Consultant Corner: Acute Management of the Dislocated Shoulder, Part 1
/Shoulder dislocations are a bread-and-butter emergency medicine presentation—common, painful, and often deceptively complex. As the most frequently dislocated large joint, the shoulder demands a confident, systematic approach from every emergency physician. With a wide range of injury patterns, reduction techniques, and potential complications, mastering the management of shoulder dislocations is essential not only for successful reduction but also for preventing long-term morbidity. In this post which is PART ONE of the series, we will discuss background / epidemiology, anatomy, history and physical exam, and imaging techniques. PART TWO will discuss pain management with intra-articular lidocaine in addition to a variety of reduction techniques with included videos.
Background
The shoulder is the most commonly dislocated large joint accounting for over half of all dislocations (1,6,7). Overall, the incidence of shoulder dislocations ranges from 21.9-51.2 per 100,000 person-years (1-4). Recurrent dislocation is common with approximately 20% of patients having ≥1 episodes of recurrent dislocation following their initial dislocation event (2,5). Shoulder dislocations occur most commonly in young males aged 10-30 years followed by individuals aged 50-70 years (1,4).
Shoulder dislocations are classified as atraumatic or traumatic with approximately 96% of shoulder dislocations being secondary to trauma (1,8). Shoulder dislocations can be further classified by the direction of the humeral head in relation to the glenoid fossa. Anterior dislocations are the most common by far accounting for 97% of all shoulder dislocation followed by posterior dislocations (3%) then inferior dislocations (<1%) (1,8-10). Anterior dislocations can be further characterized based on the location of the humeral head in the subcoracoid or subglenoid space with subcoracoid dislocations occurring most commonly (1).
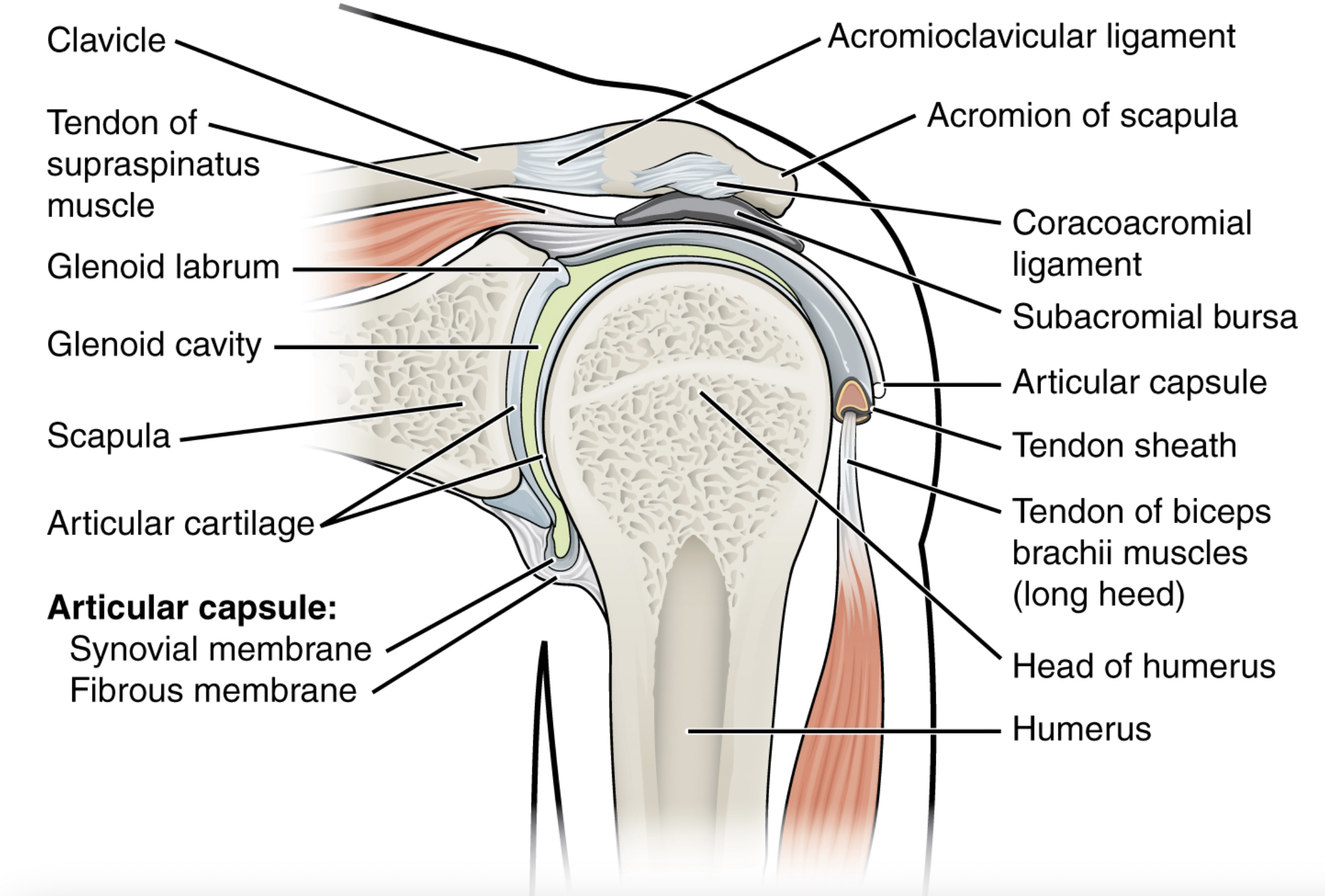
Anatomy
