Grand Rounds Recap 12.6.17
/AIRWAY GRAND ROUNDS with Dr. Carleton
Case 1: Middle aged male with Down Syndrome with morbid obesity comes in with labored breathing, accessory respiratory muscle use and retractions. Hypoxia on a NRB @ 15/L
Exam: Faint wheezing, drowsy
Labs: Respiratory acidosis with contraction acidosis
Treatments: bronchodilators, steroids, Mag, antibiotics and Lasix
Respiratory acidosis continues to worsen despite initiating bipap
Plan: DSI/Awake look using ketamine, oral endoscopic intubation through Williams airway, called ENT and surgery as back up for predicted surgical cricothyrotomy
Attempt 1: Oral endoscopy fails secondary to copious secretions
Patient re-oxygenated with bipap
Attempt 2: RSI with succinylcholine and ketamine with difficult airway blade, success
Case 2: Your female presents with AMS and SOB. Lethargic but easily aroused with respiratory distress
PMHx: MRDD, morbid obesity, asthma, hypertension, DM, arginosuccinate lyase deficiency
Labs: significant respiratory acidosis, leukocytosis, NSTEMI, AKI, BNP elevation
Attempt 1: awake technique using difficult airway blade, topically anesthetize with lidocaine, sedate with ketamine
Attempt 2: oral with a Williams airway, too many secretions
Attempt 3: re-dosed ketamine, too many secretions and redundant tissue
Attempt 4-6: attempt nasal endoscopy using viscous lidocaine and Afrin, too many secretions and redundant tissue
Eventually intubated with VL after decompensating
How to intubate during an awake look?
Difficulty indicators for VL: mouth opening
Difficulty indicators for endoscopy: secretions and operator inexperience
How do you handle secretions?
Suction ports with large disposable scopes
Be sure to take off blue end of suction tubing prior to attaching it to scope to minimize air leak
If you put the adapter on scope in order to inject through the scope this will diminish your ability to to use the suction
Use Jankauers to assist, don't rely on the suction canister
Glycopyrrolate: no central effects, less tachycardia than atropine, dose 0.2-0.4 mg IVP, onset 1-2 minutes with peak at 1 hour, however good enough effect in 10-20 minutes
Utilize simple physical measures to combat redundant tissue (jaw thrust and neck extension)
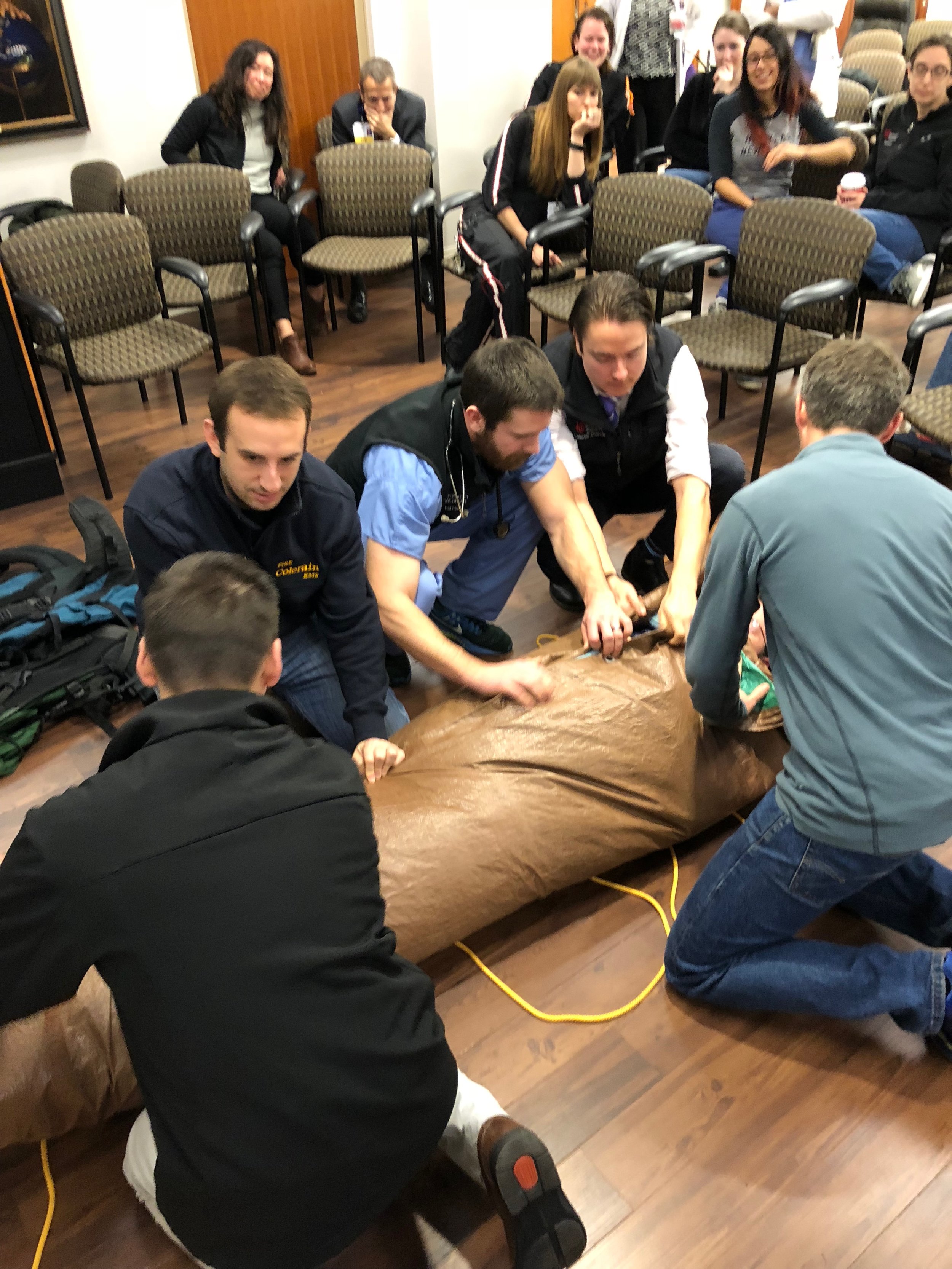
WILDERNESS MEDICINE: Extrications and botany with Drs. Roche & Plash
Extrications
Scenario 1: Back country skier falls into cold running water. Able to get out of water but need to extricate and warm simultaneously
Place a vapor barrier first (tarp) and then a conduction barrier to prevent heat loss to the floor and then use sleeping bags etc to create a "burrito”
Consider covering/protecting head both for trauma during extrication and heat loss, eye protection and access to groin for excrement
Scenario 2: Fall off cliff with debilitating lower leg injury
Carrying patient a long distance to an extraction point on a litter is difficult, expect needing 8-10 people for a one mile trek
You can consider strapping together two backpacks together to create a "backboard" and supplement that with a rope litter
Can use the backack hip belt for C-spine immobilization
Botany/Toxicology
Rosary pea and castor beans
Similar toxin (abrin for rosary pea and ricin for castor bean)
- Inactivate ribosomes, decreasing protein synthesis
- Non-toxic unless crushed when ingested
- Also have toxicity when inhaled or with skin exposure
- Ingestion- Present with bloody emesis, progressing to hepatic and renal failure
