Annals of B-Pod: Serotonin Syndrome
/The patient is a female in her 20s with a past medical history of depression who presents to the Emergency Department via EMS after an overdose. EMS reports that the patient’s friends called 911 after she ingested approximately thirty 150 mg venlafaxine extended release tablets along with alcohol in a suicide attempt approximately four hours prior to presentation.
En route to the hospital, EMS reported one episode of emesis as well as tachycardia in the 150s with otherwise normal vital signs. The patient confirms that she intentionally overdosed in a suicide attempt, but immediately regretted this decision and began to force herself to vomit, regurgitating approximately 10 pills. She states that she has had several stressors. She currently reports blurred vision as well as anxiety, but denies coingestion of any other substances, chest pain, shortness of breath, or abdominal pain.
Vitals: T 38.0 HR 167 BP 106/85 RR 24 SpO2 98% on room air
Physical Exam: The patient is evaluated on the EMS stretcher and appears non-toxic with dried vomitus around her mouth. Cardiovascular exam is significant for marked tachycardia with no murmurs, rubs, or gallops appreciated. Her pulmonary exam shows moderate tachypnea with clear breath sounds bilaterally. Abdomen is soft and non tender. She displays frequent myoclonic jerking movements of the bilateral upper extremities. Her pupils are equally round and reactive and she is alert and oriented to person, place, and time. She is grossly moving all four extremities with 3+ knee and ankle reflexes bilaterally and myoclonus of the bilateral ankles.
Diagnostics
WBC 27.0 Lactate 20.0
Na 139 K 4.0 Cl 101 CO2 9 BUN 11 Cr 1.49
VBG pH 7.07 / CO2 38 / O2 46 / BE -17.6
Acetaminophen/salicylate levels negative
EKG: sinus tachycardia
Hospital Course
As the patient was being transferred from the EMS stretcher to her bed, she exhibited a generalized tonic clonic seizure. She was given 2 mg of lorazepam IM, and the seizure resolved after approximately 75 seconds. She was postictal for approximately 10 minutes before returning to baseline. Labs obtained after she seized revealed an anion gap metabolic acidosis likely secondary to lactic acidosis, as well as significant leukocytosis. Her physical exam was notable for a low grade temperature, tachycardia and myoclonus on exam, consistent with serotonin syndrome. Poison control was contacted, and recommended supportive therapy, and recommended cyproheptadine if there was clinical worsening. She became more somnelent and she was given an initial dose of 12 mg of cyproheptadine orally and was admitted to the MICU.
Approximately six hours after admission, the patient had another generalized tonic clonic seizure that was complicated by aspiration. She was subsequently intubated for hypoxia and airway protection. She went onto develop severe ARDS requiring paralysis and proning. Her course was also complicated by acute renal failure secondary to rhabdomyolysis requiring hemodialysis. On hospital day 14 she was extubated. She spent several additional days in the hospital before being transferred to an inpatient psychiatric facility on hospital day 22.
Serotonin Syndrome
Serotonin syndrome is a condition caused by increased serotonergic activity in the central nervous system. Patients may present with a broad range of symptoms such as anxiety and tremor in mild cases, or altered mental status, cardiovascular compromise, and seizures in severe cases.[1] Mild serotonin syndrome can occur as a side effect of normal medication use for depression or anxiety. Moderate to severe cases, however, are often due to medication interactions or intentional overdose, and can quickly become life threatening, making recognition and prompt treatment of this condition important for the emergency physician.
Serotonin is a neurotransmitter found in the central and autonomic nervous system. It is a derivative of tryptophan, and depression has been associated with decreased intra-synaptic levels of serotonin. Selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) decrease pre-synaptic reuptake of serotonin, increasing the intra-synaptic serotonin concentration.[4] They are primarily used for depression and anxiety disorders. These medications generally have a very benign side effect profile, with drowsiness, weight gain, and sexual dysfunction being the most common symptoms. However, when taken in large amounts such as in an overdose or when used in combination with other serotonergic medications, especially monoamine oxidase inhibitors (MAOIs) which inhibit the degradation of serotonin, SSRI use can lead to serotonin syndrome.[10]
SSRIs include medications such as citalopram, escitalopram, paroxetine, fluoxetine and sertraline, while SNRIs include the drugs duloxetine and venlafaxine. Other commonly prescribed drugs with significant serotonergic activity include tricyclic antidepressants, trazodone, buspirone, dextromethorphan, fentanyl, lithium, tramadol, meperidine, and metoclopramide. Recreational drug use can also lead to significant serotonin toxicity, with the most common culprits being cocaine, amphetamines, and designer drugs such as ecstasy and MDMA.
