Grand Rounds Recap 11.16.22
/
R4 Capstone - Leading from the front WITH dr. Ijaz
Leaders deal with change
Setting direction involves creating a vision
Requires big picture thinking and shaping purpose of organization
Align People
Share the why you do what you do
Be consistent in your messaging
Be on the front line leading by example
Share your vulnerability
Leaders reveal their weaknesses so followers can establish trust and collaborate
Shows that you are genuine and approachable
Managers plan and budget
Planning and budgeting directly complements direction-setting.
This is how you develop strategies to accomplish your vision
Organize and hire individuals to complete roles that fit within the larger mission
Emotional Intelligence
Self-awareness
Know one’s emotions, strengths, weaknesses, drives, values and goals
Self confidence
Self assessment
Self regulation
Controlling or redirecting disruptive emotions and impulses
This is where the concept of “seek first to understand” comes into play
Empathy
Considering others’ feelings, especially when making decisions
This is when you see your colleague deal with a tough case. You reach out to cover their patients while they take a few moments for themselves
Motivation
Being driven to achieve for the sake of achievement
Passion for the work itself and for new challenges
Unflagging energy to improve
Optimism in face of failure
Social Skills
Managing relationships to move people in desired directions
Effectiveness in leading change
Persuasive
Networking
Building teams
Thoracic Outlet Syndrome WITH dr. stothers
Anatomy
Thoracic outlet bordered by clavicle, first rib, middle and anterior scalene muscles
Contents include subclavian artery, subclavian vein, three trunks of brachial plexus
Pathophysiology
Neurovascular compromise from compression of vascular structures or brachial plexus
Tumors
Anatomical variants (cervical rib, duplication of scalene muscles, hypertrophy of muscles)
Trauma (microtrauma from repetitive use vs. macrotrauma from blunt injury)
Clinical Presentation
Depends on the structures that are compressed
Brachial plexus (95%)
Subclavian vein (4%)
Subclavian artery (1%)
Thoracic duct (possible, but rarely reported)
Brachial plexus
Shooting/tingling/burning pain in the neck/shoulder, arm or hand, often not in a neurologic distribution
Present in professional athletes, violinists
Subclavian vein
Intermittent compression (McCleery Syndrome) - pain, redness and swelling
Chronic compression (Paget-Schroetter Syndrome)
Central venous thrombosis
Associated with young athletes
Subclavian artery
5 P’s: pain, pallor, paresthesias, pulselessness, paralysis
Often asymptomatic until repeat compression leads to proximal aneurysm formation -> thrombus development -> distal arterial emboli
Diagnosis
Physical exam
Upper extremity stress test
To diagnose neurogenic thoracic outlet syndrome, must perform for 3 minutes
Ultrasound
CXR for cervical rib
CT angiogram
Anterior scalene intramuscular block, may indicate neurogenic TOS
Treatment
Surgical debulking
Lifestyle modification
Anticoagulation
Anterior scalene intramuscular block
Litigation Stress WITH Dr. Gita Pensa
Emergency physicians are unprepared when it comes to litigation
Stressed defendants make more errors
Prepared defendants are better defendants
This will happen to most of us
Silence perpetuates stigma
It is the right thing to do
Good news
Less than 10% of cases go to trial
Punitive damages/personal asset losses are very rare
Rates of paid claims is down by 55%
Bad news
75-90% of us will be named at some point during career
Annually 7.4% of all physicians are sued
Threat of targeting personal assets is an increasingly used tactic
Highest payout states: NH, NY, NJ, RI, MA, IL, PA
The adverse event in medicine
Event leads to outcry, then denial, then intrusion, “working through”, and then completion
Can lead to acute stress, maladaptive behaviors, personality constriction, PTSD
Why litigation is difficult for physicians:
Physician Psychology
Perfectionism
Takes personal responsibility
