Grand Rounds Recap 06.02.21
/Attending Case Follow-Up:Nec Fasc - Attending Case Follow-Up: AMS - Attending Case Follow-Up: Evan’s Syndrome - R2 CPC - Quality in Operations Series - Gathering Sensitive Information - R3 Taming the SRU - R4 Capstone
ATTENDING CASE FOLLOW-UP WITH DR. KNIGHT
Female in her 60s with right gluteal abscess s/p I&D and packing who presents with continued pain. Physical exam is largely reassuring, abscess near but does not involve the anal verge. Rectal exam reassuring. Labs, IVF, pain medications, and antibiotics ordered. She felt improved afterwards and was discharged with prescriptions. Walked out of the ED. Presents again in 3 days and arrests in the ED.
Trust but verify - there is a fine line between providing learner autonomy and having enough supervision to avoid patient misses or harm. Find and welcome this balance.
Double and triple check labs for patients before disposition!!
Fear the dirty dishwater drainage.
Female in her 30s with recently confirmed IUP in the OB clinic presents with RLQ abdominal pain. Bedside transabdominal ultrasound demonstrated free fluid in the pelvis and RUQ. Consult placed to gynecology and acute care surgery. As plans are being made she becomes more hypotensive and is taken urgently to the OR. Confirmed cornual ectopic pregnancy.
Trust but verify - trust your clinical gestalt and concern. Relay this concern to your consultants and stand your ground if you believe a particular diagnosis should be ruled out/an intervention should be concerned. Don’t hesitate to escalate to the attending if needed, but use this sparingly and appropriately!
ATTENDING CASE FOLLOW-UP WITH DR. ROCHE
Male in his 40s with HIV/AIDS brought in by sister for confusion who reports she has been active strangely, unsteady, and confused for the past 2 days. Has been complaining of a headache and photophobia without fevers or vomiting. Possible history of meningitis. Exam is notable for cachectic man with temporal wasting, unsteady gait. Old medication list includes ART, Bactrim, fluconazole, nystatin mouthwash. CXR, UA, CT head w/wo negative.
Remain objective about whether a procedure is needed
If this were the only patient in the department, would I do it?
If I could get someone else to do it (R2), would I do it?
If this were my family member, would I do it?
Tomorrow, will I wish I had done it?
CAVEAT: we have a responsibility to each person who presents to the ED - to see them, to move them through so that other patients can be seen
Lean into the procedure
Just get it done, quiet moments are rare
Avoid the emotional and intellectual drain of a pending procedure
Harness the post-procedure high
Versed and a long needle later...opening pressure is 45cmH20. Labs then result with platelet count of 18.
Always take a minute, don’t rush the prep - be safe
If you rush and aren’t sterile, but honest in your documentation
If you screw up don’t hide it...this will crush you
Testing for Cryptococcus:
Sensitivity of serum antigen (CrAg) is close to 100% but may remain positive for years after disease
LP evaluates for elevated ICP and other causes of meningitis/encephalitis (may be normal CSF appearance ¼ of the time)
Thrombocytopenia and HIV/AIDS
Not uncommon finding at presentation
Up to 40% occurrence in advanced AIDS
Often improves with initiation of ART
Hospital course: patient received Amphotericin B and flucytosine IV. Serial LPs x5 with improved function and mentation but discharged to nursing facility after 2 weeks of inpatient. Discharged on fluconazole treatment for 8 weeks and restarted ART at 1 month.
ATTENDING CASE FOLLOW-UP WITH DR. FREIERMUTH
Female in her 20s with lightheadedness, worse with standing up, who reports heavy vaginal bleeding for the past 4 days and requires changing a super tampon every 2-3 hours. These symptoms are not consistent with her normal menstrual cycle, she is not sexually active. She also noted petechiae on bilateral feet and ankles with pale skin. ROS positive for general malaise, palpitations, slight headache, popped a pimple yesterday and her face bled for hours.
