Grand Rounds Recap - 7/20/2016
/Faculty Lecture with Dr. Knight
Part I: Evaluation and Management of Seizures: Basic Principles
Check a finger stick glucose
Airway, Breathing, Circulation
IM versus IV therapy for Pre-Hospital Status Epilepticus: IM midazolam is as good as IV lorazepam, don’t wait for the IV if you can’t get one
Second-line medications for seizures and status epilepticus
Levetiracetam 60mg/kg IV (over 15 min)
Fosphenytoin 20mg/kg (150mg/min)
Depakote 40mg/kg IV (3-6 mk/kg/min)
Home medications
Consider ESETT Study Enrollment (Inclusion Criteria)
Patients greater than or equal to 2 years of age
Witnessed to have a clinically apparent seizure in the ED, 5-30 minutes after receiving an adequate dose of benzodiazepines:
10 mg of midazolam IV or IM
4 mg of lorazepam IV
10 mg of diazepam IV
For patients < 40 kg: 0.3 mg/kg of diazepam IV, 0.1 mg/kg of lorazepam IV, 0.3 mg/kg of midazolam IM (0.2 mg/kg IV)
- Contact research personel if you think a patient may be eligible
- Obtain serum level of any prescribed AEDs to facilitate outpatient follow up
Look for the underlying cause of the seizure! Do not assume that the cause is simply non-compliance
What is Status Epilepticus?
- A seizure lasting longer than 5 minutes. If you didn’t see the beginning of the seizure and they’re being brought in to the ED, assume they are in status
- More than 1 seizure without return to neurologic baseline
When to call neurology?
- You found something abnormal in your work up
- There is an usual feature to the presentation or seizure
Should you start AEDs in the ED?
- Not recommended if they don’t have close follow up with neurology
- Don’t routinely start after the first isolated seizure
- Benzodiazepine taper or burst has no evidence
Don’t forget to give a patient that is being discharged home appropriate safety precautions.
- Do not drive until cleared by neurology (Ohio Law is 3 months seizure free)
- No alcohol
- No showering, bathing, or swimming alone
Part II: Things that scare me.
Fear can be crippling. The purpose of fear is to help you manage a real threat: fight or flight
A debrief is huge after you’ve had a bad case or a case that made you afraid. Go for a walk. Find someone to talk to
What still scares you? What you’re not prepared for
- The sick neonate
- Bad airway
How do you get over this?
- Identify the fear. What exactly is it that scares you about this? Tackle that, learn about it, lessen your fear
- What are you telling yourself about this? Are you approaching this from a positive or negative place? Optimism or pessimism? Are you exaggerating the situation?
Don’t forget, it’s also fear inducing to be a patient on the receiving end of a procedure or being “on the pointy end of the needle"
Oral Boards Cases
Oral Boards with Jeff Hill, MD
Case 1: Chest Pain at ABEM Rural Hospital
70 year old male in Amish attire sitting in the bed presenting for exertional chest pain concerning for ACS. He has mild ACS. EKG shows posterior STEMI. There is no cath lab at this facility and you cannot get the patient to a cath lab in under 60 minutes. How do you manage it?
- Alteplase or Tenecteplase for Thrombolysis
Case 2:
74 M with SOB, pulmonary edema on CXR, and severe hypertension.
EKG: T wave inversions (inferior leads) with LVH with strain pattern in precordium - no change compared to previous.
Troponin - 0.12
BNP 1124
Diagnosis: Flash pulmonary edema
Management: Nitroglycerin gtt, Bilevel, Diuretics (at least their home dose IV or if not on diuretics, 40-60mg IV furosemide)
Oral Boards with Dr. Ronan-Bentle
54 yo M presents with chest pain x 5 hours concerning for ACS
EKG: Left bundle that meets Sgarbossa criteria
Management: 4mg IV morphine, 600 mg oral plavix, 324 mg aspirin, heparin gtt (bolus and infusion)
A new left bundle branch block is always pathologic and concerning for new ischemia. In an established LBBB, the Sgarbossa Criteria can help you to determine if the patient is having a STEMI.
