Grand Rounds Recap 8/10
/Case Follow Up with Dr. Palmer
Female in her 40s with a history of sickle cell disease and hypertension presented via EMS for Altered Mental Status
She was involved in altercation with her family when she "passed out". glucose is 135.
VS: 168/104 P 101 RR 22 98% 98.6F
Exam:
General - Diaphoretic, moaning, agitated
Neuro - Pupils sluggish but symmetric, non-conjugate gaze, moves all extremities, occasionally shows thumb, intermittent jerking that is occasionally rhythmic
Remainder of exam unrevealing
DDx: seizures, stroke, ICH, PRES, atypical migraine, encephalitis/meningitis, CVT, metabolic or endocrine abnormality, tox
Patient was treated with several doses of versed with questionable/mild improvement, Noncontrast head CT was normal, as was laboratory/tox workup. cEEG revealed no seizure activity, but CTA revealed basilar artery occlusion.
Stroke in Sickle Cell Disease
By age 45, 25% of sickle cell patients will have stroke. There is a predilection for AIS in ages <20yo and >30. ICH predominates however in ages 20-29 years. The pathophysiology is thought to be the following:
- Sickled RBC stick to endothelium
- Pro-inflammatory state with endothelial proliferation
- Sickle cells trap other cells (platelets and WBC)
Additionally, hyperemia is thought to play a role. Because of the chronic anemia of sickle cell disease, over time vessels maximally dilate and can not facilitate any increase in flow to compensate for stress.
Basilar Artery Stroke
Strongly consider in AMS not otherwise explained. Particularly consider in AMS +gaze/ocular abnormality (non conjugate gaze, vertical nystagmus, rotary gaze, gaze palsy, INO).
Watch for bulbar symptoms: facial weakness, dysarthria, dysphonia, dysphagia. Less obvious symptoms include adventitious movements like jerking, fasciculations, shaking, twitching, which can be precipitated by painful stimuli.
Stroke Treatment in Sickle Cell Disease
For sickle cell patients, acute stroke treatment can include emergent exchange transfusion. The goal is to reduce Hgb S fraction to <30%, but not to increase Hgb >10 (which has been shown to viscosity and decrease O2 delivery). Patient require large bore access and a T&S, in addition to normal labs. tPA can be considered/discussed with your stroke colleagues, but it has not been studied in SCD, and it's postulated that there is a higher risk of ICH 2/2 silent infarcts in SCD brains.
R4 Case Follow Up with Dr. Scupp
4 year old male with a chief complaint of headache
Per family, has been acting strange, with staring spells that last about a minute going on for 1-2 days. Otherwise eating and drinking, no fevers, no recent illness. Patient complains of headache "all over" (he's 4).
VS: 101/60 P 120 RR 24 98% 98.6F
Exam:
General - pale, with noted bruising to anterior chest wall
Neuro: Slow to answer questions, otherwise non focal
Remainder of exam unremarkable.
Red Flags for Pediatric Headache:
- Age <6 yo
- Headaches upon waking
- Headaches worse with valsalva
- Chronic, progressive headaches; severe, acute headaches
Patients labs notable for a WBC of 4.2/Hgb 7.2/Hct 20.7/ Plts 18; 25% blasts on differential. Head CT with hyperdense signal over the midline sphenoid extending anteriorly from the pituitary.
DDx included: leukemia, langerhans cell histiocytosis, primary CNS lesion
The patient was diagnosed with CNS leukemia given his lab abnormalities and imaging. Leukemia has an incidence of 4.5/100,000 kids, 77% of which being ALL. Five percent of these leukemia patients will present with CNS symptoms. Our patient was admitted, started on induction chemotherapy with vincristine and donarubicin, and underwent LP both for diagnosis and therapeutic intrathecal chemo.
Would you give platelets to this patient with a platelet count of 18 needing an LP? The best evidence available recommends:
- Platelet count 10,000 - transfuse asymptomatic thrombocytopenia to this level (typically primary bone marrrow failure, leukemia, aplastic anemia patients)
- Platelet count 20,000 - transfuse patients undergoing minor invasive procedures (like central lines) to this level. Poor quality evidence.
- Platelet count 50,000 - transfuse patients undergoing major invasive procedures (like LP and non neurologic surgery) to this level. Very poor evidence here.
The PATCH trial recently published in Lancet 2016 investigated giving platelets to supratentorial ICH patients with GCS >8, known to be on anti platelet therapy for at least 7 days.
Results: the platelet group had increased risk of death as well as in hospital and 90 day mortality, as well as an increased in-hospital complication rate.
R2 Case Follow Up with Dr. Merriam
Male in his 50s with a chief complaint of chest pain
He was found outside a gas station smelling of EtOH. He is confused and can not answer basic questions besides stating that he has chest pain.
VS: 99/69 P 59 RR 1096% T: unreadable (feels cold, and our thermometer will read as low as 80 Farenheit)
Exam:
He is cold, confused.