Differential includes: common things being common (ectopic pregnancy, fibroids, PCOS); petechiae (infection, autoimmune); trauma
Physical exam notable for tachycardia to 110s, scattered petechiae to bilateral ankles most notable around sock line that extends to dorsum of feet. Labs notable for hgb 7.7, plt 3, total bilirubin 3.5, INR 1.
ITP vs. TTP vs. DIC
Head CT negative, consulted hematology and intensivist. Given concern for hemolytic anemia +/- ITP, plan is for solumedrol 60mg, IVIG to start upstairs, and to avoid transfusion since she is not actively bleeding. Admitted to ICU.
Evans Syndrome
ITP plus autoimmune hemolytic anemia
Antibody destruction of blood cell lines
Discharged 6 days later with platelet count of 74 and a prednisone taper. At follow up she is noted to have CD4 25 with negative HIV. Has undergone extensive genetic and autoimmune testing without underlying cause revealed.
R2 CPC WITH Drs. frankenfeld & hill
Male in his 30s with PMH of depression who presents with 1 hour of nausea, vomiting, and 6/10 periumbilical abdominal pain without radiation. He does have a profound urge to defecate. Three episodes of NBNB emesis, no fevers but feels sweaty. Has an upcoming divorce with his wife. ROS notable for diaphoresis, palpitations, depression, and suicidal ideation.
Vitals: HR 89, BP 129/90, RR 24, SpO2 100% on RA, T 34.7 axillary (repeat normothermic)
Physical exam: Diaphoretic, ill-appearing and in moderate distress. PERRL. Tachypneic with clear lungs bilaterally. Abdomen is minimally tender around the periumbilical region without guarding or rebound. Mood is depressed. Labs notable for K 3.0, CO2 14, Anion gap 20, Cr 1.39, pH 7.48, pCO2 25, lactate 3, salicylate 3. CBC, LFTs , INR, acetaminophen, ethanol otherwise unremarkable. UA was grossly bloody with proteinuria and positive nitrites (traumatic cath). EKG with no ischemic changes.
Update: Immediately after examining the patient he had a large bowel movement of orange diarrhea. Had an episode of hematemesis of ~500cc and became hypotensive. Taken to the SRU and repeat VBG notable for pH 7.12 / pCO2 46 / HCO3 15 / base deficit 14.2. EKG with A.fib without RVR.
...and then a test was ordered…
[quick interlude with some attending knowledge bombs]
Referred abdominal pain
Epigastric = celiac axis
Periumbilical = SMA axis
Lower abdominal = IMA axis
What organ systems are affected?
GI
Cardiovascular
Metabolic
Renal
What can affect all these systems and has an acute dynamic process?
Toxic, metabolic
What did they take? What could they have taken (access to which medications)?
Currently on albuterol inhaler, loratadine, sertraline
When did they take it? Are they manifesting a toxidrome?
Not particularly…
MUDPILES: methanol, iron, lactic acidosis, ethylene glycol, salicylate…
Iron overdose
Rare cause of OD in adults
Stage 1 (0-6h) - hematemesis/GI bleed with caustic ingestion and lethargy
Stage 2 (6-12h) - symptoms improve
Stage 3 (12-48h) - liver failure, coagulopathy, ANT, lactic acidosis, shock
Stage 4 (4-6wk) - gastric scarring if you survive
Toxic alcohol overdose
Propylene glycol - organic anti-freeze technology
Hyperosmolality
AGMA
Renal failure
Hypotension, seizure, coma, death
Ethylene glycol - inorganic anti-freeze technology
Hyperosmolality
intoxicating/inebriation
Dysrhythmias, QT prolongation w/calcium oxalate deposition and hypocalcemia
Renal failure
Salicylate
AGMA with respiratory alkalosis
Salicylate directly caustic to IG mucosa (GI bleed in 4% of patients who are admitted)
Can have associated conduction block abnormalities - atrial dysrhythmia, NSVT, varying heart blocks
Can have a delay in detection, especially with enteric coated aspirin
...iron level 797
Patient reports he took 100 tablets of iron. Decompensated and underwent whole bowel irrigation and chelation in the MICU. Had a downtrending iron level and was discharged on hospital day 9.
