Therapeutics: Pacing Through Skin and Vein
/Cardiac Pacing, both transcutaneous and transvenous, is a critical skill of the EM physician but also can be a black box of when to trigger action and escalation, we will cover both below…
When to Pace:
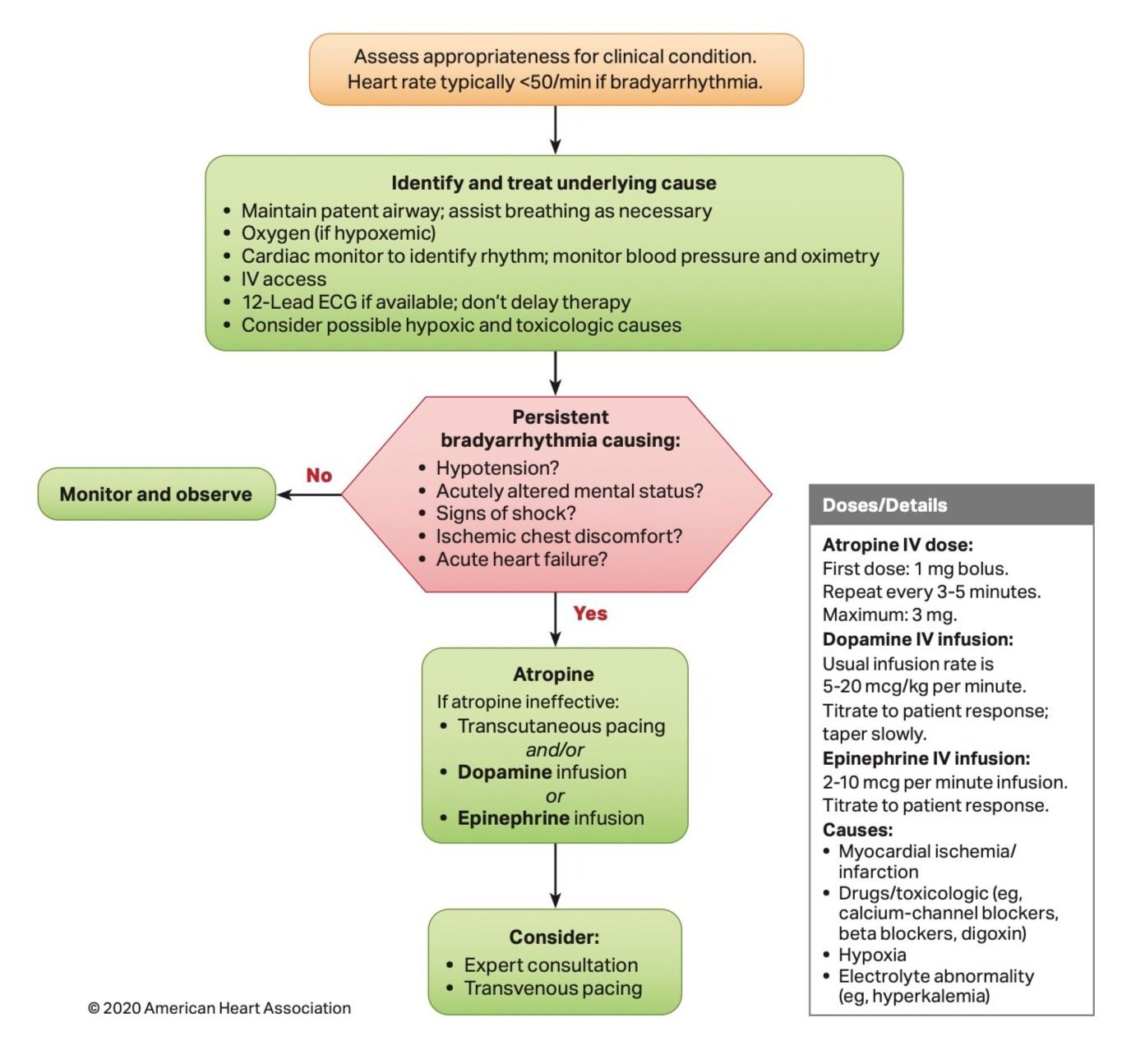
Bradycardia
Bradycardia can often be seen in patients following acute myocardial infarction (MI), most commonly in inferior or anterior MIs. In these patients, with a heart rate less than 50 beats per minute, initiate advanced cardiac life support (ACLS) bradycardia algorithm.
Follow this algorithm in patients with unstable bradycardia with acute heart failure, change in mental status, or concern for shock, physicians should start with atropine, 1 mg and may be continued every 3 to 5 minutes if effective.
Conduction Abnormalities
AV blocks, which can also be seen in patients with MI, may require pacing as well, due to ischemia affecting the electrical pathways of the heart.
Toxicogenic
In patients with possible medication overdoses, such as a beta blocker overdose, calcium channel blocker overdose, or digoxin toxicity, cardiac pacing may need to be temporarily initiated to maintain an adequate heart rate while initiating treatment or antidotes.