- Inhalation- diffuse pulmonary edema leading to respiratory failure
- Exposure- conjunctivitis, retinal hemorrhage, dermatitis, and systemic symptoms
- Treatment is supportive care and decontamination
Wolfsbane
- Aconitine is active toxin - sodium channel activator
- Present with paresthesias, weakness, atrial and ventricular arrhythmias, lacrimation, diaphoresis, vomiting, and diarrhea
- Treatments not well studied, but some data for benefit of lidocaine and tetrodotoxin (sodium channel blockers)
Gyromitra (false morel)
- Gyromitrin is toxin (hydrolyzed into monomethylhydrazine)
- Inactivates pyridoxine (B6), leading to decreased GABA activity
- Present with seizures, fasciculations, and nystagmus
- Can also cause methemoglobinemia
- Metabolite causes direct liver necrosis
- Pyridoxine is treatment of choice, reversed neurologic symptoms
Amanita phalloides (death cap)
- Amatoxin is primary toxin (RNA polymerase inhibitor)
- Leads to decreased protein production and cell lysis
- Heat stable protein, not broken down via cooking
- Initial symptoms include nausea and watery diarrhea
- Resolves in 12-24 hours
- Develop fulminant liver failure with symptoms starting in 48-72 hours
- Treatments include n-acetyl cysteine, silibinin (from milk thistle), penicillin G, and cephalosporins
Oleander and foxglove
- Active toxins are cardiac glycosides (oleandrin in oleander and digitalis in foxglove)
- Present with symptoms of Digoxin toxicity
- Atrial and ventricular arrhythmias, xanthopsia, vomiting, diarrhea
- Digibind is effective for both for severe toxicity
Jimsonweed
- Contain atropine, scopolamine, and hyoscyamine
- Present with anticholinergic toxidrome
- Benzodiazepines recommended for agitation
- Physostigmine is controversial but reverses toxidrome
Pokeweed
- Contain oxalic acid, saponins, and alkaloids
- Most symptoms localized to GI tract apart from ingestions by small children
- Present with vomiting and bloody diarrhea
- Can have respiratory failure and anemia if systemic symptoms present
- Treatment is supportive
Strychnine tree
- Strychnine is primary toxin (glycine and acetylcholine antagonist)
- Present with seizures, muscle contractions (including opisthotonus) and respiratory distress
- Treatment centers around benzodiazepines and phenobarbital for seizures
- Dantrolene controversial for muscle contractions
- Often require intubation, continuous EEG
R1 Clinical Diagnostics: Labs in Pediatric Trauma with Dr. Modi
See Dr. Modi's primer for a warm-up
Blunt cardiac trauma
1. EKG: recommended if there is any hemodyanmic instability
- Studies showed that in pediatric patients with hemodynamic instability and EKG may be helpful
- 82% of patients received an EKG based on external trauma or notability and 57% of those EKGs showed abnormalities
- Arrhythmias such as sinus tach, ST-T wave changes, new BBB, SVT, ventricular arrhythmia, electrical alternates should prompt a bedside echo
2. Troponin: unclear evidence on use in children, not reccomended
Blunt abdominal trauma
1. CBC: recommended
- Hematocrit <30 can indicate massive hemorrhage even when FAST is negative
- Less intra-abdominal muscle means pediatric patients are prone to more solid organ injury than adults
2. LFTs: recommended
- Highly specific test to rule in intra-abdominal injury, lacks sensitivity
- One study with 1095 patients showed that AST >200 and ALT > 125 had a specificity of 96% for intra-abdominal injury
3. Amylase/Lipase: not recommended as not reliable to predict pancreatic injury
4. UA: recommended