The shoulder joint consists of the articulation between the glenoid and the humeral head. The stability of the joint comes from multiple static and dynamic stabilizers, which include muscles, ligaments, and other structures. The glenoid fossa depth, labrum, glenohumeral ligaments, coracoacromial arch, and shoulder capsule make up the static stabilizers to provide stability to the shoulder at the extreme ends of motion. Throughout the shoulder’s range of motion, the deltoid, rotator cuff and periscapular musculature, and the long head of biceps tendon work to stabilize the shoulder as dynamic stabilizers (1).
The anatomy of the shoulder allows it to have the greatest arc range of motion throughout various planes compared to other joints in the body due to minimal articular contact (ability to translate) with only 25-30% of the humeral head articulating with the glenoid at any time (1,11). As a result, certain traumatic events can lead to a dislocation of the glenohumeral joint. Most traumatic shoulder dislocations are anterior dislocations; however, posterior and inferior dislocations can also occur. In anterior dislocations, at the time of injury, the arm is typically abducted and externally rotated when a force directed posteriorly occurs that overpowers the stabilizers resulting in dislocation (1,6). In contrast, posterior shoulder dislocations often occur secondary to forceful internal rotation and adduction (shock injuries or seizures) or due to a force applied anteriorly to the shoulder (1,6). Finally, inferior dislocations often occur secondary to high-energy injuries when a hyperabduction force levers the proximal humerus onto the acromion causing the humeral head to disengage inferiorly from the glenoid. As such, the humeral head becomes lodged in the infraglenoid space and these dislocations are commonly associated with soft tissue injury to the labrum and inferior joint capsule (1,6).
The axillary nerve traverses the axilla adjacent to the inferior capsule then wraps around the surgical neck of the humerus making it the most commonly injured nerve in shoulder dislocations (1,6). The axillary nerve provides motor innervation to the deltoid, teres minor, and long head of the triceps muscle units and sensory innervation to a patch of the anterolateral shoulder.
HISTORY AND PHYSICAL EXAMINATION
Original footage from our orthopedic surgeon Dr Simpson with UCMC medical students showcased as “patients”.