Used to being in control and used to being the expert
Ego: changing habits of thought
Thinks rationally and scientifically
Fairness, justice, altruism are all highly valued
Culture
Asking for help may be sign of weakness
Emotional distress can be viewed as weakness
Self-sacrifice is the standard
Physician naivete
Little teaching or discussion
No visible role models
Expect law to work like medicine
No understanding of strategy or skills
Blind to deliberate emotional manipulation
Takes the process personally
System Design
Plaintiff's attorneys are well versed in physician psychology and their job is to win
Judge and jury have no medical expertise
Physician weaknesses exploited systematically
Leverage guilt, emotion and naivete
Experts: no standards, no consequences
Litigation Stress
Stress incurred by physicians after involvement in a malpractice suit
Common themes and reactions:
Fear of repercussion/judgment
Shame
Imposter syndrome
Anger at unfairness, experts, lack of control
Guilt and self-accusation
Obsessive recounting of events
Disillusionment with medicine
Actions to take if served:
Do not tell anyone but your attorney the details of the case
Possibly spouse, peer review, “hypothetical” cases
Do tell supportive friends and family that you have been named and how you are coping
Do seek out colleagues or other physicians who have been through the process
Do get a book or visit professional society resources
Adverse events, stress and litigation (Sara Charles MD)
When good doctors get sued (Angela Dodge PhD)
How to survive a medical malpractice lawsuit (Ilene Brenner MD)
Malpractice Stress Syndrome
Continuum with litigation stress syndrome
Increased physical symptoms
Severe depressive or anxiety symptoms
Inability to perform duties at work
Substance abuse
Suicidality
Litigation is a long process, and must be viewed as chronic stress with acute exacerbations
We should provide ongoing support for colleagues who may be experiencing litigation
Process should not be hidden
Seek support – process should not be ventured in isolation
“The science… tells us that stress is most likely to be harmful when three things are true:
You feel inadequate to it
It isolates you from others
It feels utterly meaningless and against your will”
What can we do: talk, learn, find help, reframe, give help
Trial vs. Settlement WITH dr. Gita Pensa
Wong KE, Parikh PD, Miller KC, Zonfrillo MR. Emergency Department and Urgent Care Medical Malpractice Claims 2001-15. West J Emerg Med. 2021;22(2):333-338. Published 2021 Feb 15. doi:10.5811/westjem.2020.9.48845
15 years, 6779 claims
65.9% dropped, withdrawn or dismissed
22.8% settled
Average settlement $297,709
7.6% went to trial - defendants prevailed 92.6% of the time
“True malpractice is settled”
Most cases don’t actually involve malpractice
Most cases that go to trial are defensible
Criminal vs. Civil Litigation
Anyone can file a lawsuit in civil court
Burden of proof is different
Civil = preponderance of the evidence
Criminal = beyond a reasonable doubt (higher bar)
What's at stake:
Civil = money
Criminal = jail, probation, fines, community service
Considering settlement offers
Speed
Can spare you months to years of preparing for trial
Certainty
If case goes to trial, cases are decided by judges/juries without medical expertise
Disadvantages:
Physician
Reported to the NPDB
Licensure and privileges disclosures
Feels like admission of wrongdoing
Insurer pays money
Plaintiff loses a chance for a big trial payout
Insurer Perspective
Wants to support the doctor
They are a business = responsibility to make smart financial decisions
Trial is expensive
Attorney and expert billable hours
Would a settlement make more sense and be cheaper?
How likely is a large judgment against them at trial
What other losses have we had recently?
“Don’t feed the bears”
Can’t settle everything
Physician Perspective
Emotional stance
Justice vs. anxiety
Plaintiff’s Attorney Perspective
Settlements are bread and butter
Trial is expensive and stressful
How likely is a windfall?