Formulations
Ferrous sulfate - 65mg elemental iron/tablet - is the most commonly used
Ferrous gluconate - 27mg elemental iron/tablet
Ferrous fumarate - 106mg elemental iron/tablet
Free iron is toxic → binds to transferrin.
Typically, transferrin is ~20-30% saturated and when ingestions go beyond this saturation you will see the toxic side effects. Also dependent upon total iron binding capacity.
Toxic iron can cause corrosion of GI lumen and cause hypovolemia and hemorrhagic shock.
It also concentrates in the mitochondria and interferes with oxidative phosphorylation - will severely impact anything that uses this (heart, brain, liver).
Dose-dependent toxicity
More dangerous in children with smaller doses
Asymptomatic with 20mg/kg ingestion
20-60mg/kg ingestion is only GI manifestations
60-120mg/kg will result in cardiac side effects (our patient!)
>120mg/kg is a lethal dose
See above for stages of iron toxicity!
Diagnostics
Iron level peaks at 2-6 hours
Body is great at shifting iron intracellularly, so have a high index of suspicion in the appropriate clinical context if your iron level comes back suspiciously low!
KUB as many iron-containing medications are radiopaque
Therapeutics
Fluids 10-20cc/kg
Chelation: deferoxamine
Indications are for >90umol/L, shock, systemic toxicity, AMS, acidosis
Dosing: IV 15mg/kg/hr, IM 50mg/kg Q6H...max 6g/24h
Pink-tinged urine
Whole bowel irrigation with polyethylene glycol solution
Insert an NG tube and insert 1.5-2L/hr
Bicarbonate for persistent acidosis
Ineffective therapies
Activated charcoal does NOT bind iron tablets
Dialysis will not eliminate iron alone, but can be used to eliminate chelated iron/deferoxamine complexes
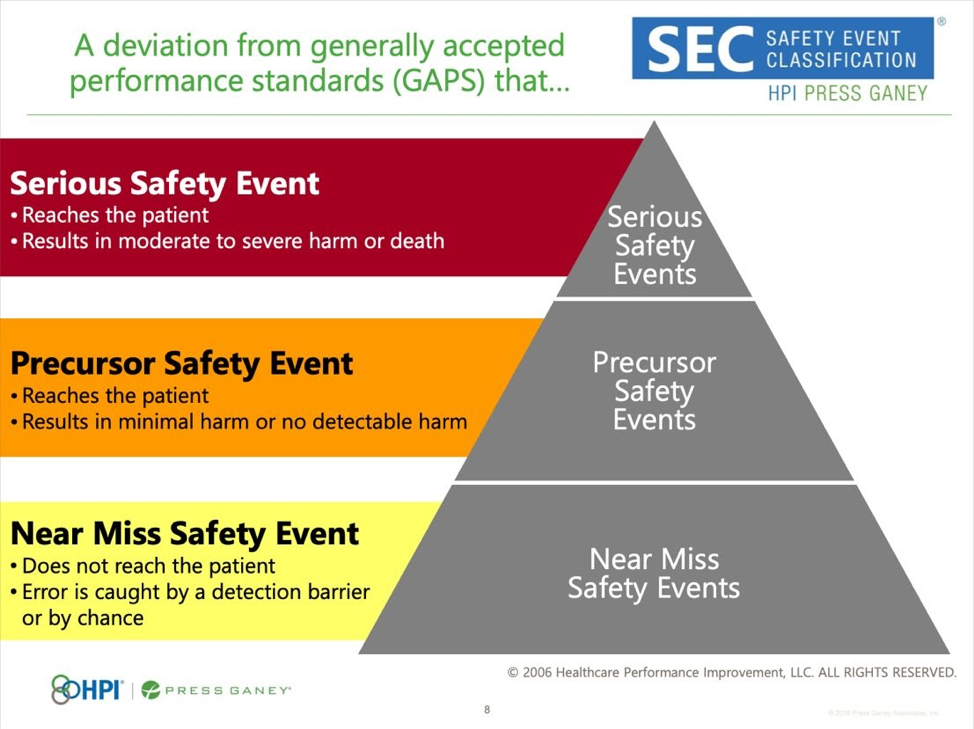
OPERATIONS QI UPDATE WITH DR. D.THOMPSON
How is patient safety relevant to you?