Overall, according to the National Poison Center Data System, a total of 2.2 million potentially toxic exposures to serotonergic medications were reported in 2013, resulting in over two thousand fatalities.[7] Less than 5% of these exposures came from antidepressant medications, and the majority of patients had minimal to no symptoms. However, 1% of SSRI overdoses resulted in life-threatening toxicity. As seen in this patient, symptoms can progress quickly.[1] Venlafaxine, the medication involved in this case, is associated with the highest mortality rate of all SSRI/SNRI overdoses.[8]
There is no specific test for serotonin syndrome or toxicity, making this a clinical diagnosis requiring a high level of provider suspicion. A history of serotonergic drug use in combination with signs of sympathetic nervous system activation (e.g., tachycardia, hyperthermia, diaphoresis, mydriasis) and CNS hypersensitivity (most commonly deep tendon hyperreflexia and myoclonus) suggests diagnosis of serotonin syndrome.[5]
The clinical presentation of serotonin syndrome has significant overlap with other toxidromes, and therefore obtaining a thorough medication history from the patient or family and friends is very helpful in making the diagnosis.[4] However, obtaining a complete medication list may not be possible in the Emergency Department, making the physical exam of the utmost importance. Patients will often present with spontaneous or inducible myoclonus, and may also exhibit tremor, hyperreflexia, ocular clonus or fever. A provider can test for inducible clonus at the bedside by quickly dorsiflexing the ankle and holding the foot in dorsiflexion. If several beats of myoclonic jerking can be felt or observed, this increases the likelihood of serotonin syndrome.
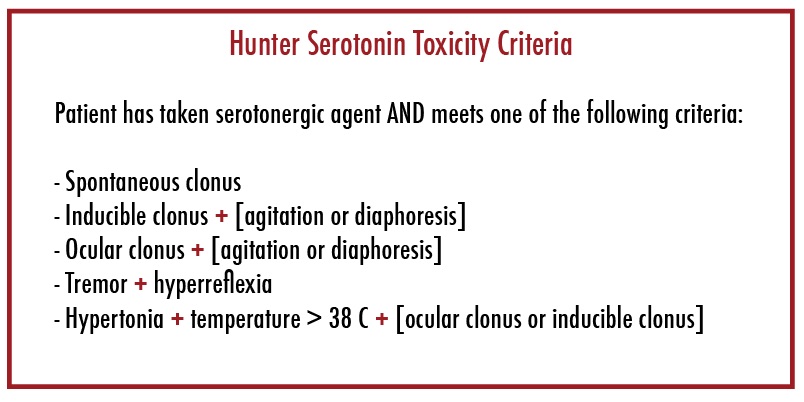
As this condition can often present subtly and progress rapidly, clinical evaluation tools are available to aide in the diagnosis of serotonin syndrome. The most current tool is the Hunter Serotonin Toxicity Criteria (Table 1), which is based on a retrospective analysis of prospective data collected from over 2000 patients who presented with an overdose of a serotonergic drug.[2] This tool was 84% sensitive and 97% specific for the diagnosis of serotonin syndrome. The decision tool requires that the patient has taken a serotonergic medication and exhibits one or several physical findings as described above.
This combination of signs and symptoms allows the clinician to readily differentiate serotonin syndrome from other similar conditions such as neuroleptic malignant syndrome, anticholinergic toxicity, and sympathomimetic toxicity. Patients with neuroleptic malignant syndrome will not exhibit clonus and will instead present with muscle rigidity.[6] Anticholinergic toxicity may appear similar to serotonin syndrome and should remain on the differential of a patient that presents with seizures after an overdose. However, these patients will classically have dry skin as opposed to the diaphoresis seen in serotonin syndrome and sympathomimetic toxicity. Serotonin syndrome and sympathomimetic toxicity can present similarly, but can be differentiated based on the presence of myoclonus.
