Grand Rounds Recap 1/7/14
/CPC with Dr. Boyer vs. Dr. Steuerwald
16 yo female with 4 days of bilateral lower quadrant abdominal pain and diarrhea that was tachy, dry, and with a diffusely tender abdomen and some right-sided discomfort on pelvic exam with a mild leukocytosis.
Dr. Steuerwald's approach to listening to patient presentations: Pick out the main symptoms, get a time course, and listen for any other true "weirdness" then build your own timeline of events.
- Don't forget about the "sexy numbers" in everyone, these include the vitals and also key aspects of a disease process (i.e. the EF in a patient with CHF)
- DDx included appendicitis, PID, TOA, Fitz-Hugh Curtis, Ovarian Torsion, Yersinia enterocolitis
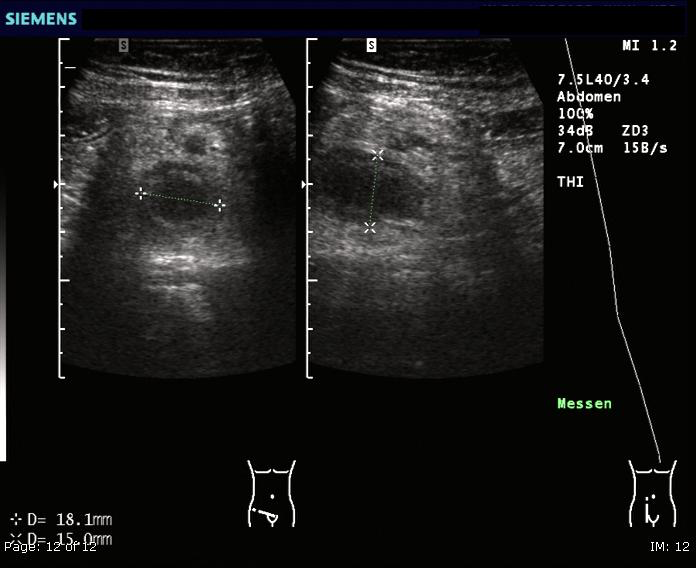
- Dr. Steuerwald correctly identified the need to get a RLQ US to assess for appendicitis!
Keep in mind that kids, elderly, and women often don't follow the text book
- The younger the child with appy, the more likely that the diagnosis will be delayed, in part because many of these patients present later, however in one study up to 2/3 of those with perforation had seen a health care provider and was given an alternative diagnosis since the onset of their symptoms
Perforation rate is highest within the first 1-2 days of onset of pain, so return precautions need to truly be strict and we may want to reduce the time course to 8-12 hours, rather than "within a few days"
The Pediatric Appendicitis Score (which includes RLQ tenderness, pain with hopping/percussion, nausea/vomiting, anorexia, fever, migration of pain, leukocytosis, and neutrophilia) was developed and validated with an initial sensitivity of 100% and specificity of 92%
- Further studies have revealed that the PAS (as with most scoring systems) depend on the prevalence of disease and thus low risk scores (especially in a referral populations) may have higher risk for missing disease
- Consider combining imaging modalities (such as RUQ US) for patients with mid-range scores to further reduce the "miss rate" of a scoring system such as the PAS
Systematic Reviews with Dr. Toth
A systematic review can often help to separate the wheat from the chaff in research as the medical literature is growing so fast that these help summarize many smaller studies into a more meaningful result
Advantages of a systematic review is that the can minimize bias, focus the summary of recommendation for a given research question, increase the power and generalizability
- To create a good systematic review the process must be explicitly outlined in advance and reproducible
- As with all research a review should have a good clinical question, but sometimes one must ask if the field is ready for it before undertaking the review
Meta-analysis is the statistical test that helps clarify the results of the review by aggregating the results of the individual studies reviewed
Keep in mind "GiGo" when assessing a review, that is "Garbage in, garbage out"
RUQ US with Dr. Thompson
RUQ US in the ED can approach the sensitivity of formal US when assessing for cholecystitis (91% vs. 94%)
Be sure to assess the gall bladder in longitudinal and transverse in both supine and left lateral decubitus positioning
The targeted clinical questions we ask each time are:
- Are there gallstones?
- Is the common bile duct (CBD) dilated?
- Is there a Sonographic Murphy's Sign?
- Is the gall bladder wall thickened?
- Is there pericholecystic fluid?
Be sure to measure the common bile duct and gall bladder wall every time, depth settings can affect your ability to reliably "eyeball it."
- Normal CBD is 5mm or less in anyone under 50, from that point on you get +1mm/decade
- Normal gall bladder thickness is less than or equal to 3mm and should always be measured using the anterior wall in a transverse plane
When assessing for a Sonographic Murphy's Sign, you must elicit pain in the patient while watching under ultrasound the compression of the fundus of the GB but there should not be pain when not over the GB, this can greatly add to the sensitivity of your exam
When having trouble locating the gall bladder consider moving to left lateral decubitus positioning or asking the patient to take and hold a deep inspiration, also consider asking when the last time the patient ate, as this exam is always best performed when NPO
Use Color Doppler to help identify the CBD as the portal vein and hepatic artery will run with it, giving you 3 tubular structures to differentiate between
R4 Capstone on Research Policy & Ethics with Dr. Walsh
Research can be quite contentious and its vital that we keep our fingers on the pulse of not just reviewing evidence but being mindful of what the popular press conveys to our patients
Recent scandals in the world of medical research have included questionable cell lines and lineage used throughout basic science studies, recognizing that animal models rarely adequately serve as a real model for humans, the lack of reproducability of many results of published studies and the publication bias of publishing positive trials.