History should involve asking about mechanism of injury as well history of prior arm trauma, injuries, and dislocations as prior dislocation significantly increases risk of subsequent dislocations (2,5). Common mechanisms for anterior shoulder dislocations include force applied to abducted and externally rotated or extended arm in addition to falls onto an outstretched hand. Suspicion for posterior shoulder dislocation should be raised when patients sustain forceful internal rotation and adduction or a force applied to the anterior shoulder. Posterior shoulder dislocations commonly occur secondary to seizures or electrocution so make sure to inquire about relevant patient history.
If major trauma is present, examination and assessment of the patient should begin with a primary and secondary survey assessing for any life threats or other injuries. Physical examination of the shoulder itself includes inspection and palpation of the affected extremity with comparison to the contralateral extremity. Typically, passive and active movement of the affected extremity will be limited. Asking the patient to attempt to touch their contralateral shoulder can clue you into a dislocation as patients with a dislocation will typically be unable to do so. Patients with anterior shoulder dislocations will typically present with their arm internally rotated and abducted. Additionally, flattening of the shoulder silhouette compared to the contralateral shoulder is often apparent on inspection. In contrast, patients with posterior shoulder dislocations will often be holding their arm fixed internally rotated and and adducted. Finally, patients with inferior dislocations will typically hold the affected arm fixed in an abducted position over their head.
A thorough neurovascular exam should be documented both pre- and post-reduction. The axillary nerve is susceptible to traction injury due to its anatomic location with respect to the shoulder joint and has been reported to be injured in 13% of patients with shoulder dislocations (12). As such, sensory function of the axillary nerve should be assessed by testing for numbness over the anterolateral shoulder and motor function by assessing deltoid strength (involved in shoulder abduction). However, it can be difficult to assess deltoid weakness in the setting of trauma due to pain limiting range of motion. Of note, normal sensation in the axillary nerve distribution does not exclude axillary nerve injury (1). Additionally, examination should also involve assessment of the radial, median, and ulnar nerve distributions as well as the perfusion of the distal extremity.
