X-ray Vision - Shoulders and Elbows
/Radiography of the Shoulder
According to the American Academy of Orthopedic Surgeons, shoulder pain accounted for approximately 11.5 million visits to the physician in 2010. Additionally, shoulder dislocations are the most common dislocation seen in the emergency department (1). Radiographs along with a thorough history of physical exam plays a key role in the diagnosis of the cause of shoulder pain.
Indications
According to the American College of Radiology, plain films are the preferred first testing in the setting of traumatic and atraumatic shoulder pain. In the setting of traumatic cases 3 views should be obtained, these include an anterior-posterior view in both internal and external rotation as well as Lateral Y or Axillary view (2). In atraumatic shoulder pain, 2 views – most frequently an anterior-posterior view along with a scapular Y or axillary view – are considered sufficient (3).
Anatomy
In order to identify pathology on shoulder plain films, an understanding of normal anatomy is essential. There are three main components of the shoulder radiography: the bones, the joints and soft tissue. The bones of the shoulder include the proximal humerus, the lateral clavicle, the ribs, and the scapula. The scapula is, in turn, subdivided into the glenoid, the coracoid, and the acromion. The articulation of these bones comprises the 4 major joints, specifically the glenohumeral, acromioclavicular, sternoclavicular, and scapulothoracic joint. Though plain films offer limited resolution into the integrity of soft tissue structures, clinicians should review the associated musculature and nonosseous structures for gross abnormalities (4).
Shoulder Views
Shoulder imaging should, at the minimal, consists of both an anteroposterior and a lateral view. A standard approach behooves clinicians in reviewing radiography: first by confirming the you are looking at the correct patient, the correct laterality (right or left), and desired view before proceeding to review the alignment, bone densities, osseous cortex, and the soft tissue structures.
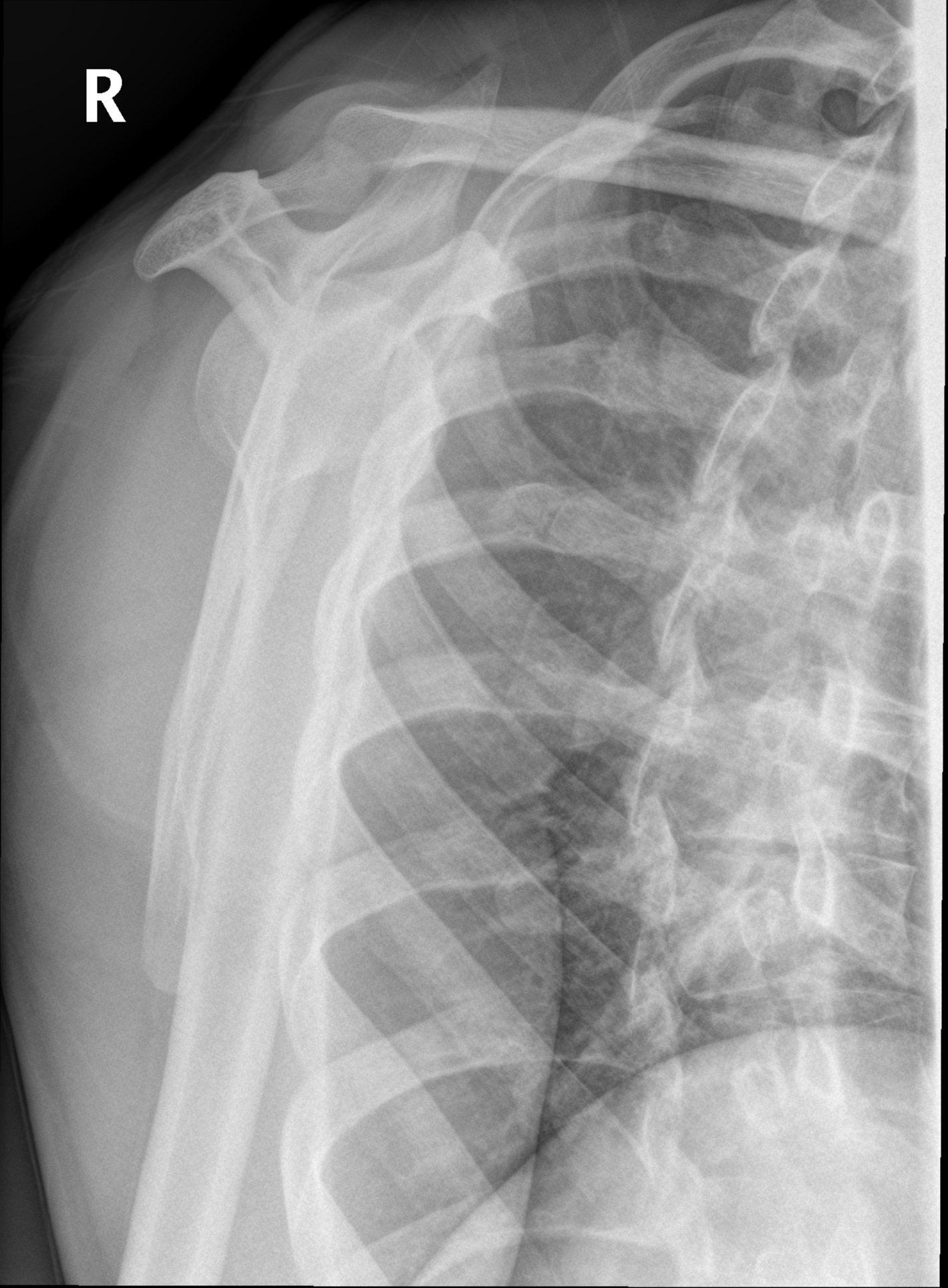
In the anterior-posterior (or anteroposterior) view, you should start by evaluating the glenohumeral joint, the acromioclavicular joint, and the scapulothoracic joint. The sternoclavicular joint is typically not visible. Next, evaluate the bony structures for gross deformities, luxations, fractures, or cortical irregularities. Finally, review at the soft tissue for any evidence of calcification or soft tissue swelling. Additionally, if the image was obtained with the arm in either internal rotation or external rotation, you can look at the lesser or greater tubercle, respectively, for fracture (Figure 1) (4,5,6,7).
