Grand Rounds Recap 11.2.16
/CPC with Drs Sabedra and Toth
The case - an elderly female presents via EMS with vomiting, diarrhea, and a fall
HPI: Got up quickly to go to the bathroom, fell and couldn’t get up. She’s had diarrhea for several days. Last seen normal at 9:30 last night, called out for help to family around 4:30am. Right side of her body feels “quiet”. No pain, but can not walk.
PMH: Hypertension, hyperlipidemia, possible stroke and PRES in 2011
Social Hx: Tobacco use
Meds: aspirin, hydrocholorothiazide, levetiracetam, losartan, metoprolol, pravastatin
VS BP 198/82 HR 90 T 98.1 F SpO2 99% on room air
Exam; 4/5 strength LLE, 3/5 strength RLE, upper extremity strength is intact bilaterally. Decreased sensation to light and sharp touch throughout R leg. Toes down going bilaterally.
Labs:
- Cr 1.0; BUN 32; +Anion gap 21
- Lactate 6 -> 2.6 after fluids
- Trop 0.05 -> 1.08
CXR, pelvis x-ray, femur x-ray, and CT head all normal. MRI brain -> new, small left occipital infarct, otherwise normal. EKG with a fib rate in 90s
A diagnostic test was ordered....
Ddx:
- GBS
- AIDP
- Transverse Myelitis
- B12 deficiency
- Dissection (vertebral vs aortic)
- Vasculitis
- Embolic disease
Test of choice by Dr. Toth: MRI axial skeleton to evaluate for spinal stroke
Test ordered by team: CT abdomen/pelvis: demonstrated large clot at the aortic bifurcation
Peripheral arterial disease (PAD)
Specifically in this patient: Aortoiliac occlusive disease
Symptoms include: hip, buttock and thigh claudication; decreased pulses; bruit over renal arteries, lower extremity muscle atrophy, slow wound healing
According to ACC/AHA 2013 guidelines:
Risk factors for PAD include increasing age, male gender, African-American race, hypertension and hyperlipidemia
Critical limb ischemia is denoted from PAD by presence of pain at rest and tissue loss or destruction. Acute limb ischemia is most likely due to thromboembolism, with dissection another consideration. The American College of Chest Physicians recommends immediate weight-based IV heparin bolus and drip for anyone with critical limb ischemia.
Limb ischemia from PAD is generally stratified into:
- Viable - no immediate threat of tissue loss
- Threatened - salvageable with prompt/urgent revascularization
- Nonviable - major tissue loss with nerve damage
A word about Ankle Brachial Indices (ABI):
Sn >90% Sp >95% in diagnosing >/= 50% stenosis of lower extremity arteries.
CTA has generally been found to have equal sensitivity and possibly better specificity than MRA or doppler.
Our patient ended up needing a pacemaker placed for uncontrolled/unstable a-fib; she went into rhabdo with AKI secondary to ischemia of the bilateral lower extremities, got a R knee amputation, needed CRRT, underwent exploratory laparotomy for bowel ischemia, and was ultimately passed away
Viral Hepatitis with Dr. Habib
Take a minute to review Dr. Habib's Primer Post
Case 1: Young male with history of IVDU and chronic low back pain presents with 1 week of progressively worsening nausea, vomiting, generalized malaise. Exam notable for scleral icterus and mild RUQ/epigastric tenderness without rebound.
VS: T100.1 HR 104 BP 132/84 RR 18 SpO2 97%RA
Labs:
- BMP - unremarkable
- CBC - WBC 3.2; Hgb 12.4; Plt 190
- LFT - AST 740; ALT 825; Dbili and Tbili elevated
- Lipase - normal
Q1) What factors might lead you to send hepatitis serology on this patient?