Coarse breath sounds bilaterally
Neurologically he is non focal, but obviously disoriented.
Hypothermia is defined as a core temp <35C. It carries with it a 40% in-hospital mortality. For every 1 degree drop in C temperature, cellular O2 consumption decreases 6%, which can actually serve as a protective mechanism in significant hypothermia.
- Mild hypothermia = core temp 32-35 C; presents with some confusion
- Moderate hypothermia = core temp 28-32 C; presents with impaired judgement, paradoxical undressing
- Severe hypothermia = 25-28C; presents with dysarthria, ataxia, unconscious
- Profound hypothermia is <20C
Various organ systems react differently to hypothermia.
- Anterior hypothalamus mediates vasoconstriction to keep blood in the core. Posterior hypothalamus mediates shivering.
- Kidneys undergo cold diuresis, and ~50% of patients develop AKI from hypovolemia. HypoK is a poor prognostic sign.
- The blood increases in viscosity, and patients are generally coagulopathic
- Respiratory: mild hypothermia = tachypnea; moderate hypothermia = decreased cilliary function and O2 consumption
- Cardiac: mild hypothermia = tachycardia and HTN; moderate hypothermia = bradycardia, interval prolongation, *Osborne waves, ST segment changes; severe = profound bradycardia and asystole
*Osborne wave amplitude is inversely proportional to temperature. Osborne waves are also correlated to increased risk of ventricular arrhythmia.
Tx: OK to intubate if needed, consider 1/2 dose RSI meds. Don't use LR as hepatic metabolism will be decreased resulting in increased lactate. Rewarming is key. Mild hypothermia requires blankets and wet clothing removal. Moderate hypothermia requires surface warming, warm/humidified oxygen. Severe hypothermia requires arctic sun, ECMO, dialysis or mediastinal irrigation.
In cardiac arrest situations, it is OK to delay initiation of CPR for as much as 10 minutes, as the cold decreases cellular metabolism which is protective in cardiac arrest (Gordon, et al. Resuscitation 2015). General recommendations are to not initiate CPR for PEA, as true PEA tends to be transient, and it may in fact just be difficult to palpate the perfusing rhythm through the cold. The European Resuscitation Council recommends against ACLS drugs until rewarmed to 30C, and they recommend to shock no more than 3x unless warmed past 30C.
EM-Peds Lecture with dr. Fananapazir
Case 1 - 7mo F with fever and a UTI
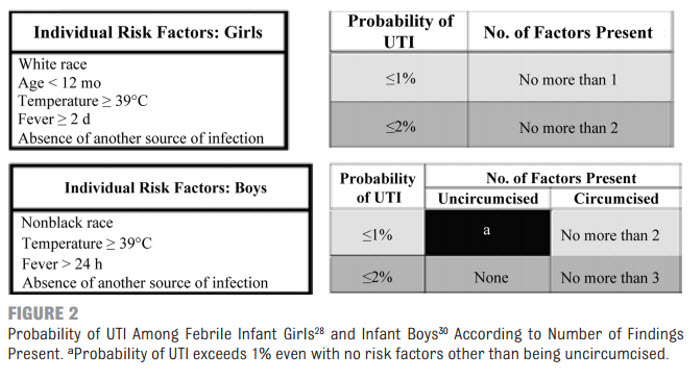
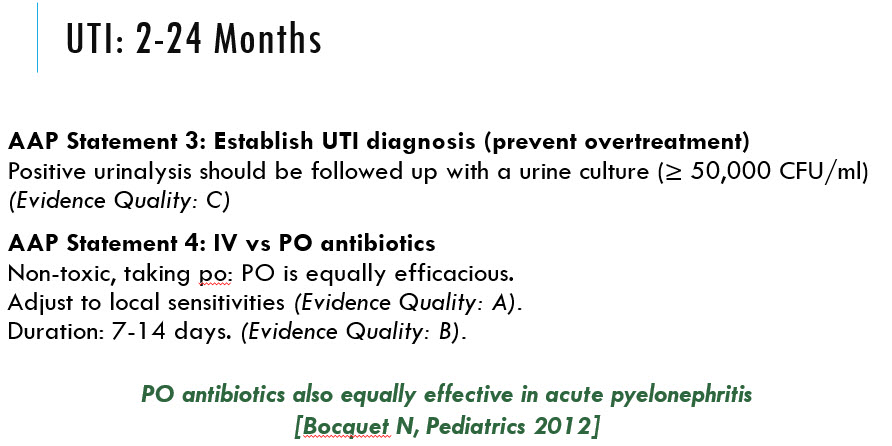
UTI (2-24 mo age group)
UTIs are increasing in prevalence in this age group. Signs and symptoms include:
- Poor feeding
- Vomiting
- Strong smelling urine
- Abdominal pain
- Irritability
Case 2 - 18mo M fever x 5 days at home. Febrile to 103.6 and noted to have cracked lips, rash on trunk, hands and feet.