imaging
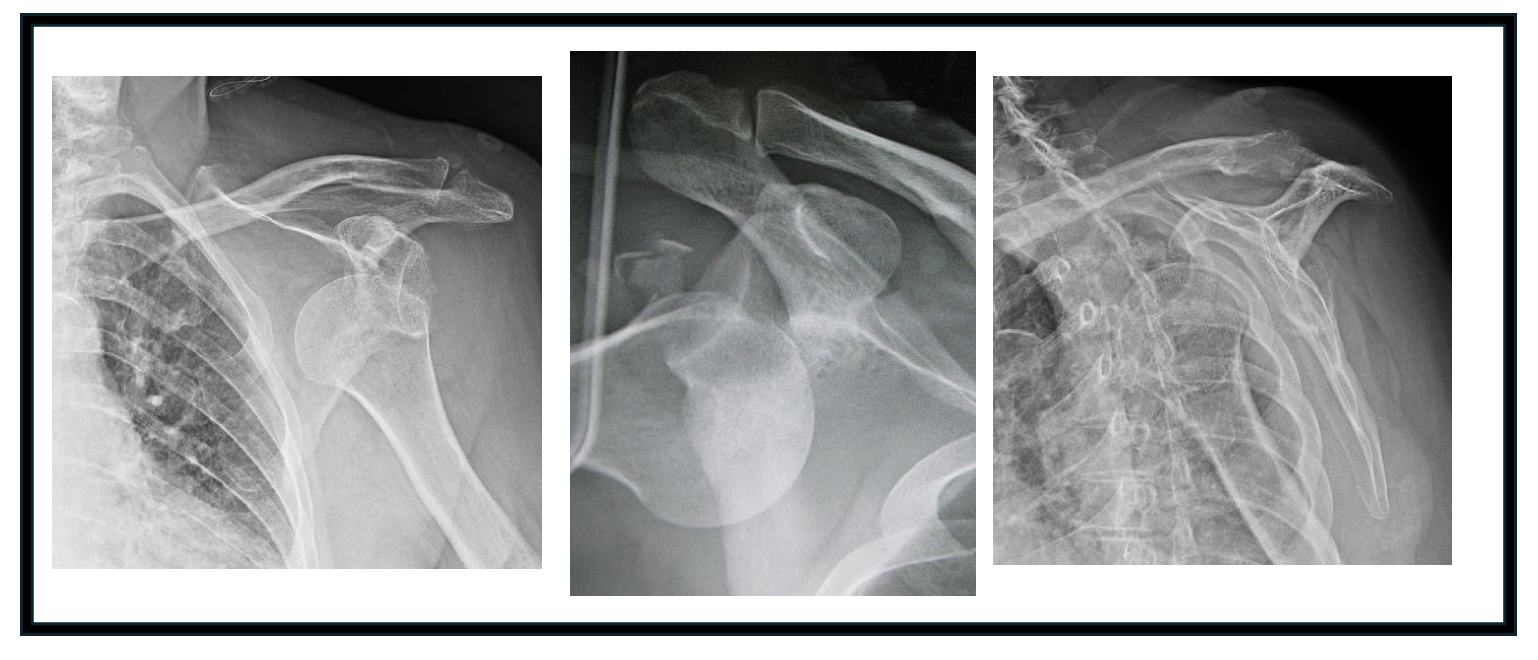
1) X-ray imaging
Plain radiograph imaging is the most common imaging modality used for evaluation of the dislocated shoulder. While there may be clinical signs of dislocation, radiographic imaging is pertinent to obtain at the time of injury and following reduction to ensure appropriate alignment and to evaluate for any fractures. The standard radiographic views should include AP, lateral, axillary and occasionally scapular-Y views. The axillary x-ray is performed with the patient’s arm abducted to about 90 degrees and the x-ray beam is directed into the patient’s axilla. A Velpeau view can be performed if the patient cannot tolerate position arm in space for the axillary view. The obtained image should show the relationship between the glenoid and the humeral head, which can help in the reduction maneuvers. A scapular-Y view is a lateral scapula view with the acromion, coracoid and scapula body forming a “Y” shape. The humeral head (in the non-dislocated setting) should be in the center of the “Y” but may be anterior or posterior to the “Y” when the glenohumeral joint is dislocated. While this view is particularly helpful in differentiating between anterior and posterior shoulder dislocations, it can be difficult to obtain especially when patients are in pain (1-3,25).
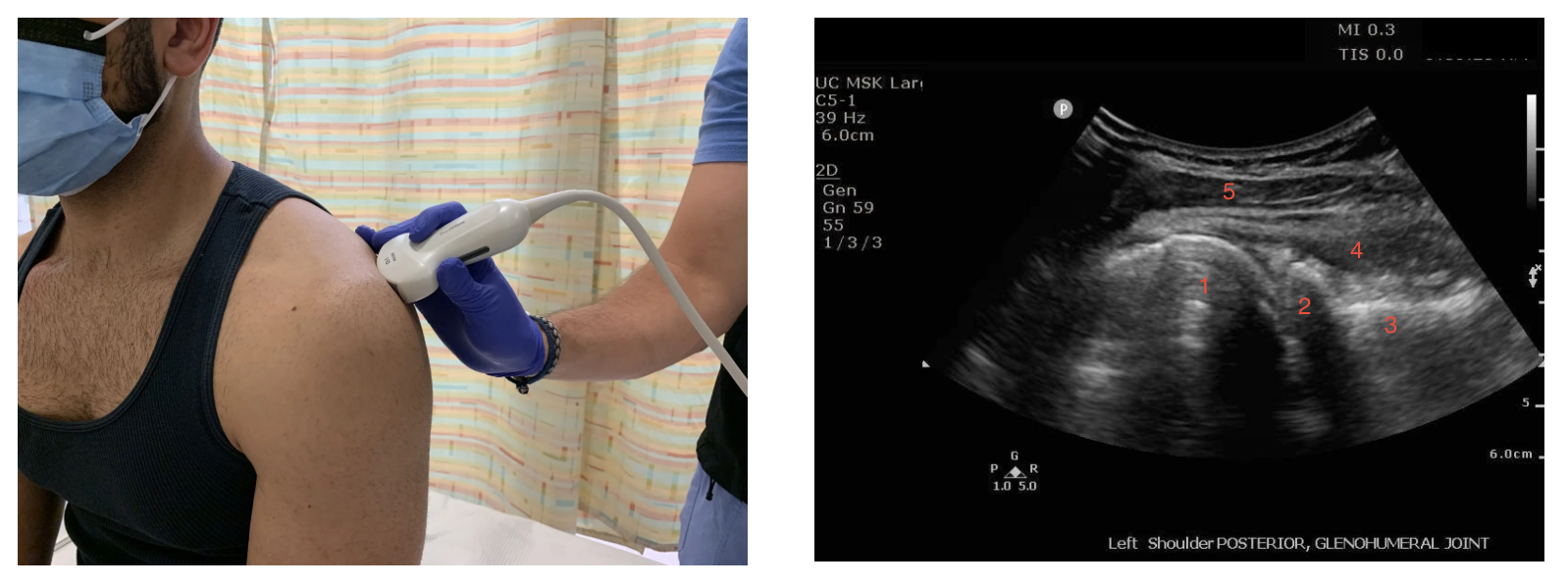
2) Ultrasound
While X-ray imaging will remain the primary imaging modality used for the diagnosis of shoulder dislocations, point-of-care ultrasound has been demonstrated to have essentially 100% sensitivity and specificity for the diagnosis of a shoulder dislocation when utilized and interpreted correctly (13,14). Furthermore, ultrasound can provide guidance for intra-articular anesthesia while also providing real-time feedback on success of reduction attempts without requiring repeat radiographs, though post-reduction radiograph should still be obtained as it is the current gold standard (14).