Emergency medicine = high risk for patient harm
Majority of safety events identified through Midas reports, mortality reviews, codes, word of mouth, etc.
Examples: medication errors, patient falls with injury, patient assaults, delays in care or delays in diagnosis, complications
Historically at UC each department had their own approach (M&M, case reviews)
Very siloed
Focused on individuals
Try to do the right things
Current and future state
Unified approach to patient safety
Focus on systems rather than individuals
Make it hard to get things wrong
Multiple patient safety models have been created by the Joint Commission, the National Quality Forum, and the WHO
UC Health chose a model for patient safety called Healthcare Performance Improvement, a division of Press Ganey (1100 health organizations who use this model as well)
Identify events from various sources and funnel/screen these events based on organization or individual culpability and level of harm to the patient - output is a classification system
IMPROVING HISTORY TAKING: GATHERING SENSITIVE INFORMATION WITH DR. FREIERMUTH
Importance of history
Adds context to the presentation
Guides your differential - 70% of diagnoses can be made by history alone
Minimizes unnecessary testing
Reveals behaviors that contribute to health which may need modification
First impressions matter
Clearly introduce yourself and your role on the care team (not everyone knows what a resident or attending is)
Sit down if possible (it’s less intimidating than standing over the patient and patients will perceive this as spending more time with them)
Try your best to let the patient talk (the average physician interrupts a patient after 18s)
Make eye contact (if charting while in the room, share your screen with the patient or make sure you are focused on them while asking questions)
Body language of a patient can add to your information gathering
Ask the patient about his/her/their preferred name
Tell me how you would like to be addressed…
Who do you have here with you in the room? Allow them to answer and ask about the relationships if only a name is stated. How are you related or how do you know each other? Is it OK if we discuss your complaint and medical history in front of said person?
Emergency Department visits are exhausting
People are here because they don’t feel well
Repetitive questions is frustrating - go in as a team when possible
Summarize what you have learned from the nurse/nursing note/EHR and then expand from there
Share wit the rest of the care team if a patient shares a preferred name/pronoun with you that is incongruous with EPIC
EHR - help or hindrance?
Information may not be accurate - must be verified
We are the head of the care team and should ensure PMH, surgeries, and social histories
Develop a system
Asking the same questions the same way each time ensures you don’t forget
Also decreases bias from assuming certain items won’t apply to certain types of patients
One study demonstrated that there is physician variability in history taking in ED chest pain patients (Academic Emerg Med 2006) varying based on gender, race, age, etc.
Framing your questions
Open ended vs leading
Non-judgmental tone
Practice so your own discomfort isn’t obvious
Some preface with explanation for why they are asking certain questions
Key portions of history
PMH - is the problem today new or an exacerbation of underlying disease
PSH - missing/altered organs
medications/allergies
Family history
Social history - living situation, substance use, sexual practices
Language for questioning
Where do you live? Who lives with you?
Do you ever have difficulty getting enough food to eat?
How much do you smoke per day?
How often do you drink alcohol/? How much do you typically drink on those days? Clarify use - beers come in different sizes and very different alcohol content
Questioning continued
Do you use any type of drugs, such as cocaine, marijuana, or heroin? Any pills that aren’t prescribed to you? Do you use needles to inject drugs? Avoid words such as illegal or illicit!
