Grand Rounds Recap 12.14.16
/Emergency KT Protocol - Alcohol Withdrawal with Drs. Whitford and Soria
Epidemiology of Alcohol Use Disorder (AUD)
- 30,722 EtOH related deaths in 2014
- DT's untreated mortality 15%; treated mortality is 5%
Diagnosis of AUD:
- CAGE: 90% sens 77% spec for AUD in patient's lifetime
- FAST-Audit: 94% sens for AUD 99% sens for patients at risk for withdrawal right now
- Physical Exam: Intention tremor is most sensitive for risk of withdrawal
- Seizures do not equal DTs and the presence of one does not predict the other
- Seizures typically present at 6-25 hrs after the last drink
- DTs typically present at 2-3 days after the last drink
Screening for withdrawal: use a scale and be consistent
- CIWA-Ar was developed in 1975 developed for research in rehab centers
- Shot Protocol
- Glasgow Modified Alcohol Withdrawal Scale (GMAWS)
Pharmacology of EtOH withdrawal:
- Benzo options: Diazepam v Lorazepam
- Diazepam PROs: Faster onset means less risk of dose stacking, longer half life means less risk of rebound withdrawal
- Diazepam CONs: Tremendously lengthened half life in end stage liver disease
- Lorazepam CONs: potential for propylene glycol toxicity (80% of drips are propylene glycol)
- Phenobarbital: In one study, a single dose of phenobarbital reduced amount of benzos and decreased intubations and PNAs in the ICU
- 10mg/kg load in a small RCT showed reduction in ICU admission
Protocol
- Mild CIWA <10: consider observing and okay to discharge if tremor gone and two CIWAs <10 2h apart
- Moderate CIWA 10-20: PO Diazepam (unless liver failure, then consider lorazepam)
- Severe CIWA >20: Diazepam IV q5-10min titrated to RASS -1 (sleepy but arousable)
- If still refractory after >300mg of diazepam consider phenobarbital IV q30min
- Initial CIWA >30: consider upfront phenobarbital load 10mg/kg over 30min
Discharge Criteria:
- Once alert, clinically sober, and medically cleared, consider discharge
- Consider gabapentin for alcohol withdrawal
- Day 1 300mg PO QID
- Day 2 & 3 300mg PO TID
- Day 4 300mg PO BID
Myths
- Fixed dose benzo regimens are not good for patients
- IV fluids do not help
- No change in BAC or time to discharge
- Blood work may not actually help your management
- The need for Thiamine is actually very rare
EM-Neurology Combined Lecture: Neuropathies with Dr. Neel
6 levels of the peripheral nervous system
- Anterior horn cell & dorsal root ganglia
- Roots
- Plexus
- Nerve
- Neuromuscular junction
- Muscle
Painless weakness: consider pathology at the level of the muscles, NMJs and anterior horn cells
Pain with weakness: consider pathology at the level of the nerve roots, plexus, and peripheral nerves
Ask about autonomic symptoms: sweating, GI (constipation, gastroparesis), CV (palpitations), sexual dysfunction, GU (hesitancy, frequency)
Types of Neuropathies
- Mononeuropathy (individual nerves)
- Polyneuropathy
- Distal symmetric polyneuropathy
- Polyradiculoneuropathy (Guillan-Barre)
- Peripheral Polyneuropathy
- Primarily motor
- Primarily sensory
- Mixed
- Large fiber (vibration, light touch) vs Small fiber (pain, temp)
- Autonomic involvement
- Distal>Proximal
- Distal=Proximal
- Distal<Proximal
- Axonal v Demylinating
Distal Symmetric Polyneuropathy:
- Multiple neuropathic symptoms are accurate than single symptoms
- Signs are more accurate than symptoms
- A single abnormality is less sensitive than multiple abnormalities
- Simple testing at bedside can be accurate for diagnosis
Examination:
- Motor
- Look for atrophy of the EDB
- Toes up, fingers spread or thumb pinky
- Check peripheral small muscles and proximal large muscles
- Deep Tendon Reflexes (use a Tromner or Queens Square reflex hammer)
- Look for achilles reflex
- Sensory (safety pin, 128 C tuning fork)
- Put your finger under the toe or finger you are testing with a tuning fork, if you can feel it then they should be able to feel it
Diagnosis:
- Motor neuropathies:
- AIDP/CIDP
- Acute motor axonal neuropathy
- MMN
- CMT
- Lead intoxication
- Porphyric Neuropathy
- Sensory Neuropathies:
- Diabetes
- Paraneoplastic
- HIV/AIDs
- B12 deficiency
- Sjogren's
- Celiac sprue
- Cisplatin, thalidomide
- Infectious Etiologies:
- HIV
- Syphilis
- Lyme
- Leprosy
- HCV/HBV
- Drugs causing peripheral neuropathy: There are many. Don't forget:
- Colchicine
- Phenytoin
- Metronidazole
- Amiodarone
- Nitrous oxide
- Levofloxacin
- Chemo drugs.