While laboratory evaluation does not confirm the diagnosis, several abnormalities can be seen in cases of severe serotonin syndrome. These patients may have a severe metabolic acidosis secondary to lactic acid production, as well as leukocytosis and elevated creatinine kinase levels. In severe, life-threatening cases, serious laboratory derangements can develop, including disseminated intravascular coagulation and renal failure secondary to rhabdomyolysis.[5]
Management of serotonin syndrome is primarily supportive care, with fluid resuscitation and benzodiazepines as the mainstays of treatment. In mild cases, simply withdrawing the offending agent and treating with benzodiazepines for symptom control is adequate. If the patient is severely agitated, chemical sedation with benzodiazepines is the recommended treatment. Choice of benzodiazepine is often determined by provider preference. However, if the patient is actively seizing, a benzodiazepine with rapid onset such as 5-10 mg midazolam or 1-2 mg lorazepam should be chosen initially. Once the seizure has resolved, longer acting benzodiazepines can be given to reduce dosing frequency. Physical restraints should be avoided as this can contribute to rhabdomyolysis. Antipsychotics such as haloperidol should also be avoided, as these inhibit sweating and can worsen hyperthermia.[9]
In severe cases of serotonin syndrome that do not respond to supportive measures, cyproheptadine can be administered.[3] This antidote is primarily a H1 anti-histaminergic medication, but also has both anticholinergic and anti-serotonergic properties. An initial loading dose of 12 mg is followed by 2 mg every 2 hours until clinical improvement is demonstrated. Cyproheptadine is only available in oral form.
In severe cases, especially those in which the patient’s temperature is greater than 40 degrees or where airway protection is a concern due to seizure activity, endotracheal intubation should be performed. Rapid sequence intubation is safe in these patients. However, ketamine should be avoided as an induction agent due to the serotonergic activity of this drug, and succinylcholine should also be avoided if evidence of rhabdomyolysis is present.[1] Cyproheptadine may be administered via NG or OG tube in patients that require intubation. Ultimately, patients exhibiting signs of moderate to severe serotonin syndrome require close observation in an intensive care unit due to the potential for rapid worsening of symptoms.
Overall, the vast majority of patients who present following a serotonergic drug overdose will have mild to no symptoms, and can often be discharged home after a short period of observation. However, severe serotonin syndrome can be a rapidly progressive disease with significant morbidity and mortality, and emergency physicians should have a high clinical suspicion for this disease in overdose patients. Quick screening tests for myoclonus and hyperreflexia can be performed at the bedside, allowing providers to quickly establish a management plan. Patients can quickly progress from generalized tremors to full tonic-clonic seizures with the development of serious end-organ damage including acute renal failure. The best treatment strategies for these patients is early and aggressive supportive care with benzodiazepines and fluid resuscitation, and clinicians should have a low threshold for definitive airway management and admission to the ICU.
Authored by Michael Klaszky, MD Posted by Grace Lagasse, MD
References
- Boyer EW, Shannon M. The serotonin syndrome. N Engl J Med. 2005;352(11):1112-20.
- Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96(9):635-42.
- Graudins A, Stearman A, Chan B. Treatment of the serotonin syndrome with cyproheptadine. J Emerg Med. 1998;16(4):615-9.
- LoVecchio F, Mattison E. Atypical and Serotonergic Antidepressants. In: Tintinalli JE, Stapczynski J, Ma O, Yealy DM, Meckler GD, Cline DM. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e New York, NY: McGraw-Hill; 2016.
- Mason PJ, Morris VA, Balcezak TJ. Serotonin syndrome. Presentation of 2 cases and review of the literature. Medicine (Baltimore). 2000;79(4):201-9.
- Mills KC. Serotonin syndrome. A clinical update. Crit Care Clin. 1997;13(4):763-83.
- Mowry JB, Spyker DA, Cantilena LR, Mcmillan N, Ford M. 2013 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 31st Annual Report. Clin Toxicol (Phila). 2014;52(10):1032-283.
- Nickson, C. Serotonin Syndrome. Life in the Fastlane. http://lifeinthefastlane.com/ccc/serotonin-syndrome. February, 2017
- Nisijima K, Shioda K, Yoshino T, Takano K, Kato S. Diazepam and chlormethiazole attenuate the development of hyperthermia in an animal model of the serotonin syndrome. Neurochem Int. 2003;43(2):155-64.
- Ramsay RR, Dunford C, Gillman PK. Methylene blue and serotonin toxicity: inhibition of monoamine oxidase A (MAO A) confirms a theoretical prediction. Br J Pharmacol. 2007;152(6):946-51.