Hemoptysis
/What is it? Bleeding below the cords
More specifically, it may be subdivided into Massive and Non-Massive hemoptysis. And while the definitions of massive vary from paper to paper, it is generally agreed that increasing volume over 24 hours is associated with increased mortality. However, the literature consistently concludes that patients and providers are poor, at best, at estimating volume. Thus, the simplest and most effective definition for massive hemoptysis is as such: expectoration of blood causing hemodynamic instability or abnormal gas exchange / airway obstruction.
- Pearl: 90% of bleeds are from the Bronchial arteries which see systemic pressures as opposed to the lower pressure pulmonary arteries.
What causes hemoptysis?
- Out of all patients, the most common cause is bronchitis
- Looking specifically at massive hemoptysis, the big 3 are
- Bronchiectasis
- Infectious (cavitating lesions, pneumonia, TB)
- Mass
How do you manage these patients?
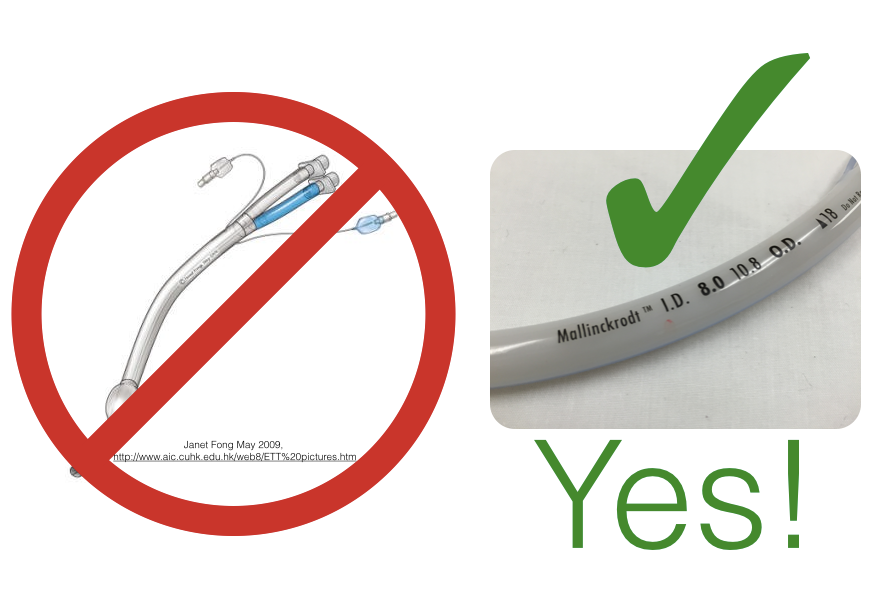
Keep in mind that as little as 200mL of liquid is required for asphyxiation. Once the decision to intubate is made, reach for the largest ETT available (expect this patient to get bronched).
- Pearl: Greater than 50% double lumen ETT are misplaced - even when thoracic anesthesiologists are placing them. And, you can’t bronch through them.
- Point: don’t use them
Post-intubation care is more complicated than the usual ABG and CXR. Reading the CXR as soon as humanly possible is important. You’ve got a 50/50 shot to identify the location of the lesion via CXR. Once the lesion is localized you can A) place the patient in the lateral decubitus position with the pathology side down to protect the good lung and B) consider mainstem intubation if there is concern that the patient’s good lung is being affected.
- Pearl: place the tube past the cords and rotate 90 degrees towards the mainstem bronchus you would like to intubate, advance until you meet resistance, and viola!
- 95% R mainstem and 73% left mainstem success rates (Bair et al, 2003)
Next steps:
- Pick up the phone: IR, CT surgery, and Interventional Pulm
- Resuscitate your patient
- Localize/define the lesion:
- CTPA if possible, but if too unstable, bedside bronchoscpy
References
- Bair AE, Doherty MJ, Harper R, Albertson TE. An evaluation of a blind rotational technique for selective mainstem intubation. Acad Emerg Med. 2004;11(10):1105-7.
- Haponik EF, Fein A, Chin R. Managing life-threatening hemoptysis: has anything really changed? Chest. 2000 Nov;118:1431-5.
- Hirshberg B, Biran I, Glazer M, Kramer MR. Hemoptysis: etiology, evaluation, and outcome in a tertiary referral hospital. Chest. 1997 Aug;112:440-4.
- Ibrahim WH. Massive haemoptysis: the definition should be revised. Eur Respir J. 2008 Oct;32:1131-2
- Klein U, Karsai W, Bloos F, et al: Role of fiberoptic bronchoscopy in conjunction with the use of double-lumen tubes for thoracic anesthesia: A prospective study.Anesthesiology 1998; 88:346-350
![Lung Cancer. By For the original image: unknown. For this edited version: Doruk Salancı. [Public domain], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1422883861684-UGWXH1S4KK4JOWR6SQJK/image-asset.png)