Grand Rounds Recap 6.7.23
/
Taming the sru WITH dr. diaz
Case: Middle aged patient with esophageal varices, recently banded presents for large volume hematemesis in hypovolemic shock. She required MAC line placement, MTP activation and transfusion. She was intubated for airway protection and the decision was made to perform balloon tamponade with placement of a Minnesota Tube.
Balloon Tamponade for Massive UGI Bleed:
- Minnesota tube vs Blakemore tube: MT has extra isolated esophageal aspiration port, as well as more air in gastric balloon
- Indications: acute UGI (mostly variceal) unresponsive to medical therapy
- Contraindications: known esophageal stricture, recent surgery at the GE junction
- Complications: esophageal perforation/erosions, aspiration
Steps:
Intubate the patient. Recommend using rocuronium to give you time with the patient paralyzed.
Insert 3-way stopcocks to inflation ports
Test balloon in water to evaluate for leaks and deflate entirely
Prep tube: consider placing in bucket of ice to stiffen for easy placement, lubricate with jelly and consider bougie insertion into the distal port to ease guidance
Insert under direct visualization with video laryngoscope to 50cm
Inflate 50cc of air into gastric balloon
Obtain an xray to ensure gastric balloon is below diaphragm
Fully inflate to 500cc and clamp balloon port
Pull back until some resistance is felt, usually ~40cm, secure with ETT holder or tie Minnesota tube with 1-2lbs of tension to ensure appropriate placement
Aspirate from esophageal port and potential need for intervention
If planning to intervene, use cufflator to inflate balloon to 30mmHg
See AirCare Taming the SRU article: Balloon Tamponade of Variceal Hemorrhage
R4 Case Follow-up WITH dr. gressick
Case: Patient presented post-arrest from recurrent VT/VF secondary to STEMI in electrical storm.
Electrical storm: 3+ sustained episodes of VT, VF or appropriate ICD shocks during a 24 hour period
- Causes: drug toxicity, electrolyte disturbance, new/worsened heart failure, acute myocardial ischemia, thyrotoxicosis, QT prolongation
- Treatment: high-quality CPR if under arrest as well as appropriate use of cardioversion/defibrillation, amiodarone, magnesium, lidocaine
- Attenuation of sympathetic drive: esmolol (or other BB), avoid epinephrine, u/s-guided stellate ganglion blockade
- Treat the underlying cause
r1 clinical diagnostics: waveform capnography WITH dr. wilson
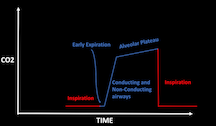
End-tidal CO2: Information we are getting: numerical CO2, which has to do with our metabolic rate and cardiac output
- Time of inspiration/expiration
- Information about air movement
Phase 0: inspiration
- CO2 should be 0 due to low amount of CO2 in normal air
Phase 1: early expiration, purely deadpace
- The air inside the patient rushes out of them driven by the spring-like recoil of the chest wall and lung parenchyma
Phase 2: mixing dead space and conducting airways
- Gas from the upper airways (poor in CO2) slowly gives way to mixed gas from the lower airways (rich in CO2)
- Alpha angle: transition point between airway gas and alveolar gas; once dead space has emptied, the remaining gas exchange is a passive mixing of the gas in the tubing and gas inside the alveoli
Phase 3: approach equilibrium, alveolar plateau
Phase 0: inspiration
Specific scenarios: Asthma exacerbation: sawtooth slope due to obstruction in bronchi; the dead space does not finish emptying by the time the next inspiration begins leading ot loss of the transition angle
Mechanical airway obstruction: inspiratory and expiratory flow will be affected; their is a less steep transition to inspiration demonstrating that the obstruction can’t be overcome even when a patient is ventilated
Emphysema: aleveolar slope is reversed; due to poor gas exchange and abnormally increased lung compliance, the alveolar gas exchanges very rapidly. The part of the curve that represents the arterial CO2 is the early peak, not the end-tidal value. After, gas in the ventilator tubing diffuses backwards into the patient, at which point an equilibrium between the higher CO2 in the patient and the lower CO2 in the ventilator circuit is reached which results in a gradual drop of the CO2 concentration
Pigtail capnogram: seen in poor lung compliance, as well as some pregnant women and obese patients. Sudden peak of pre-inspiratory expired CO2 due to sudden airway closure. The last few milliliters of CO2-rich gas is expired before the collapse of the lung parenchyma occludes the bronchi and puts an end to the escape of gas.
Clinical pathologic case WITH drs. haffner and bryant
Valproic Acid Toxicity with Hyperammonemic Encephalopathy
Valproic acid: antiepileptic agent
Blocks voltage-gated sodium channels
Increases brain GABA concentrations
No direct effect on GABA(A) receptors
Complex mechanism
Overdose can cause hyperammonemia
Small volume of distribution, at therapeutic levels, VPA is >80% protein bound
Serum levels:
50-100 ug/ml: therapeutic
>180: mental impairment
>450: serious intoxication
>850: coma likely
Diagnosis
Ammonia level, valproic acid level
Electrolytes and liver function tests
CK
Management
Supportive care: ABCs
Treat the source: stop valproic acid, consider charcoal, consider hemodialysis
Provide antidote: L-carnitine
Loading: 100mg/kg over 30 minutes
Maintenance: 15mg/kg every 3-4 hours
Consider naloxone, carbapenems (reduce effectiveness of valproic acid)
taming the sru WITH dr. wosiski-kuhn
Case: Critically ill patient presenting with profound metabolic acidosis from DKA who unfortunately necessitates intubation for airway protection and severe acute hypoxic respiratory failure.
Intubating DKA: try to avoid it if possible; high risk of cardiovascular collapse and arrest due to difficulty matching metabolic demand on ventilator and apneic period leads to CO2 retention and worsening overall acidosis
Correct hypovolemia; start with MAP >75
Attempt to correct metabolic derangements
Be prepared for emesis
Apneic ventilation with BVM
Large ETT to minimize airway resistance
As soon as ETT is secured, restart your hyperventilation to prevent arrest from CO2
Tidal volume 8cc/kg
High RR
Rocuronium- assists with ventilator synchrony
Consider giving bicarbonate prior to intubation if HCO3 <10