- Gross hematuria or UA >50 cells/HPF field should prompt cross sectional imaging to assess for GU injury
Quick and Dirty Pediatric Vitals
Pulse
- Infant: 160
- Preschool: 120
- Adolescent: 100
SBP
- Infant: 80
- Preschool: 90
- Adolescent: 100
- OR SBP = 70 + (2 x age)
RR
- Infant: 40
- preschool: 30
- Adolescent: 20
R2 CPC with Dr. Murphy-Crews & Dr. Bryant
The Case
3 day old with difficulty breathing, grunting noises, and increasing pauses in respirations. Progressively worsening and unrelated to feeds. No fever, born at 41w 4d via C section for failure to progress, good Apgars, GBS negative. Breast fed exclusively with excellent prenatal care
Exam: RR 68, diminished tone with grunting, no dysmorphic features, clear lungs, cap refill < 2 seconds
Labs: BMP, CBC, LFT, Ammonia = normal, VBG with pH 7.33 & PCO2 54
LP with 3500 RBCs (potentially traumatic), 4 WBC, Glucose 66 and Protein 118
Brain US WNL
While in ED has increasing apnea spells with worsening respiratory acidosis requiring intubation
Subsequently develops myoclonic jerks
CT head WNL, cEEG shows burst suppression
Diagnostic test is ordered
Discussion:
T: Trauma, tumor, thermal
H: Heart disease, hypovolemia, hypoxia
E: Endocrine (CAH, DM, thyroid)
M: Metabolic disturbances (electrolyte imbalance)
I: Inborn errors of metabolism
S: Seizures or CNS abnormalities
F: Formula dilution or over-concentration leading to hypo/hypernatremia
I: Intestinal catastrophe (intussusception, volvulus, NEC)
T: Toxins (including home remedies such as baking soda for burping)
S: Sepsis
Consider ammonia, calcium, glucose and ketones when thinking about inborn errors of metabolism
Ddx: Rare metabolic error, seizure disorder, neonatal stroke, meningoencephalitis, or hypoxia ischemic encephalopathy
Diagnostic test of choice: CSF:Serum Amino Acid Ratio
Diagnosis:
Non-ketotic hyperglycinemia (glycine encephalopathy) diagnosed by CSF:Serum amino acid ratio (Dr. Bryant for the win)
Defects in glycine metabolism causing an increase in the neurotransmitter in the CSF
Consider in the apneic, hypotonic previously healthy neonate with burst suppression
1 in 60,000 babies with an autosomal recessive inheritance pattern
Onset of encephalopathy in hours to days so usually newborn screen results after onset of symptoms
Treatment is supportive for seizures and possibly dextromethorphan
Valproic acid is contraindicated
Prognosis is poor
R4 Case Follow Up: Hyoid Fracture with Dr. O'Brien
Case: 50 year old male presents after assault with ecchymosis over right eye and 1.5 inch lac to the posterior scalp
CT scan shows hyoid fracture with significant hematoma
Patient develops SOB and inspiratory stridor
Bedside scope shows prolapse of soft tissue and false vocal chords obscuring view true vocal cords
ENT consulted and patient goes to OR emergently for an awake tracheostomy
Hyoid Bone Fractures
Mechanisms of injury: most often direct blow to the nick while it is hyperextended or strangulation
Signs and Symptoms: neck pain, hoarseness, dyspnea, dysphagia, ecchymosis/edema, crepitus, stridor
Management: CT of the neck with IV contrast or direct visualization with fiberoptic scope if unstable
Consider CTA as patients can have carotid artery injuries and pseudoaneurysms
If asymptomatic patient's require monitoring for at least 24-72 hour. Stridor and airway compromise can be delayed but can develop very quickly as was seen in this patient
Managing Stress and Building Resilience with Sian Cotton, PhD