How many sexual partners have you had in the past 6 months? Do you have sex with men, women, or both? Do you use condoms or other barrier methods? How often? Sex can include vaginal, anal, oral, and use of other objects
Don’t forget about harm reduction
Discussion surrounding safer sex practices
Need for testing/treatment of partners when STI is a concern
Safer use of drugs
Don’t mix drugs, use with someone who can call for help if needed, clean needles and syringe exchanges, access to naloxone stocked in omnicell!
Majority of physicians and APPs have an X waiver to prescribe buprenorphine
ED resources
Early intervention team
Substance abuse team
Peer counselors offer their own experience
Referral to treatment
R3 TAMING THE SRU WITH DR. PULVINO
Male in his 50s with LKN 22:30 (2 hours PTA). Stroke with patient flaccid on the left and simultaneous ST elevations in multiple leads.
Stroke + STEMI?
Aortic dissection
LV aneurysm w/ embolic stroke
Septic emboli from endocarditis
STEMI is a red herring (pericarditis, old EKG findings, etc.)
Patient denies chest pain or shortness of breath, in no discomfort. Definitely having a stroke with left facial droop, left upper extremity weakness, left-sided neglect and mild dysarthria. CT head, CTA head, neck, chest, abdomen/pelvis ordered. Glucose 141. No ICH and stroke team is paged. CVICU team also paged given ST elevations on pre-hospital EKG - cath lab not activated due to lack of symptoms.
Radiology calls and notes a complete R M1 occlusion. EKG in ED does not demonstrate STEMI. Bedside echo performed by CVICU fellow demonstrates mitral valve vegetation with grossly normal LV function. Concerned about endocarditis at this time, and infectious work up is initiated in addition to antibiotics ordered. Patient receives aspirin 325mg.
Stroke team does not recommend tPA given concern for infectious endocarditis, and the patient goes to neuro IR. TICI 2b reperfusion achieved, NIH remained 9 (from 10 on ED presentation). Blood cultures positive for E.faecalis. Has a complicated hospital course
Infective endocarditis
Diagnosis - Duke criteria
Management
Blood cultures to target abx therapy
Antibiotics should be administered empirically
Supportive care
Consults to cardiology and CT surgery for possible valve replacement
Stroke from infective endocarditis
The brain is one of the most frequent sites of embolization in left-sided endocarditis
Duke criteria are often no present or noticed
Thrombolytics are contraindicated, but thrombectomy is an option
Antibiotics decrease risk of embolization
Antiplatelets and anticoagulation are controversial
STEMI in endocarditis
Very rare, mechanism is usually embolic
Thrombolytics = big risk of bleeding
PCI can be helpful
Case report of nonobstructive STEMI with endocarditis and ICH
Takeaways
No thrombolytics for endocarditis
Treatment is fast antibiotics and individualized supportive care
Take a full history (and get a full set of vital signs!)
Ultrasound is your friend
Don’t be afraid to call for help
R4 CAPSTONE: LESSONS LEARNED ALONG THE WAY WITH DR. MAND
Learn from your mistakes
Intellectualize the criticism
Open, non-biased communication
Self-forgiveness
Become an expert/prevent recurrences
Sometimes, despite your best efforts, good people die
How you perceive yourself may not be how others view you
When loved ones get ill, don’t be their doctor, be their support. Be their family.
Imposter syndrome is
“The internal belief that one is not intelligent or successful despite a history of high achievement”
“a collection of feelings of inadequacy that persist despite evident success”
Don’t let imposter syndrome hold you back
Does not necessarily correlate with low self-esteem or lack of self-confidence
Be self aware, reframe your mindset, recognize your own value, seek support
Progress at your own pace
Embrace your emotions
Find your people
Focus on the GOOD you do