Figure 1 -
Figure 2 - Case courtesy of Dr Craig Hacking, https://radiopaedia.org/. From the case https://radiopaedia.org/cases/37498
The lateral view can be extremely helpful in evaluating for both dislocation and fracture. Providers should start by looking at the glenohumeral joint and its relationship to the body of the scapula, acromion, and coracoid process. The humeral head should be centered over the glenoid fossa and make a Y shape (Figure 2). You can also evaluate the bony structures (coracoid process, scapula, acromion, and proximal humeral shaft) for fractures as well as the soft tissues (4,7).
The axillary view is also an extremely valuable view if you are concerned for dislocation, as this view details the position of the humeral head relative to the glenoid fossa (Figure 3). As the head of the humerus and neck of the humerus and scapula are visualized well on this view, the axillary radiograph is the study of choice to assess for a Bankart fracture, which involves fracture the anterior glenoid rim. A limitation of this view is that the patient must be able to abduct the arm and patient may be unable due to pain. Alternatives views to the axillary view include the Velpeau, modified Velpeau, and West Point views (4).
Figure 3 - Case courtesy of Dr Matt Skalski, https://radiopaedia.org/ From the case https://radiopaedia.org/cases/23096
Common pathologies
As mentioned, shoulder dislocations are the most common dislocations seen in the emergency department. Should dislocations are named according to the displacement of the humeral head relative to the glenoid fossa: anterior, posterior, or inferior. Of the three, anterior dislocations account for 95% of all shoulder dislocations, with posterior being 2nd most common and inferior displacements being the least common. Given their frequency, it is important to note some of the associated radiographic pathology that can be seen with anterior dislocations, namely the Hill–Sachs defect and Bankart fracture (Figure 4) (8).
Fractures of the proximal humerus are also not infrequently seen, including surgical neck, anatomical neck (figure 5), and fractures of the greater and lesser tuberosity. Other common pathologies of the shoulder include scapular, clavicular and rib fractures, and acromioclavicular joint dislocations (4).