In patients with electrolyte abnormalities who are unstable, it may be beneficial to initiate pacing while starting treatment.
Transcutaneous Pacing:
Pad Placement
Historically, it was taught to place pads at the anterolateral (AL) position with the positive electrode pad over the right upper anterior chest wall and the negative electrode over the left midaxillary line. This was generally the easiest placement as it did not involve rolling the unstable patient; however, new data has shown that anteroposterior (AP) placement may be more effective. AP placement is when the positive electrode is placed under the left scapula and the negative electrode pad is placed over the left parasternal chest wall.
AP placement was proven to be capture at a lower current than the AL placement in the same patients, thus more effective. [5]
Set Up
Attach pads to patient (in AP orientation if possible)
Plug in pads to Zoll
Set Zoll to “pacer”
Start with rate set to 70 bpm (60-80)
Increase current to 40 mA then slowly increase current by 5-10 mA until you see electrical capture on the monitor
Verify you also have mechanical capture by checking palpable pulses to ensure they match the rate you set – continue to increase current until you also have mechanical capture
Adjust final setting to 5-10 mA above the lowest current where both electrical and mechanical capture are achieved for reliable pacing
Sedation/Analgesia
The electrical current used for inducing cardiac myocardial cell depolarization, can also cause chest wall muscle contractions which can be painful to patients. Skin burns and irritation can also result from the pacing pads and cause pain.
Sedation can be adequately achieved with benzodiazepines.
Opioid pain medications are most effective for analgesia while pacing.
Transvenous Pacing:
Indications
If a patient has been stabilized with transcutaneous pacing and is then alert enough to have difficulty tolerating the transcutaneous pacing.
You are unable to achieve mechanical capture with transcutaneous pacing.
Long-term temporary pacing may be required before patient is stable enough to have a permanent pacemaker implanted.
Set Up - please refer to the Taming the SRU page on Transvenous Pacemaker Placement for more in-depth details regarding placement.
Insert large bore Cordis or multi-lumen access catheter (MAC) to right internal jugular or left subclavian
Non-sterile person sets up pacer with electrical cords and ports plugged in (labels on electrical cord from wire will be marked “positive” to know which port it plugs into
Ensure balloon inflates and unlock syringe with balloon deflated
Sterile person threads Swan catheter/transvenous pacer wire to 15 cm
Inflate balloon and lock syringe
Turn on pacer and advance slowly until you have capture – you can set the transvenous pacer at different rate (higher) from transcutaneous to distinguish when you truly have capture from the TV pacer, or turn down transcutaneous pacer current
Deflate the balloon and tape catheter – noting depth of catheter where you achieved adequate capture electrically and mechanically
*Note: you can use transthoracic or transesophageal echocardiography to evaluate for adequate mechanical capture observing left ventricular rate in both transcutaneous and transvenous pacing.
Post by Madeleine Sookdeo, MD
Dr. Sookdeo is a PGY-1 in Emergency Medicine at the University of Cincinnati
Editing by martina Diaz-Mcdermott, MD and Ryan LaFollette, MD
Dr. Diaz-McDermott is a graduating PGY-4 and incoming Ultrasound Fellow at the University of Cincinnati
Dr. LaFollette is an Associate Professor in Emergency Medicine at the University of Cincinnati and co-editor of TamingtheSRU.com
References
Adult Bradycardia Algorithm, 2020, cpr.heart.org/-/media/cpr-files/cpr-guidelines-files/algorithms/algorithmacls_bradycardia_200612.pdf.
Bektas, Firat, and Secgin Soyuncu. “The efficacy of transcutaneous cardiac pacing in ED.” The American Journal of Emergency Medicine, vol. 34, no. 11, Nov. 2016, pp. 2090–2093, https://doi.org/10.1016/j.ajem.2016.07.022.
Moayedi, Siamak, et al. “Anteroposterior pacer pad position is more likely to capture than anterolateral for transcutaneous cardiac pacing.” Circulation, vol. 146, no. 14, 4 Oct. 2022, pp. 1103–1104, https://doi.org/10.1161/circulationaha.122.060735.
Cousar J, Bohanske M, Hill J. Transvenous Cardiac Pacemaker Educational Resource. MedEdPORTAL Publications; 2015. Available from: https://www.mededportal.org/publication/0107.
Siamak Moayedi, Priya Patel, Nicholas Brady, Michael Witting, Timm-Michael L. Dickfeld. “Anteroposterior pacer pad position is better than anterolateral for transcutaneous cardiac pacing.” Resuscitation, Volume 181,2022,Pages 140-146,ISSN 0300-9572, https://doi.org/10.1016/j.resuscitation.2022.11.009.
Scott Weingart, MD FCCM. EMCrit 310 – Transvenous Pacemakers. EMCrit Blog. Published on November 4, 2021. Accessed on June 18th 2024. Available at [https://emcrit.org/emcrit/transvenous-pacemakers/].