CDC Recommendations: consider hepatitis testing in all patients from endemic areas. Only the US, Canada, Western Europe, Australia, Chile and Argentina are regarded as NOT endemic areas. Patient from any other country can be considered from an endemic area. They also recommend testing anyone with personal risk factors for hepatitis including (though not limited to):
- IVDU
- Men who have sex with men
- Pts on immunosuppressive tx
- Elevated AST/ALT of unknown etiology
- Household or sexual contacts known to be HBV+
- HIV patients
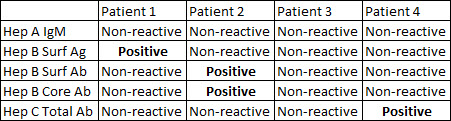
Q2) You decide to send hepatitis exposure panel. Results from 4 possible patients are given below. What is your interpretation of each?
- Patient 1: Infected with HBV, but yet unclear if this is acute or chronic. Will require repeat testing in 3 months to further delineate.
- Patient 2: This patient is immune. Core antibody indicates a prior infection.
- Patient 3: This patient is susceptible. They either are not infected or have a very early infection.
- Patient 4: This patient has 4 possibilities -
- Resolved past infection
- Resolving acute infection (window period)
- Low level chronic infection
- False + anti core Ab (unlikely)
To review HBV serology:
- HbsAg - a marker of infectivity (+ = infection)
- Anti HBsAb - immune to HBV
- Anti HBc IgM - early infection
- Anti HBc IgG - late infection (must order total core and core IgM and then subtract to obtain IgG)
- HBeAg - Indicative of high replication (more important for our GI colleagues)
- Anti HBe - marker of low replication
Case 2: Inspired by recent data that suggests hepatitis C is highly prevalent in ED patients, you consider offering screening to patients in your pod. Would current guidelines support testing in the following patients?
CDC/USPSTF recommendations for HCV screening:
Screening is based on age and personal risk factors. If born between 1945-1965, patients should have 1 lifetime screening. Patients who are IVDU, HIV+, with transaminitis of unknown origin, on hemodialysis, received clotting factor concentrate prior to 1987, received blood transfusion prior to 1992 should be screened.
- 24yoF, G3P2 @16wks, here for intractable vomiting - CDC says doesn't need screening, ACOG says does need screening. Reasonable to screen if they have not been already
- 19yoM, received narcan for heroin overdose - no official recommendation to screen, but may be worth offering
- 43yoM, hx of crack cocaine abuse, c/o chest pain - may depend on method of crack use (injection), but does not necessarily need to be screened
- 32yoF works as scrub nurse in OR, c/o syncope - no recommendation to screen health care providers.
- 42yoM admitted for asymptomatic dialysis - yes, CDC recommendation interval screening, though specific interval less well defined
- 22yoF c/o vaginal discharge, reports 7 sexual partners in the last year - recommendations are to screen, however this scenario is not given as strong a recommendation as HIV/IVDU patients
- 68yo M, c/o rectal bleeding - yes he should be screened, given his age
- 40yoM HIV+, on ARV c/o fever and cough - yes he should be screened
- 38yoM c/o Sickle Cell pain crisis - may warrant screening, if hx of blood transfusions prior to 1992
Case Follow-Up: Master's Class With Dr. Powell
Case 1 - Middle aged male c/o 1 day left lower abdominal pain, worse with movement, and when riding in the car. No n/v/d, no pelvic or urinary complaints.
PMH: diverticulosis & HTN taking lisinopril and metformin
VSAfebrile HR 106 BP 146/92 98%RA
She ambulated to the room. Clear lungs, heart is regular without murmurs. She has some mild LLQ tenderness on abdominal palpation, no CVA tenderness, rebound, or guarding.
Labs - normal including WBC and urine. CT a/p with diverticulosis but no evidence of diverticulitis.
Dispo - home on cipro/flagyl, and strict return precautions.
Case 2 - Another middle aged male with L hip pain. Worsening over 2 days. No prior ED visits, has been taking ibuprofen with some relief. Denies trauma.