Original Sgarbossa Criteria:
- Concordant ST elevation > 1mm in leads with a positive QRS complex (score 5)
- Concordant ST depression > 1mm in V1-V3 (score 3)
- Excessively discordant ST elevation > 5mm in leads with a negative QRS complex (score 2)
Total score of ≥3 is reported to have a specificity of 90% for diagnosing MI.
Modified Criteria:
- ≥1 lead with ≥1 mm of concordant ST elevation
- ≥1 lead of V1-V3 with ≥1 mm of concordant ST depression
- ≥1 lead anywhere with ≥1 mm ST elevation and proportionally excessive discordant STE, as defined by 25% of the depth of the preceding S wave
R4 Simulation with Drs. Boyer, DeVries and Winders
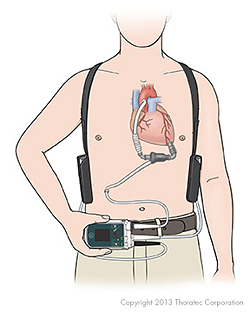
The case: LVAD patient in shock with MAPs in the 40s. Evidence of drive line infection on exam.
Initial management:
- Obtain a MAP by inflating a BP cuff on the patient’s arm and then listening for the “whir” of the device over the brachial artery using a doppler. Have a low threshold for invasive BP monitoring in a critically ill LVAD patient
- Contact the LVAD coordinator (contact should be on the device) and verify that the device is functioning by auscultation
- Assess the patient.
- EKG: Dysrhythmias can be treated the same as in patients without an LVAD. Medications and electrical cardioversion are all fair game
- Initiate appropriate lab work-up including LDH (lysis) and INR (thrombosis)
- Assess LVAD parameters
- Decreased flow: consider hypovolemia, bleeding (GI bleeds are common, 40% of patients will have at least one - do a rectal exam), RV failure (LVAD patients are dependent on preload and RV function), tamponade, and pneumothorax
- Elevated flow: consider sepsis
- Elevated power: consider pump thrombosis
- Low pulse index: consider a suction event or decreased LV function for another reason (worsening heart failure, ischemia, etc)
- Empiric treatment: 250-500 mL boluses as needed, antibiotics etc.
Other considerations:
- Get an LDH, extreme spikes in LDH can be sign of pump thrombosis. Urinalysis can also give you a sense for if someone has hemolysis due to thrombosis
- There may be two processes going on. Sepsis puts these patients at higher risk of thrombosis
A note about suction events:
This is often due to hypovolemia causing the LV to collapse around the intake canula of the LVAD. This can induce ventricular arrhythmias and syncope
When a suction event occurs you may see a decrease in the pulse index on the LVAD. In addition, the RPM will also drop to lowest set rate to try to resolve the suction event (allowing the LV to refill with blood). It will then re-ramp itself up
R2 Case Follow-up with Dr. Continenza
The case: A middle age male presents after a car accident with history suspicious for syncope and slight head trauma during the accident presents the next day with mild unilateral extremity weakness and ataxia present on his left side. CT head shows masses with vasogenic edema. MRI showed 3 enhancing lesions concerning for metastatic disease. He was given dexamethasone and admitted. CT to look for primary malignancy shows paratracheal mass - found to be NSCLC
Topic: Oncologic Emergencies in the ED
Brain Metastases:
- Brain mets are most commonly from: lung, melanoma, renal, breast cancer (ductal), colon
- 60% of new brain mets with unknown primary are from the lung
- Presentation: 50% have headache (but less than 1% of all HA patients presenting to the ED have a brain met), focal deficit, seizure, N/V, AMS
ED Management:
- Stabilization: A,B,C
- Corticosteroids: dexamethasone 4-8 mg with the goal to reduce vasogenic edema
- Manage ICP: 3% saline, elevated head, avoid hypercapnea
- Empiric AEDs are controversial and not routinely recommended
SVC Syndrome:
Obstruction of blood flow through the SVC causing elevated venous pressure in the upper body. This is most commonly from external compression but thrombosis can also occur
Responsible malignancies: lung 70%, lymphoma 20%
Symptoms: facial swelling, arm swelling, distended neck and chest veins, cough, dyspnea
Management: If thrombosis you could consider heparini. Stenting is an option for compressive lesions
Malignant Pericardial Effusion:
- Occurs in 20-34% of cancer patients but the majority are small and asymptomatic.