- Auto-immune:
- Connective-tissue disease associated (lupus, RA, Sjogrens)
Lab Testing for Etiology:
- CBC, ESR, Renal, LFT, Glucose, TFTs, B12, SPEP, IFE, HIV
- HbgA1C (not recommended by neurology academy as there is not a correlation, should get a glucose tolerance test as its more sensitive)
- B12 (consider MMA and homocysteine)
- MMA and Homocysteine elevated in 5-10% of low normal B12
Treatment of Neuropathy
- Therapeutic (can decide after patient gets an EMG, so likely going to happen as an outpatient)
- Demylinating: treat underlying disorder
- Axonal: typically can't treat
- Take off drugs that can cause neuropathy, treat the diabetes
- Symptomatic
- Pharmacologic (gabapentin) is used for positive symptoms (pain, tingling, burning)
- Gabapentin has to be used TID (can be titrated up to 3600mg/day before considered "failure")
- Lyrica (start with 50mg BID and titrate up)
- Amytryptiline
- Low doses (10-50mg)
- Cymbalta
- Topical
- Compounding topicals, capsaicin, lidocaine
- Others (not recommended)
- NSAIDS
- Narcotics
- Mexiitene
- Non-Pharmacologic: activate large fibers to overcome the small fibers so use compression socks or ace-wraps
- Pharmacologic (gabapentin) is used for positive symptoms (pain, tingling, burning)
EMS Grand Rounds with Drs. Brent and Curry: 2017 Southwest Ohio Protocol Update
Stroke
- Record last known normal time (LKNT)
- Scene time expected to be <10min
- Pre-notify ED about patient
- AHA/ASA recommends bypassing non-stroke centers if primary/comprehensive stroke center is <15min longer transport and LKNT <12h
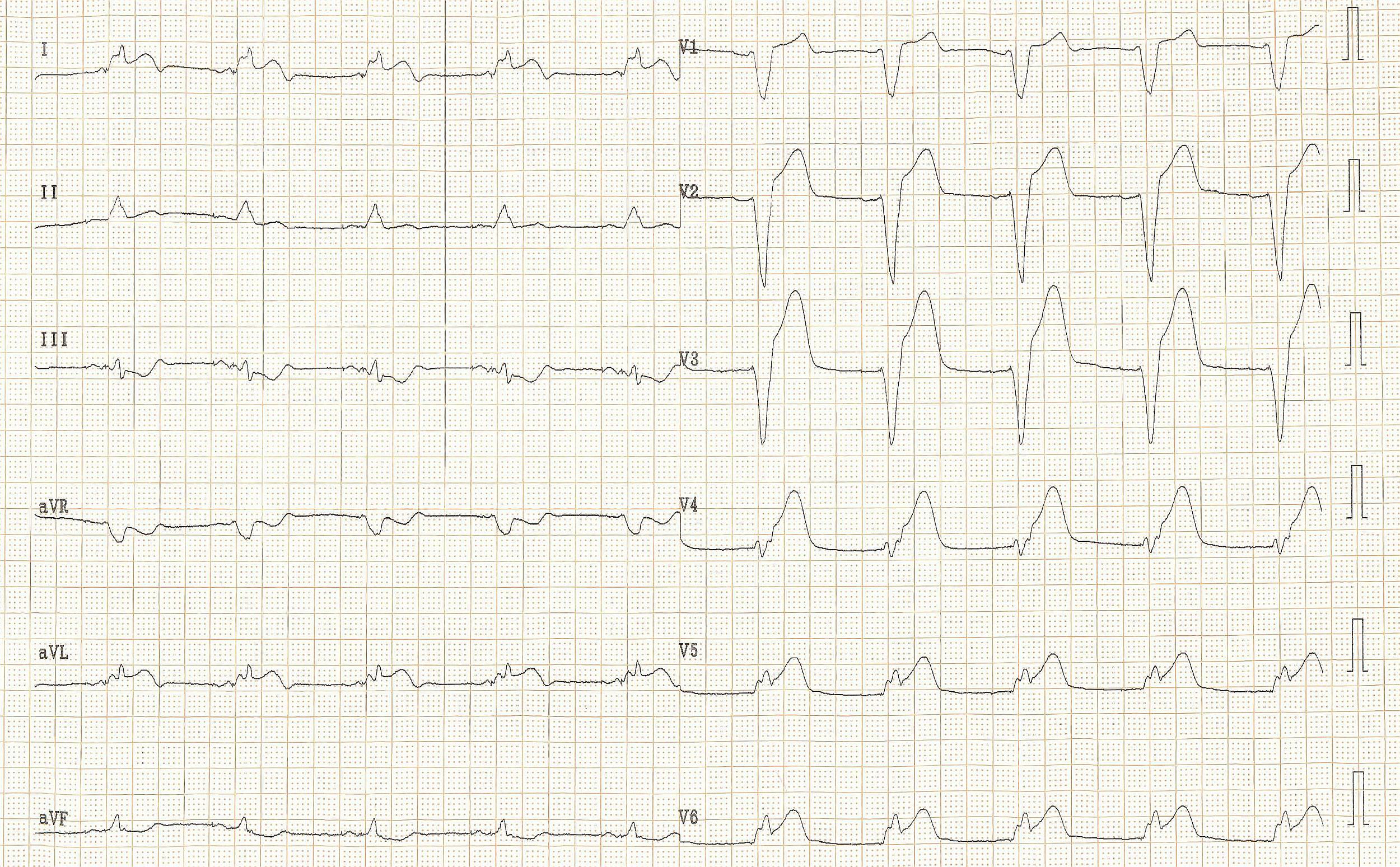
Acute Coronary Syndrome
- 12 lead EKG within 10 min
- Off scene by 15min
- Contact with STEMI alert and request cath lab
Adult Cardiac Arrest (applies to all algorithms)
- No vasopressin
Termination of Resuscitation
- Post termination body movement allowed if not a homicide and for public good
- Can terminate in the ambulance now; take body to ED as before, just let them know that CPR was stopped
Return of Spontaneous Circulation
- No more prehospital cooling after ROSC as not evidence based
- No specific end tidal CO2 goals
Overdose
- Update dose range: 0.4mg to 4mg
Adrenal Crisis: brand new protocol
- Patients/Family can self administer 100mg IM Solucortef
- Medics can given 125mg IM Solumedrol or 2mg/kg for peds
- Medics expect low sugar and low BP; think of this in cardiac arrest, N/V, hypotensive pts
Anaphylaxis
- If going to do push dose Epi then don't use IM Epi at the same time
Burns
- Cover the wound, put a blanket on the patients, start fluids, and check carbon monoxide in the field
Peds Cardiac Arrest
- Max epi dose changed to 10ml of 1:10,000 for both bradycardia and cardiac arrest
- Max atropine dose
Peds Restraint
- Restraints to be used on violent or potentially violent patients only
- Monitoring required
- Least restrictive methods to start
- Verbal de-escalation
- Physical Restraints: soft restraints
