tzovaras, G; Perivoliotis, et al. Impact of Laparoscopic Sleeve Gastrectomy on Gastrointestinal Motility. Gastroenterology Research and Practice. 2018; doi: 10.1155/2018/4135813
Porat D, Markovic M, Zur M, et al. Increased Paracetamol Bioavailability after Sleeve Gastrectomy: A Crossover Pre- vs. Post-Operative Clinical Trial. Journal of Clinical Medicine. 2019; 8(11):1949.
Ardila-Hani A, Soffer, E.E. Review article: The impact of bariatric surgery on gastrointestinal motility. Alimentary Pharmacology & Therapeutics. 2011; 34(8):825–831.
Bizovi KE, Aks SE, Paloucek F, Gross R, Keys N, Rivas J. Late Increase in Acetaminophen Concentration After Overdose of Tylenol Extended Relief. Ann Emerg Med. 1996;28(5):549-551.
Cetaruk EW, Dart RC, Horowitz RS. Extended-Release Acetaminophen Overdose. JAMA. 1996;275(9):686.
Douglas DR, Smilkstein MJ, Sholar JB. Overdose with ‘extended-relief’ acetaminophen: is a new approach necessary? Acad Emerg Med . 1995;(2):397-398.
Cetaruk EW, Dart RC, Hurlbut KM, Horowitz RS, Shih R. Tylenol Extended Relief Overdose. Ann Emerg Med. 1997;30(1):104-108.
Ambre J, Alexander M. Liver toxicity after acetaminophen ingestion. Inadequacy of the dose estimate as an index of risk. JAMA. 1977;238(6):500.
Read RB, Tredger JM, Williams R. Analysis of factors responsible for continuing mortality after paracetamol overdose. Hum Toxicol. 1986;5(3):201.
Hendrickson R. What is the most appropriate dose of N-acetylcysteine after massive acetaminophen overdose? Clin Toxicol. 2019;57(8):686-691.
Yarema M, Chopra P, Sivilotti M, et al. Anaphylactoid Reactions to Intravenous N-Acetylcysteine during Treatment for Acetaminophen Poisoning. J Med Toxicol. 2018;14(2):120-127.
Gosselin S, Juurlink D, Kielstein J, et al. Extracorporeal treatment for acetaminophen poisoning: recommendations from the EXTRIP workgroup. Clin Toxicol. 2014;52(8):856-867.
Shah KR, Beuhler MC. Fomepizole as an Adjunctive Therapy in Severe Acetaminophen Toxicity. Am J Emerg Med. 2020;38(2):410.e5-410.e6.