Figure 4 - from https://radiopaedia.org/articles/shoulder-dislocation?lang=us
Limitations
Plain films are a good first test for any type of shoulder pain. However, despite being able to detect most fractures and dislocations, additional testing may be needed to diagnose radiographically occult injuries. Conditions such a rotator cuff tears, nerve impingements, and degenerative changes are not well-delineated on X-ray and could require further imaging such as ultrasound, CT, or MRI (4).
Radiography of the Elbow
Trauma to the elbow and proximal forearm represent around 15% of upper extremity injuries annually (9). Elbow dislocations are the second most common dislocation seen in the emergency department (following shoulder dislocations) in adult populations and the most common dislocation seen in pediatric demographics.
Indications
As with shoulder plain injuries, the American college of Radiology recommends plain films as the initial imaging test in the setting of acute, chronic, and traumatic elbow pain (10).
Anatomy
The elbow consists of 3 bones and 3 joints. The bones include the humerus, ulna, and radius. The elbow comprises three joints including the radiohumeral joint (the articulation of the capitulum and the radial head), the proximal radioulnar joint (the articulation of the radial notch of the ulna and head of the radius), and the ulnohumeral joint (the articulation of the trochlear notch of the ulna and trochlea of the humerus). Additional boney structures to consider when assessing radiographs of the elbow include the medial and lateral epicondyles of the humerus and the ulnar coranoid process and olecranon (11).
Views
Standard radiographic evaluation of the elbow includes 2 views: an anteroposterior view and a lateral view. As described above, providers should adopt a systematic approach to evaluating elbow plain films that includes confirming the correct patient, laterality, and the views that have been obtained. Providers may assess for proper alignment of the joint by drawing an imaginary “radiocapitellar line” (which is maintained in both AP and lateral views) as well as an “anterior humeral line” (demonstrated in the lateral view). In pediatric imaging, providers may also note the presence and alignment of metaphyseal structures, depending on the patient’s age; clinicians must be diligent not to mistake centers of ongoing osseous growth for fractures (12). A unique feature of elbow X-rays relates to the presence of both anterior and posterior fat pads lining the joint space; displacement or accentuation of these fat pads is highly suggestive of underlying injury to the osseous or joint structures
In the AP view, the image is taken with the elbow in full extension and the arm supinated (the hand facing up), allowing for examination of the medial and lateral epicondyles, the radiohumeral joint, and the radiocapitellar line. Any deviation in the radiocapitellar line could indicate a possible dislocation of the radial head (Figure 6) (11,12,13).
The lateral view is obtained with the elbow in flexion, forming a 90-degree angle, and the forearm in a neutral position (with the thump facing up). The ulnohumeral joint, coranoid process, and olecranon are all apparent on this view. Soft tissue structures are optimally defined in this view, to include the anterior and posterior fat pads and supinator fat plane. As described above, providers should utilize the lateral view to assess the anterior humeral line, which should pass through the middle third of the capitulum. Anterior or posterior displacement of capitulum can suggest a physeal/growth plate injury or supracondylar fracture of the humerus. The radiocapitellar line is drawn through the middle of the radius and should pass through the capitulum on all radiographic views (Figure 7) (11,12).
Figure 6 - From http://pemplaybook.org/podcast/pediatric-elbow-injuries/
Figure 7 - From https://radiologypics.files.wordpress.com/2013/03/elbow-1.jpg
Bizarrely, both “capitulum” and “capitellum” are used to described the articulating body of the humerus that interfaces with the radius. Both words stem from Latin meaning “little head” and are used essentially interchangeably with regards to human anatomy.