PMH: HTN, HLD, NIDDM, he is on a stating, amlodipine and metformin
VS: Afebrile HR 92 BP 136/98 97%RA
He ambulated to the room. Clear lungs, heart is regular without murmurs. L hip is mildly tender to palpation, but full ROM, sensation intact. No warmth or overlying skin changes. Lower leg is normal.
Hip X-ray is normal. CT non-con of the hip shows only mild OA with mild joint effusion.
Labs - Unremarkable except for mild CRP elevation to 19.
Dispo - home on with PO pain control, ortho f/u in 3 days.
Case 1 Return Visit - 4 days after initial visit. Persistent LLQ pain despite antibiotics. Can not ambulate pain is so bad. No other new symptoms.
Exam: L groin and hip tenderness to palpation, without significant abdominal tenderness. pain with internal and external rotation at the hip, but not knee. No overlying skin changes. Pulse and sensation intact.
Labs - WBC 14; ESR/CRP 30/100
Patient admitted, MRI concerning for infectious process in joint, tap by orthopedics grows out Group A Strep (GAS). Patient got PICC for IV antibiotics, and is doing well.
Case 2 Return Visit - 4 days after initial visit, patient returns in a wheelchair unable to bear weight on his L hip. Now with low grade temps. Had seen ortho who ordered some labs, they called him today and said his labs were "abnormal" and to go to ED.
Exam: T 100.1 HR 106 BP 154/88 97%RA
No external changes to hip, but now with significant discomfort with ROM.
Labs - CRP 342; ESR 36; WBC 11
Patient admitted, MRI concerning for infectious process in joint, tap by orthopedics grows out Group A Strep (GAS). Patient got PICC for IV antibiotics, and is doing well.
Lessons from these cases:
- Consider non-abdominal causes of "abdominal pain," especially the hip!
- Septic arthritis most commonly affects
- Knee (50% cases)
- Hip (2nd most common site)
- Shoulder
- Elbow
- There is NO absolute synovial WBC cut off to diagnose septic arthritis (though sources will quote 50,000-150,000 cells/mm3)
- One study quoted a mean CRP in patients with septic joint diagnosis at 13 (compared to 6 in normal patients) and a mean ESR in septic joint patients as 57 (compared to 43 in normal patients.
Legally Defensible Documentation: Tips to Improve Patient Safety with Dr. Mike Weinstock
Q1: Why do we document?
Three reasons:
- Inform future providers (ED providers at handoff, hospitalists, future ED providers)
- Billing
- Legal protection (according to NEJM 2006;354:2024, 7.8% of ED providers are sued per year, and the average time to resolution of a case is 5 years)
Q2: What is required to lose a lawsuit?
It must be proven that:
- Physician had a duty
- Physician has breached that duty (by deviating from standard of care of like-minded providers)
- There was harm
- The harm was caused by breach of duty
Q3: What is the deal with the MDM section?
Your MDM should reflect your decision making. It should not be redundant with the rest of the chart. It should record a differential diagnosis, as well as pros and cons for diagnoses considered. It should also be used as a mental "hard stop" for you to reflect on the progression/logic of the case and whether it makes sense.
Dr. Weinstock's final recommendations for legally protective charting
- Address the nursing chief complaint in your note, especially if it differs from the history you gather!
- Document a good neuro exam (especially for any HA, dizziness, weakness, LOC, incontinence, or numbness chief complaint)!
- Be descriptive in your encounter (ex. "the patient exhibited facial wincing with chest palpated" is better than "reproducible chest pain," and "soft/nontender" is not an acceptable abdominal exam!
- Perform repeat exams (especially abdominal) and document them in your MDM!
- Document a plan if the patient condition changes (remember the 3 "R's": revisit your patient, record the revisit in your MDM, and recruit follow up help for your patient)!
- For AMA documentation, you must document patient is of sound mind and body and has capacity to make decisions
- Ultimately, do not practice defensive medicine, but document in a way that is defensible