Back to the Basics: Demystifying the UA
/Amongst the various diagnostic studies that can be obtained in the ED, urinalysis is a virtually ubiquitous test. Urine itself reflects the functioning of the human body in both health and disease and the values it comprises can give us information regarding a myriad of conditions from infections, metabolic or endocrine derangements, and toxidromes to neoplastic processes and pregnancy. Despite this, many of the elements of even the standard urinalysis are often overlooked and underappreciated. In this talk we will explore some of these values and hopefully gain a renewed respect for the “golden cup of answers” and all that it may reveal.
Elements of Urinalysis
Let’s take a few moments to review the values that are tested on a standard urinalysis dipstick.(1,2)
Macroscopic
Color (reference yellow/straw):
Color can be abnormal in a wide range of pathology. Amber color can indicate concentration as seen with dehydration. Red urine can indicate hematuria, myoglobinuria, or may be explained by something as benign as the sliced beets your patient had with their most recent meal.
Clarity (reference clear):
Normal urine is clear, but can become turbid with various types of contaminants such as cellular debris, casts, crystals, or protein, and vaginal discharge, bacteria, or sperm.
Specific Gravity (reference 1.005 - 1.035):
In the broadest sense, specific gravity is a term that describes the density of a given substance relative to a reference substance, usually water. In physiologic terms, this value reflects the kidney’s ability to concentrate urine as well as the body’s overall hydration status. Low values are seen when urine is dilute, such as with diabetes insipidus or acute tubular necrosis, and high values indicate concentration or increased solutes such as in dehydration or proteinuria.
pH (reference 5.0 - 8.0):
pH can vary under normal circumstances by diet, with high protein diets yielding more acidic values. Acidic urine can also be the result of drugs, metabolic derangements such as DKA, dehydration, and diarrhea. Alkaline urine is found with various drugs (think salicylates and acetazolamide), infection with certain types of bacteria, and acute and chronic renal failure.
Protein (reference negative mg/dL)
Increased protein indicates impairment of the glomerular filtration apparatus. Common ED diagnoses that will exhibit proteinuria include congestive heart failure and diabetes, but it is also found in glomerulonephritis, pyelonephritis, preeclampsia and malignant hypertension. Albumin is the primary type of protein that will appear in urine, but other types can be found in states such as multiple myeloma. These other types are not detected on standard urine dipsticks.
Glucose (reference negative)
Glucose should be reabsorbed by the proximal tubules under normal conditions. When serum glucose concentration rises above 180 mg/dL then this reabsorptive capacity becomes overwhelmed and glucose will begin to appear in the urine. This is primarily observed in patients with diabetes mellitus, but can also be found in thyrotoxicosis, intravenous glucose administration, catecholamine surges, liver dysfunction, acute pancreatitis, and asphyxia (such as with CO poisoning).
Ketones (reference negative)
Ketone bodies reflect altered cellular metabolism when there is an inadequate supply of glucose to meet an increased metabolic demand. When glucose stores are depleted (or inaccessible as with type 1 diabetes), cells turn to using lipids instead, and ketones are the breakdown product of that process. They are commonly elevated in vomiting, diarrhea, and malnutrition, as well as pregnancy and hyperthyroidism, and are part of the diagnostic criteria for DKA.
Bilirubin (reference negative) and Urobilinogen (reference 0.2 - 1.0/EU/dL)
Bilirubin is a breakdown product of hemoglobin, and is normally reduced in the intestine to be excreted in urine as urobilinogen. Normally there is no bilirubin in urine, but when present it indicates liver disease. The pattern of obstructive disease includes elevated bilirubin and low urobilinogen. Hemolytic processes may show elevated urobilinogen as more hemoglobin than normal is processed. Urobilinogen can also be elevated when damage to liver parenchyma prevents its metabolism back to bilirubin. Specific processes include hepatitis, cirrhosis, pancreatic cancer, and choledocholithiasis.
Blood (reference negative)
Blood can be present in three possible forms: hematuria (results from whole red blood cells), hemoglobinuria (free hemoglobin), and myoglobinuria. A few red blood cells per HPF is normal in urine, but gross hematuria or myoglobinuria is unmistakeable even by simple visual inspection of its color. Specific conditions that can cause hematuria include many renal disorders such as calculi, neoplasms, infection, and drugs. Myoglobinuria will appear as blood on macroscopic exam with an incongruently small number of red blood cells on microscopic analysis and is usually the result of muscular trauma.
Nitrite (reference negative) and Leukocyte esterase (reference negative)
These values are the hallmarks of urinary tract infection. Nitrite is a product of the conversion of endogenous nitrates to nitrites and has high specificity for gram negative bacteriuria. Leukocyte esterase is an enzyme produced by white blood cells, usually in response to infection.
Microscopic
RBCs (reference 0-3/HPF)
Red blood cells in urine can be transient but normal in pediatrics, but in adult patients requires further evaluation. The source can be either glomerular or non-glomerular (supported by the presence or absence of RBC casts, respectively), or extra-renal (consider renal calculi, neoplasms, trauma, and infections).
WBCs (reference 0-5/HPF)
Generally, the presence of white blood cells indicates infection, which is often supported by nitrites and/or leukocyte esterase and the presence of bacteria. Sterile pyuria, or WBCs without these concomitant features, can be seen in patients with UTI being treated with antimicrobials, contaminated samples, and infection with atypical organisms such as Chlamydia and tuberculosis.
Squamous Epithelium (reference 0-5/HPF)
Elevated squamous epithelial cells should make the clinician suspicious of contaminated sample.