To acquire your image, stand behind the patient’s affected shoulder with arm adducted against their side and find the scapular spine then palpate laterally until you reach the glenohumeral space. Place a curvilinear or linear probe in transverse position parallel and slightly inferior to the scapular spine then slide lateral until you can visualize the glenoid and the humeral head (14). Probe marker should be oriented to the patient’s left. The location of the humeral head (circular structure immediately lateral to the glenoid) with respect to the glenoid can diagnose anterior versus posterior dislocations as the humeral head will be at a greater depth (farther from the probe) in anterior dislocations as opposed to more superficial (closer to the probe) in posterior dislocations (14,15). Following reduction, the humeral head should be in close approximation to the glenoid fossa and should be visualized to freely internally and externally rotate within the glenoid fossa (14,15). Normal shoulder anatomy is shown in images below. We recommend taking a look at this external site for a comprehensive video of normal anatomy vs anatomy seen under ultrasound guidance with shoulder dislocations.
3) Computed Tomography (CT)
Given that most of these patients present in the emergency department, a CT scan without contrast of the affected shoulder can easily be obtained following reduction and is often a crucial part of the treatment algorithm for the patient. While plain radiographs can confirm the reduction, CT scans help identify humeral and/or glenoid bone loss, which can be helpful in determining surgical management. Although surgery may not be the initial management for all patients with shoulder dislocations, identifying bone loss can help guide this decision. Studies have shown bone loss is one of the leading modifiable risk factors for recurrent dislocations, making its identification in both first-time or recurrent dislocations beneficial. Furthermore, some patients may have had previous subluxation events, leading to unrecognized bone loss that may not be visible on plain radiographs. From an efficiency standpoint in the emergency department, not every dislocation patient needs a CT. Instead, consider consulting orthopedic surgery before ordering a CT to determine if a specific patient might benefit from this additional imaging modality (26).