There has been a precipitous decline in the number of large clinical trials finding statistically significant patient centered outcomes over the last several decades and it is unclear why
Obstetric Emergencies with Dr. Flood-Shaffer
Rupture of membranes (ROM) can happen spontaneously during normal labor or at times are artificially rupture by the healthcare team, however problems arise when these rupture prematurely
- Premature Rupture of Membranes (PROM) occurs when membranes rupture prior to the onset of labor when a pregnancy is at term (greater than or equal to 37 weeks) and requires admission
- Preterm Premature Rupture of Membranes (PPROM) occurs when PROM occurs when the pregnancy has not yet reached term
The typical precipitant for PROM or PPROM is a bacterial infection
A diagnosis of PROM (or PPROM) should be considered anytime a pregnant woman is complaining of leakage of fluid from her vagina and prompt a sterile speculum exam
If PROM/PPROM is on the DDx avoid a digital exam until you've ruled it out
Pregnant women presenting to the ED with vaginal bleeding who are over 20 weeks gestation should similarly not have a digital exam until placenta previa can be ruled out
Tests for PROM/PPROM include ferning (placing fluid on a slide to let dry and assess for a broad-leafed fern pattern under microscopy), however, this is only 51% sensitive and 75% specific
- There are newer testing kits available to test for placental alpha-microglobulin (PAMG-1), which is 99% sensitive
- Management of PROM is delivery, which is typically induced by OB
- Management of PPROM in later pre-term period (34-37 weeks) is typically delivery by OB
- Management of PPROM from viability (at ~24 weeks) to 34 weeks is typically expectant management with antibiotic therapy for presumed ascending infections (and also GBS prophylaxis), steroids for fetal lung maturity, and in attempt to prolong the pregnancy safely through reduced activity
- Strict bedrest is a thing of the past, while minimal activity is still encouraged the risks of strict full time bedrest can be equally detrimental
- Management of PPROM before 24 weeks is typically significant counseling as the pregnancy is likely non-viable
Many women experience contractions throughout their pregnancy and these should be classified as whether they are associated with cervical change
- The common term of "Braxton-Hicks Contractions" are now referred as false contractions and are quite common and may start out as regular, they typically quickly become irregular and extinguish in a change in activity
- Preterm contraction not associated with cervical changes can be treated with sedation (i.e. hydroxyzine) and hydration
Preterm labor is defined as regular contractions that are associated with cervical changes prior to 37 weeks gestation and accounts for 12.3% of births in the US
- Risks associated with preterm labor include prior preterm births, STI history, low SES, smoking, short cervix, short pregnancy interval (time between pregnancies), and African-American race
- Treatment for preterm labor should include hydration, magnesium sulfate (4-6g IV; for fetal neuroprotection), steroids (betamethasone 12.5mg IV; for fetal lung maturity), tocolysis (nifedipine PO is currently what is being recommended by our OB's), and antibiotics (for GBS prophylaxis)
- If you are concerned for preterm labor, send a fetal fibronectin, which must be completed during the sterile speculum exam as bimanual cervical checks can lead to false positives
Air Care Procedure Lab with Drs. Hinckley, Powell, Steuerwald, Chinn, & Latimer
Peri-morteum C-Section: Complete in pregnant women who are in cardiac arrest with obviously gravid uterus whose fundal height reaches the ubmilicus (~20 weeks gestation)
- Decision to complete the C-section should occur within 4 minutes of losing pulses for optimal fetal outcomes, keep in mind that this can significantly increase mom's rate of ROSC due to increased blood return
- Make an incision sub-xiphoid and extending to the pubic symphysis to expose the uterus, make a punch incision through the uterus with a scalpel and then use scissors to open the uterus and expose the fetus and deliver the fetus
- Be sure to continue resuscitative measures for mom, such as chest compressions, during the c-section
Lateral Canthotomy and Catholysis: Complete in patients with facial trauma who do not have signs of open globe but who have signs of increased intraocular pressure (i.e. vision loss or proptosis) (should be discussed with medical control)
- Anesthetize the lateral canthus of the eye with lidocaine with epi and then bluntly dissect the lateral canthus from the globe with a hemostat and place the hemostat on the lateral aspect tightly to help devascularize and then extend an incision from the lateral canthus to expose the canthal ligament, using scissors, pointing away from the globe, cut the canthal ligament to reduce intraocular pressures
- Often cutting just the inferior aspect of the canthal ligament will be adequate but if IOP continues to be high you can also cut the supeior canthal ligament
Field Amputation: Complete in patients with obvious life-threats that are entrapped due to a single crushed extremity (should be discussed with medical control)
- Provide appropriate sedation/analgesia and clean the area proximal to the entrapped extremity, use a scalpel to make a circumferential incision through the skin, soft tissue and muscles, loop the gigli saw around the affected extremity and use a back-and-forth motion superiorly to cut through the bone
![By James Heilman, MD (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1420896647203-WD9W4ZU5W0GPI9HELQEH/image-asset.png)