Bacteria (reference none/HPF)
Bacteria are usually a strong indicator of infection, particularly when present along with the other markers discussed above. When present with WBC casts, the clinician should suspect pyelonephritis as opposed to simple cystitis. When present together with a high number of squamous epithelial cells, the result should be regarded as contaminant.
Mucus (reference none/HPF)
Mucus presence is nonspecific but can be elevated in a variety of conditions including infection, neoplasms, and renal calculi. It can also be a contaminant from vaginal or anal sources.
Sediment (reference none)
Sediments are a mixed-bag of cells, crystals, casts, and microorganisms that give clues to what structures along the urinary tract may be involved, what organisms are present, and what physiologic conditions exist in the kidneys, bladder, and body beyond the urinary system.
Clinical Cases
Having reviewed the above information, let’s now attempt to apply it to some cases. However, let’s do so with a twist: we’ll work backwards from the urinalysis results to history and physical exam and then discuss other tests and treatments that you might wish to order based on your findings.
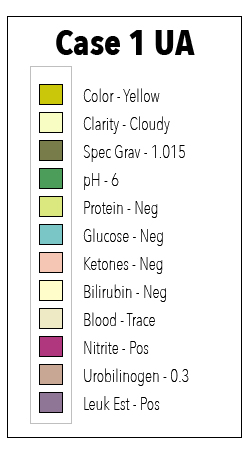
Case 1
What is your differential for this patient based only on what you see on urinalysis? Certainly urinary tract infection seems likely given the cloudiness and positive nitrites and leukocyte esterase. However, let’s not stop there since we have at least one other abnormality: trace blood. This could still go along with an infectious picture, but we start to have to consider other entities such as stones, neoplasm, or drugs. However, for this case let’s let Occam’s razor do some work for us and put UTI at the top of our list. We still don’t know where in the tract this infection may reside, but our urinalysis has more information yet to reveal in the microscopic analysis.
Microscopic results demonstrate 5 RBCs, 50 WBCs, 2 squam, WBC casts, and numerous gram negative rods. So this clearly appears to be an infection based solely on what we can determine on UA. Even better, we are able to differentiate lower UTI from upper based on the microscopic analysis showing WBC casts. Recall that casts are a type of sediment that are formed in the renal tubules. Therefore, if we’re seeing casts there must be tubular pathology of some kind. RBC casts might make us think of glomerulonephritis, but in this case the WBC casts clearly point to pyelonephritis when taken in context with the other findings. In an equivocal sample you should also make note of the specific gravity because in the case of very concentrated or dilute samples one might get false positive or false negative results.(3)
We’ve practically made our diagnosis without ever speaking to or examining our patient, but let’s not forget the importance of the history and physical exam. In interviewing your patient you find a 22-year-old female who is otherwise healthy with no meds or allergies who complains of dysuria for the past week and flank pain and fevers since yesterday. On exam she is febrile to 101.2, hemodynamically stable, and has suprapubic and left flank tenderness.
What factors should we consider when initiating treatment? Patient factors and microbiology will drive your decision, and in this case we have a young woman with no comorbidities or allergies with what appears to be uncomplicated pyelonephritis. This patient will likely be a candidate for outpatient therapy and antibiotic choice should offer gram negative coverage, likely a fluoroquinolone or cephalosporin. Let’s for the sake of argument say that there were no casts on UA, and our patient had no fevers or flank pain. In other words simple cystitis. You would want to be sure that she was symptomatic before prescribing antibiotics as studies have shown that any one of the UA findings in isolation (nitrites, leukocyte esterase, bacteria) without symptoms does not indicate a clinically significant UTI and should not be treated with antimicrobials.(4)
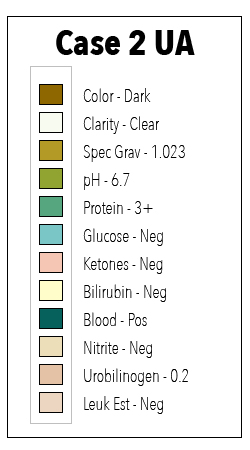
Case 2
Again we’ll start with the UA and build a differential based on the values. Here we see dark urine that is positive for blood and protein. The differential for hematuria and proteinuria is broad, including transient proteinurias (febrile and exercise-induced), orthostatic and postural proteinuria, post-streptococcal glomerulonephritis, Alport syndrome, and a host of glomerular and tubulointerstitial diseases.4 It looks like this case may not be as straightforward as our last one, so we’re going to need the history and physical in order to make the diagnosis. First, let’s be sure to check the microscopic analysis, which shows numerous RBCs, RBC casts, and no WBCs or bacteria. Again, it is important to note the specific gravity when interpreting results as very concentrated or very dilute samples can give false positives or negatives, respectively.(5)
Our patient turns out to be a 10 year old boy with no prior medical history who comes with poorly localized abdominal pain, fevers, malaise, and facial swelling. We discover that three weeks ago he had a sore throat that resolved without medical attention. On physical exam he appears ill, is hypertensive, and has periorbital and pedal edema, but normal heart and lung sounds.
The case appears to be one of acute post-streptococcal glomerulonephritis. Additional studies for this patient will also include CBC and renal panel in the ED, and he will likely be admitted for further testing, formal renal ultrasound, and possibly biopsy. The only management in the acute setting is supportive care.
Conclusion
Urinalysis is one of the most versatile and readily available diagnostic tests that we as clinicians have available. Many of the important elements are assessed visually, or at most require widely available dipstick tests, and so the UA can provide answers even in rural or austere settings. By understanding what each element can tell us individually, recognizing the patterns that they present in combination, and placing that information into the clinical context of our patient, there is almost no disease process in which the urinalysis cannot help make a diagnosis.