50% of physicians experience burnout but this is up to 60% of Emergency Medicine physicians
"Burnout is a response to chronic stressors that wear on a person over time — not acute ones such a big event or a big change"
- Emotional exhaustion (nothing left to give)
- Depersonalization
- Low sense of personal accomplishment
Burnout leads to decreased satisfaction, increased healthcare cost, decreased productivity, decreased patient satisfaction, broken relationships, alcohol/substance abuse, depression and alcoholism
Particularly difficult for the EM physicians since after a stressful event we often don't have the opportunity to return to baseline. This leads to increasing amounts of cortisol throughout the day which can have an additiive effect
Mindfulness: the awareness that emerges through paying attention in a particular way on purpose in the. present moment and not judgementmentally to the unfolding of experience moment to moment
This has been proven to reduce burnout and increase empathy
R1 Clinical Knowledge: Kawasaki's disease with dr. li
Unknown etiology of the disease
What if we miss it?
- 25% of untreated children develop a coronary artery lesion
- 3-5% rate in treated children, ranges from mild dilatation to giant aneurysms
- This can lead to endothelial dysfunction and accelerated atherosclerosis later in life
Diagnosis: Fever for 5 days or more + at least four out of the five following findings
- Bilateral, nonexudative bulbar conjunctival injection (perilimbic sparing)
- Oropharyngeal mucous membrane changes
- Cervical lymphadenopathy (at least one node >1.5cm)
- Peripheral extremity changes (erythema and swelling of the hands and feet during the acute phase or periungal desquamation during the convalescent phase)
- Polymorphous generalize rash (non-vesicular and nonbullous)
What if the patient has fever for more than 5 days but only 2 or 3 criteria?
If you have a CRP > 3 and/or ESR >40 look for three or more supplemental laboratory findings
- Anemia for age
- Albumin <3
- Plateles >450,000
- WBC >15,000
- ALT elevation
- Pyuria >10 WBCs
If CRP and ESR are low use serial clinical re-evaluation and echocardiogram if peeling develops
Differential Diagnosis: measles, adenovirus, enterovirus, EBV, SJS, toxim-mediated syndromes (staph scalded skin), scarlet fever, mercury posining
Management
Acute febrile phase: decrease inflammation to the myocardium and supportive care
When initiated within the first 10 days of fever treatment can decrease progression to coronary artery dilatation and aneurysm formation
All patients need admission and cardiology consults
IVIG
- 2g/kg over 10-12 hours
- Very safe treatment but is expensive
- Live vaccines should be deferred for 11 months
- If immunized <14 days prior to administration will need to be re-immunized
ASA
- High dose: 80-100 mg/kg/day orally every 6 hours until patient afebrile for 48-72 hours
- Low dose: 3-5mg/kg/day orally until lab studies become normal (usually 6-8 weeks)
Reye’s syndrome:
Risk in children receiving aspirin who have active infection with varicella or influenza or patients receiving high dose aspirin for a prolonged period of time after Kawaski
Not assocaited with low-dose aspirin administration
In patient with influenza and Kawasaki concurrently can give IVIG without aspirin and use alternative anti-pyretic (APAP) and alternative antiplatelet for at least two weeks
Has been reported in high dose proton but not low dose
Other treatment that are not standards of care but has some data: steroids, infliximab, cyclosporine A