4) MRI
MRI is typically used in the setting of dislocation after a reduction to visualize any damage to the local soft tissues such as to the glenoid/humeral head, additional ligament injury in the shoulder, and any tears of the rotator cuff musculature. This imaging modality is typically not indicated in the emergent management of a shoulder dislocation (1-3,25).
Stay tuned for part 2 of this series will discuss intra-articular pain injection management, and various reduction techniques with videos.
POST BY charlie brower, MD AND Nana simpson, MD with assistance from medical students Bri Mcmonagle, luke buck, hayden schott
Dr. Brower completed his residency in Emergency Medicine at the University of Cincinnati in June 2025 and is now an attending EM physician at North Memorial Health in Minnesota.
Dr. Simpson completed his residency in Orthopedic Surgery at the University of Cincinnati in June 2025 and is now completing a fellowship specializing in Shoulder and Elbow surgery at the University of Pittsburgh.
EDITING BY brian grawe, md and bret betz, md and danny gawron, md and ANITA GOEL, MD
Dr Grawe is a Professor in Orthopedic Surgery at the University of Cincinnati with fellowship training in sports medicine and shoulder reconstruction. He is also one of the team physicians for the Cincinnati Bengals.
Dr Betz is an Associate Professor in Emergency Medicine at the University of Cincinnati with fellowship training in sports medicine. He works in both the emergency department as well as the sports medicine clinic. He is also one of the team physicians for the Cincinnati Bengals.
Dr Gawron is an Assistant Professor in Emergency Medicine at the University of Cincinnati with fellowship training in sports medicine. He works in both the emergency department as well as the sports medicine clinic.
Dr. Goel is an Associate Professor at the University of Cincinnati, a graduate of the UC EM Class of 2018, and an assistant editor of Taming the SRU.
References
Youm T, Taekmoto R, Park PKH. Acute management of shoulder dislocations. J Am Acad Ortho Surg. 2014; 22(12):761-771. doi:10.5435/JAAOS-22-12-761.
Gottlieb M. Shoulder Dislocations in the Emergency Department: A comprehensive Review of Reduction Techniques. J Emerg Med. 2020; 58(4):647-666. dot:10.1016 /j.jemermed.2019.11.031.
Zacchilli MA, Owens BD. Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg Am. 2010;92(3):542-549. doi:10.2106/JBJS.I.00450.
Leroux T, Wasserstein D, Veillette C, et al. Epidemiology of primary anterior shoulder dislocation requiring closed reduction in Ontario, Canada. Am J Sports Med. 2014;42(2):442-450. doi:10.1177/0363546513510391.
Kao JT, Chang CL, Su WR, Chang WL, Tai TW. Incidence of recurrence after shoulder dislocation: a nationwide database study. J Shoulder Elbow Surg. 2018;27(8):1519-1525. doi:10.1016/j.jse.2018.02.047.
Long B. EM@3AM: Anterior Shoulder Dislocation. emDOCs. April 4, 2020. Accessed November 16, 2024. https://www.emdocs.net/em3am-anterior-shoulder-dislocation/.
Hindle P, Davidson EK, Biant LC, Court-Brown CM. Appendicular joint dislocations. Injury. 2013;44(8):1022-1027. doi:10.1016/j.injury.2013.01.043.
Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am. 1956;38-A(5):957-977.
Robinson CM, Aderinto J. Posterior shoulder dislocations and fracture-dislocations. J Bone Joint Surg Am. 2005;87(3):639-650. doi:10.2106/JBJS.D.02371.
Patel DN, Zuckerman JD, Egol KA. Luxatio erecta: case series with review of diagnostic and management principles. Am J Orthop Belle Mead NJ. 2011;40(11):566-570.
Soslowsky LJ, Flatow EL, Bigliani LU, Mow VC. Articular geometry of the glenohumeral joint. Clin Orthop. 1992;(285):181-190.