Ddx includes: UTI, URI, Scarlet Fever, Kawasaki's Disease
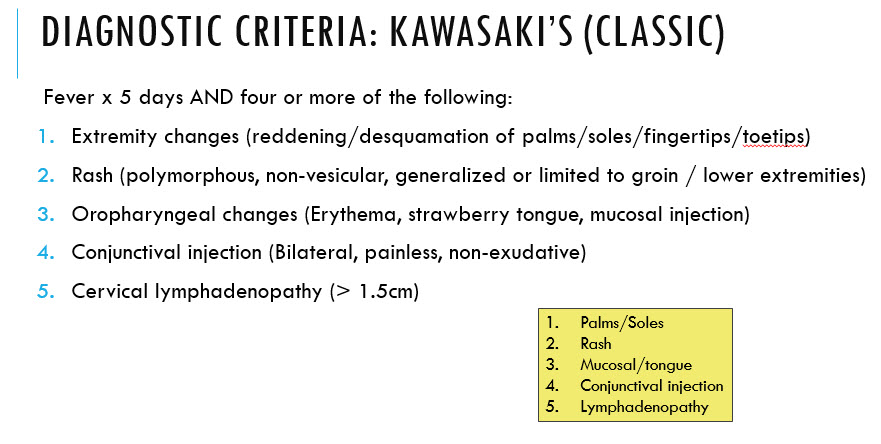
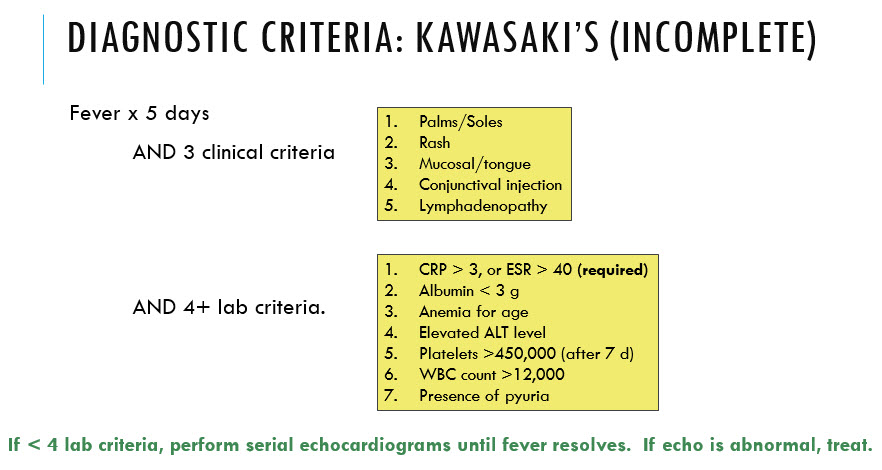
Kawasaki Disease = an acute, febrile, vasculitic syndrome of unknown etiology associated with coronary artery aneurysm in 25% of untreated patients. It is the leading cause of acquired heart disease in children in the US. Peak age of diagnosis is 18-24 mo, with 90% of patients presenting younger than 5yo.
Tx includes IVIG, aspirin, and can consider corticosteroids or other biologic agents in refractory cases. Patients require echo at time of diagnosis, at 2 weeks, and at 6-8 weeks after illness onset looking for coronary artery aneurysm.
ABEM: Ethical Issues of Resuscitation with Dr. Marco
The most important factor in OHCA survival is down time. Patients have a 27% chance of survival to hospital discharge if ACLS initiated within 8 minutes of arrest. Mortality increases by 3% for each passing minute without ACLS. These numbers are increasing, and ethical issues surrounding resuscitation will only grow more prevalent.
DNR (Do Not Resuscitate)
It's important to remember a patient's wishes trump any particular document (assuming they have decision making capacity), whether desiring resuscitation or not. Similarly, a physician is under no obligation to resuscitate in medically futile situations. According to the AMA Council on Ethical and Judicial Affairs: "CPR may be withheld when efforts to resuscitate a patient are judged by the treating physician to be futile." A report by the Hastings Center agrees. And further, according to ACEP policy: there is no ethical obligation to render treatment physicians judge to have no realistic likelihood of medical benefit to a patient.
Family presence at end-of-life care
The year 2000 AHA guidelines advocate for family witnessed resuscitations. In one study, 64% of families surveyed felt their presence was beneficial to their dying loved one, and that it helped the family better adjust to the grieving process. Resident physicians are the most hesitant to involve families in resuscitations, generally out of fear of 'messing up' or needing to ask questions. However, in a study by Pasquale from 2010, all family members present for trauma resuscitations stated they would be present again if given the opportunity, and that they suffered no ill effects psychologically.
Some guidelines to consider for family witnessed resuscitations:
- Assign a staff member to accompany the family
- Communicate the family's wishes
- Prepare the family for what they are about to see
- Attend to the family during the resuscitation
- Involve the family in decisions made
- Involve the family in declaration of death and aftercare