- Physiologically the pericardium can accommodate and tolerate up to 2L if chronic, however acute increases can cause tamponade.
- Management: Evaluate for tamponade. Symptoms include: dyspnea, tachycardia, chest pain.
- Beck’s Triad:
- Muffled heart sounds
- Elevated JVP
- Hypotension
- Rare findings: Pulsus paradoxes, Electrical Alternans
- Management: Fluids, pericardiocentesis, drainage catheter, pericardial window
Caution with intubation: induction agents and increased intrathoracic pressure can further reduce preload.
Taming the SRU Case Follow-up with Dr. Gorder
The case: 30 yo female with > 95% TBSA burns presents in full cardiac arrest from a house fire. Arrives in PEA undergoing CPR, unknown down-time, king airway and tibial IO in place, given epinephrine x 2 prior to arrival. The patient was given Cyanokit but ultimately did not survive.
Topics: Smoke Inhalation Injuries, Chemical Asphyxiation, Treatments and Antidotes
Why do people die in house fires? The majority die from respiratory injuries
- Upper airway: Thermal injuries
- The heat capacity of air is low - so typically injury occurs above the glottis
- This takes minutes to hours to develop
- Swelling may be exacerbated by necessary fluid resuscitation
- Early intubation should be considered
- Lower airway
- Smoke related toxins causing damage to capillary and endothelial membranes and surfactant producing cells
- This causes disruption of mucociliary transportation, surfactant production, oxygenation and ventilation
- Can occur up to 72 hours after the initial injury, consider prolonged monitoring for severe cases
- Chemical asphyxiation
- Carbon Monoxide
- Binds to hemoglobin with 200x greater affinity than oxygen
- Carboxyhemoglobin is in the infrared spectrum so pulse oximetry cannot differentiate and the patient may have normal saturations
- Treatment is 100% FiO2
- Cyanide
- Method of destruction
- Binds to metalloenzymes that are co-factors in electron transport and oxidative phosphorylation
- Inactivates cytochrome oxidase
- Uncouples mitochondrial oxidative phosphorylation
- Inhibits cellular respiration
- Sources of cyanide
- Combustion of furniture and other household items
- Iatrogenic sources (nitroprusside gtt)
- Food (i.e. apple seeds)
- If CN level greater than 40, mortality is extremely high
- In a study comparing house fire victims to controls, it was more common for people who died to have high cyanide levels than high CO levels
- Correlation identified between elevated CN and lactate
- Symptoms of CN poisoning
- Flushing, tachycardia, tachypnea, headache
- Profound circulatory failure
- There is no good test for CN in real time in the ED
- When to suspect: inappropriately high lactate, severe metabolic acidosis
- Assume all critically ill unstable patients from a house fire or industrial fire have both CO and CN poisoning and treat as such
- How to treat it:
- Traditionally: amyl or aodium nitrate induced methemoglobinemia which binds cyanide - however they cause hypotension and methemoglobinemia will further worsen oxygen delivery
- Sodium thiosulfate will bind cyanide for excretion
- What we use now: Cyanokit - combines with CN with hydroxocobalamin to form cyanocobalamin
- Give 5 gms - 2.5 gm in 100 mL LR x 2, each dose infuses over 10 minutes
- Cyanokit turns everything red (skin, urine, secretions etc), this also adversely effect all labs that require colorimetry, but if you need it, use it
- The patient may experience transient hypertension
- Does it work?
- French 8 year retrospective review: given to 101 patients with possible CN (hypotensive, awake, cardiac arrest)
- 21 of the 28 people who arrested got ROSC
- 9/12 “refractory" hemodynamically unstable patients became more stable
- US Study: CN given to all smoke-inhalation patients. 67% of the patients that were later found to have elevated CN levels that got cyanokit survived
- French 8 year retrospective review: given to 101 patients with possible CN (hypotensive, awake, cardiac arrest)
- Method of destruction
- Carbon Monoxide
What is an unsurvivable burn?
- Modified Baux score = Percent of TBSA burned + Age + 17 points for inhalation injuries. Greater than 140 is considered unsurvivable
- As a result of advancements in burn surgery, the score was increased to 160
- Recommendation of burn specialists - consult a specialist before deciding that a burn is unsurvivable