Robinson CM, Shur N, Sharpe T, Ray A, Murray IR. Injuries associated with traumatic anterior glenohumeral dislocations. J Bone Joint Surg Am. 2012;94(1):18-26. doi:10.2106/JBJS.J.01795.
Gottlieb M, Russell F. Diagnostic Accuracy of Ultrasound for Identifying Shoulder Dislocations and Reductions: A Systematic Review of the Literature. West J Emerg Med. 2017;18(5):937. doi:10.5811/westjem.2017.5.34432.
Tin J, Simmons, Cailey, Ditkowsky, Jared, Alerhand, Stephen. US Probe: Ultrasound for Shoulder Dislocation and Reduction. emDOCs.net - Emergency Medicine Education. January 18, 2018. Accessed November 16, 2024. https://www.emdocs.net/us-probe-ultrasound-for-shoulder-dislocation-and-reduction/.
Blakeley CJ, Spencer O, Newman-Saunders T, Hashemi K. A novel use of portable ultrasound in the management of shoulder dislocation. Emerg Med J EMJ. 2009;26(9):662-663. doi:10.1136/emj.2008.069666.
Rauker N, Pensa G. Shoulder Dislocations. EM:RAP UC Max. August 2024. Accessed June 19, 2025. https://www.emrap.org/urgent-care/episode/ucmax2024august/shoulderreducti.
Aronson, Paul L, Mistry, Rakesh D. Intra-articular lidocaine for reduction of shoulder dislocation. Pediatr Emerg Care. 2014;30(5). doi:10.1097/PEC.0000000000000131.
EM:RAP Productions. Intra-articular Lidocaine For Reduction Of Shoulder Dislocation. Accessed May 5, 2025. https://www.emrap.org/episode/ema-2015-1/abstract22.
Rungsinaporn V, Innarkgool S, Kongmalai P. Is Ultrasound-guided or Landmark-guided Intra-articular Lidocaine Injection More Effective for Pain Control in Anterior Shoulder Dislocation Reduction? A Randomized Controlled Trial. Clin Orthop. 2024;482(7):1201-1207. doi:10.1097/CORR.0000000000002936.
Hayashi M, Tanizaki S, Nishida N, et al. Success rate of anterior shoulder dislocation reduction by emergency physicians: a retrospective cohort study. Acute Med Surg. 2022;9(1):e751. doi:10.1002/ams2.751.
Stafylakis D, Abrassart S, Hoffmeyer P. Reducing a Shoulder Dislocation Without Sweating. The Davos Technique and its Results. Evaluation of a Nontraumatic, Safe, and Simple Technique for Reducing Anterior Shoulder Dislocations. J Emerg Med. 2016;50(4):656-659. doi:10.1016/j.jemermed.2016.01.020.
Lin M. Trick of the Trade: Got a shoulder dislocation? Park it. ALiEM. June 25, 2013. Accessed June 19, 2025. https://www.aliem.com/trick-of-the-trade-got-a-shoulder-dislocation-park-it/.
Long N. Spaso technique. Life in the Fast Lane (LITFL). March 13, 2019. Accessed June 19, 2025. https://litfl.com/spaso-technique/.
Tobola, A., Cook, C. et al. Accuracy of glenohumeral joint injections: comparing approach and experience of provider. Journal of Shoulder & Elbow Surgery, 20(7): 1147-1154.
Bao MH, DeAngelis JP, Wu JS. Imaging of traumatic shoulder injuries - Understanding the surgeon's perspective. Eur J Radiol Open. 2022 Mar 2;9:100411. doi: 10.1016/j.ejro.2022.100411. PMID: 35265737; PMCID: PMC8899241.
Dickens, J., Slaven, S., Cameron, K. et. al. (2019). Prospective Evaluation of Glenoid Bone Loss After First-time and Recurrent Anterior Glenohumeral Instability Events. American Journal of Sports Medicine, 47(5): 1082-1089. doi: 10.1177/0363546519831286.