- Chemical Restraints: versed, then check BS, give O2, monitor EtCO2
- Repeat dosing requires medical control
Peds Seizure
- Versed dosing changed to weight based dosing
- Added <12kg -> 0.2 mg/kg
Determination of Death/Termination of Resuscitation
- Do not have to start ACLS on a dead person if
- Valid DNR
- Injury incompatible with life
- Signs of lividity, or rigor
- Will call for termination after:
- Airway management
- Drug administration
- 20 minutes
- No sustained ROSC (5 minutes or more)
- No spontaneous respirations, eye opening or neuro activity
- No persistent/recurrent Vfib/Vtach
- No electrical strike, hypothermia, pregnant
Imminent Delivery
- Transport mom and baby together to the same hospital
Refusal of Transport
- Can refuse transport if drinking EtOH if not clinically intoxicated
Peds Simulation with Dr. Bensman
Sim: 18 month old male in rural Malawi presents with several days of 10 episodes of diarrhea per day, decreased PO intake, and lethargic. VS HR 190 SpO2 95% 70/25 PE: awake but lethargic, sunken eyes, dry MM, cap refill slightly delayed (7 sec), hands and feet are mottled.
Access options for 18 month olds: scalp IVs, EJs, or tibial IOs
Adult IV drips: 20 drops = 1 ml
Peds IV drips: 60 drops = 1 ml
To make D5 (0.05g/ml) out of D50 (0.5g/ml) you need 50g in 1000mL so take out 100ml of NS out of the bag and then put 100ml of D50 into the bag (2 amps).
FEAST trial showed in African children with severe febrile illness and impaired perfusion, kids who got a bolus did worse than those who did not get a bolus up front. WHO is not sure how to incorporate these into guidelines, but consider going slower with these kids.
Poor man's test for malnutrition: symmetric pitting lower extremity edema or upper arm circumference of <12cm in 1-5yo
Oral Boards Case #1: 15 day old male with lethargy & poor feeding. Full-term, normal birth history. Tachycardic, tachypneic, mottled.
DDx:
- NAT
- SBI
- Cardiac (coarctation of the aorta, TAPVR)
- Pyloric stenosis
- CAH
Labs: Na 119 K 7.5 Ca 1.0
CAH: Typically presents in the first few weeks of life, will be picked up on newborn screen which comes back in 2-3 weeks. Females tend to be picked up because of ambiguous genitalia but males will appear normal so may not. Treat with hydrocortisone 100/m2 divided q6h over 24h. Keep Ddx broad and treat for SBI as well (Amp, Gent, and Acyclovir)
Oral Boards Case #2: 5 day old female with poor PO intake. VS 180 HR 56 108/70 37 87% on RA. Lethargic, mottled lower extremities, with difference in pre and post ductal sats. Diagnosis: Coarctation of the aorta above or at the level of the ductus arteriosus
Cyanotic congenital heart disease:
- Truncus Arteriosus
- Transposition of the great vessels
- Tricuspid atresia
- Tetralogy of Fallot
- Total Anomalous Pulmonary Venous Return
With concern for a ductal dependent lesion, start PGE1 before transfer to definitive care: Bolus of is PGE1 0.05mcg/kg (watch for apnea, consider intubation if transporting with non-pediatric team)