Common Pathology
Radial head and neck fractures are the most common elbow fractures encountered in adults and can be classified by the Mason-Johnston system (14). These fractures can be very subtle and are sometimes missed; on occasion, a displaced anterior fat pad may be the only radiographic sign of a radial head/neck fracture. Additionally, distal humerus fractures and coranoid process fractures are not uncommonly seen. Some uncommon fracture/dislocations that of the elbow that include forearm and wrist pathology are the Monteggia, Essex-Lopresti, and Galeazzi fractures/dislocations. Though infrequent, these injuries can require emergent orthopedic intervention and cannot be missed (14,15)
Limitations
Overall, plain radiography is a good tool for detecting fractures and dislocations. In adults, overuse injuries - such as biceps tendonitis, olecranon bursitis, and medial and lateral epicondylitis - account for a significant portion of subacute elbow pain. While radiography is still the appropriate imaging modality, these conditions are typically diagnosed clinically and further imaging may be required, such as MRI (16).
References
Department of Research & Scientific Affairs, American Academy of Orthopaedic Surgeons. Physician Visits for Musculoskeletal Symptoms and Complaints. Available at: http://www.aaos.org/research/stats/patientstats.asp.
Amini B, Beckmann NM, Beaman FD, et al. ACR Appropriateness Criteria ® Shoulder Pain–Traumatic. Journal of the American College of Radiology. 2018;15(5). doi:10.1016/j.jacr.2018.03.013.
Small KM, Adler RS, Shah SH, et al. ACR Appropriateness Criteria® Shoulder Pain-Atraumatic. Journal of the American College of Radiology. 2018;15(11). doi:10.1016/j.jacr.2018.09.032.
Sanders TG, Jersey SL. Conventional Radiography of the Shoulder. Seminars in Roentgenology. 2005;40(3):207-222. doi:10.1053/j.ro.2005.01.012.
Murphy A. Shoulder series: Radiology Reference Article. Radiopaedia Blog RSS. https://radiopaedia.org/articles/shoulder-series?lang=us. Accessed October 9, 2019.
Murphy A. Shoulder (AP view): Radiology Reference Article. Radiopaedia Blog RSS. https://radiopaedia.org/articles/shoulder-ap-view-1?lang=us. Accessed October 9, 2019.
Shoulder Radiography. In: Imaging of the Shoulder. Springer, Berlin, Heidelberg; :3-13.
Cutts S, Prempeh M, Drew S. Anterior Shoulder Dislocation. The Annals of The Royal College of Surgeons of England. 2009;91(1):2-7. doi:10.1308/003588409x359123.
Pitts SR, Niska RW, Xu J, Burt CW. National Hospital Ambulatory Medical Care Survey: 2006 emergency department summary. Natl Health Stat Report 2008;(7):1–38.
Chronic elbow pain. American College of Radiology. ACR Appropriateness Criteria. Radiology. June 2000:339-343.
Grayson DE. The Elbow: Radiographic Imaging Pearls and Pitfalls. Seminars in Roentgenology. 2005;40(3):223-247. doi:10.1053/j.ro.2005.01.013.
Shetty A. Elbow series: Radiology Reference Article. Radiopaedia Blog RSS. https://radiopaedia.org/articles/elbow-series?lang=us. Accessed October 9, 2019.
Shetty A. Elbow (AP view): Radiology Reference Article. Radiopaedia Blog RSS. https://radiopaedia.org/articles/elbow-ap-view-2?lang=us. Accessed October 9, 2019.
Sheehan SE, Dyer GS, Sodickson AD, Patel KI, Khurana B. Traumatic Elbow Injuries: What the Orthopedic Surgeon Wants to Know. RadioGraphics. 2013;33(3):869-888. doi:10.1148/rg.333125176.
Liman MNP, Avva U, Ashurst JV, et al. Elbow Trauma. [Updated 2019 Jun 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan. https://www.ncbi.nlm.nih.gov/books/NBK542228/
Kane SF, Lynch JH, Taylor JC. Evaluation of Elbow Pain in Adults. https://www.aafp.org/afp/2014/0415/p649.html. Published April 15, 2014. Accessed October 9, 2019.
Authorship
Written by Calyn Crawford, MD PGY-1, University of Cincinnati Department of Emergency Medicine
Peer Review by Matthew Scanlon, MD, PGY-4, University of Cincinnati Department of Emergency Medicine
Editing and Posting by Jeffery Hill, MD MEd