Settlements can occur at any time, including during trial at any point prior to verdict
True malpractice is settled
However, settling does not always mean malpractice occurred (just the best decision among bad choices)
“Consent to settle” and “hammer” clauses
Consent to settle clause = doctor has the ability to decide whether or not a case can be settled
Hammer clause = if you decide to forego settlement and take the case to trial and lose, you are responsible for verdict in excess of settlement offer
Preparing for trial
Once a trial date is set, talk to your attorney about a prep plan
Trial dates are subject to change
Attorney will instruct you
Know the sequence of events
Jury selection and ‘voir dire’ (examining the jurors)
Opening statements
Plaintiff puts on case first, then rests
Defense puts on case, rests
Closing statements
Judge “charges the jury”
Deliberation and verdict
Know your deposition testimony
Know your role
Testifying is different from deposition
Talk more
Explain more fully
Educate the jury
You are supposed to be a ‘fact’ witness
Within that context, teach the medicine
Connect with the jury
Demeanor matters
Skill set and mind set
Learn to hold composure no matter what
Be attentive to word choice and tone
Be mindful of body language, positioning or any nervous habits
Be knowledgeable, but not egotistical or arrogant
Learn about common questioning traps and how to avoid them
Know the rough spots and how you will handle them
Learn to evade being pigeonholed
Take home points:
Connect with the jury on a human level
Let your concern and care for patient and shine through
Educate the jury and make them understand your side of events
Stay calm and composed, no matter what
The jury should come away wishing you were their doctor
The outcome does not rely on you alone
Judge decisions and attorney performance
Where the case is tried
Performance of experts
Co-defendants
Makeup of jury
Plaintiff optics
Control the things you can
Skill set
Mindset
Prioritizing your own health
Air care Grand rounds WITH drs. winslow and goff
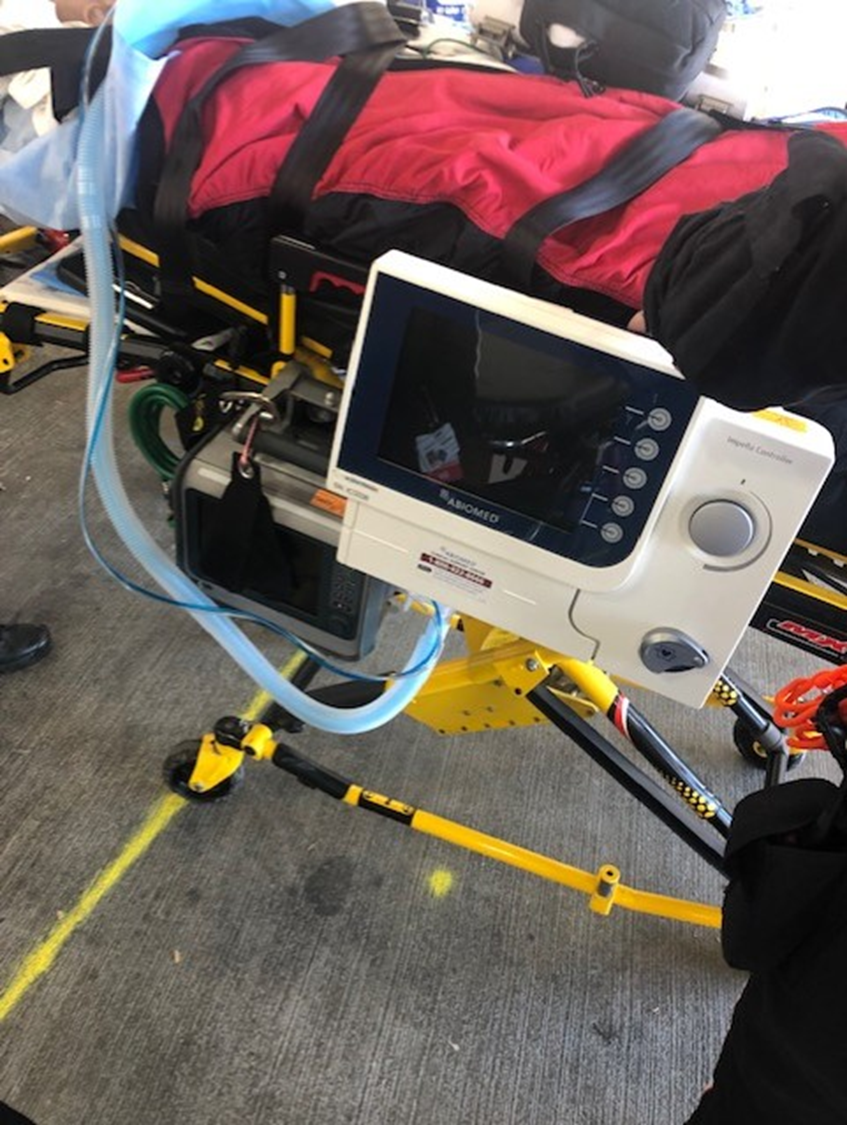
Impella and Transfer Training - Dr. Saad Ahmad
Cardiogenic shock is a spectrum and subtle signs (rising Cr, poor extremity perfusion, rising transaminases) must be appreciated and may be present without hypotension
Approach at the bedside
Pulse pressure (SBP-DBP) < 25% of SBP indicates low cardiac output
Echo (contractility, PA pressure, valve assessment, dynamic obstruction, device depth, effusion)
EKG
Impress Trial - 2016 RCT comparing IABP and impella on 6-month mortality
No difference
Small sample sizes
Sick population (mean pH 7.15, lactate 8, post-arrest patients with cardiogenic shock)
RV support
TandemHeart with dual lumen cannula
Impella RP
Femoral access
LV support
IABP
Impella
Typically femoral access, sometimes axillary
Tandem Heart
Femoral artery and femoral vein access
Inflow cannula in LA (venous percutaneous access through ASD), blood returned into aorta
ECMO
Impella Configurations
Impella RP for right sided support
Impella CP for left sided support
Impella 5.5 - axillary cutdown for left sided support
Bipella - Impella CP or 5.5 + RP
Ecpella - ECMO + impella for LV unloading
Things I need to know when picking up an impella patient on Air Care:
Clinical indication
Hemodynamics before and after support device
Access (number of sticks) - ask if access was easy
Groin appearance
Sheath depth
Sheath (peel away or repositioning sheath)?
Is the sheath secured?
Tuohy Borst Valve secured? (White twistable valve proximal to the blue T piece that is sutured to skin - will prevent catheter from slipping within sheath)
If not secured, impella will move
Distal pulses (pre and post impella)
Anticoagulation: ACT, infusion
Cangrelor much more potent platelet inhibitor than Brilinta
Urine color
Patient considerations:
With femoral access, do no raise head of bed higher than 30 degrees
Use knee immobilizer
Assess access site for bleeding and hematoma
After confirming security of access site, position impella plug to allow easy access during transport in the event of a “air in purge” alarm
Be careful not to pull on the impella catheter when transferring a patient from one bed to another
Monitor distal pulses
Do not use alcohol products on any part of impella products
Make sure fluids are hanging higher than the purge cassette
If you must perform CPR, turn the impella down to P-2
If you need to defib, do not change impella settings
If you get an “impella stop” alarm, it is not functioning and you may need to start inotropes
Waveforms:
Placement signal = similar to art line waveform (similar pressure)
LV pressure is estimated, pay attention to EDP
Motor current (difference between inlet and outlet), must be pulsatile
Flow displayed in bottom left
Top and bottom numbers (systolic and diastolic flows) should be at least 1L apart
Purge system (flow and pressures) next to the impella flow numbers
Cardiac output and power output numbers next to purge system numbers
Alarms:
Suction:
Reduce P level
Decrease until suction alarm breaks
Filling level and volume status
Can see negative diastolic pressure on LV pressure reading
Verify impella position
ECMO Logistics
Expect increasing volumes of ECMO transports in the coming years either by Air or Ground with UC and The Christ as receiving; also long distance transports out of Cincy to other centers for transplant (Cleveland, Detroit, etc)
Crew configuration based upon receiving - ECMO nurse specialist + flight crew if going to Christ; perfusion + CCAT + flight crew if UC
Eyes on and dedicated handler for ECMO cannulas during any patient movement.
Consider the myriad logistics of the transport including multiple infusions (analgosedation, paralysis, heparin, vasopressors, blood products, antibiotics), ventilator, chest tubes, ECMO cannulas, CVC, PA catheters, A line, Foley - organize perhaps with the lasagna technique of layering devices with blankets
Consider VV vs VA indications and rescue enroute should mechanical support fail.
VV - likely on lung rest settings on ventilator and may need to titrate settings; may need to initiate Veletri
VA - consider inotropes, vasopressors, preload versus afterload reduction
ECMO mounting equipment - all front-line AC stretchers with ECMO bracket to accommodate ECMO shelf. Review images below for anticipated gurney configuration and loading with ECMO moved to floor plate for flight.