Grand Rounds Recap 5/18
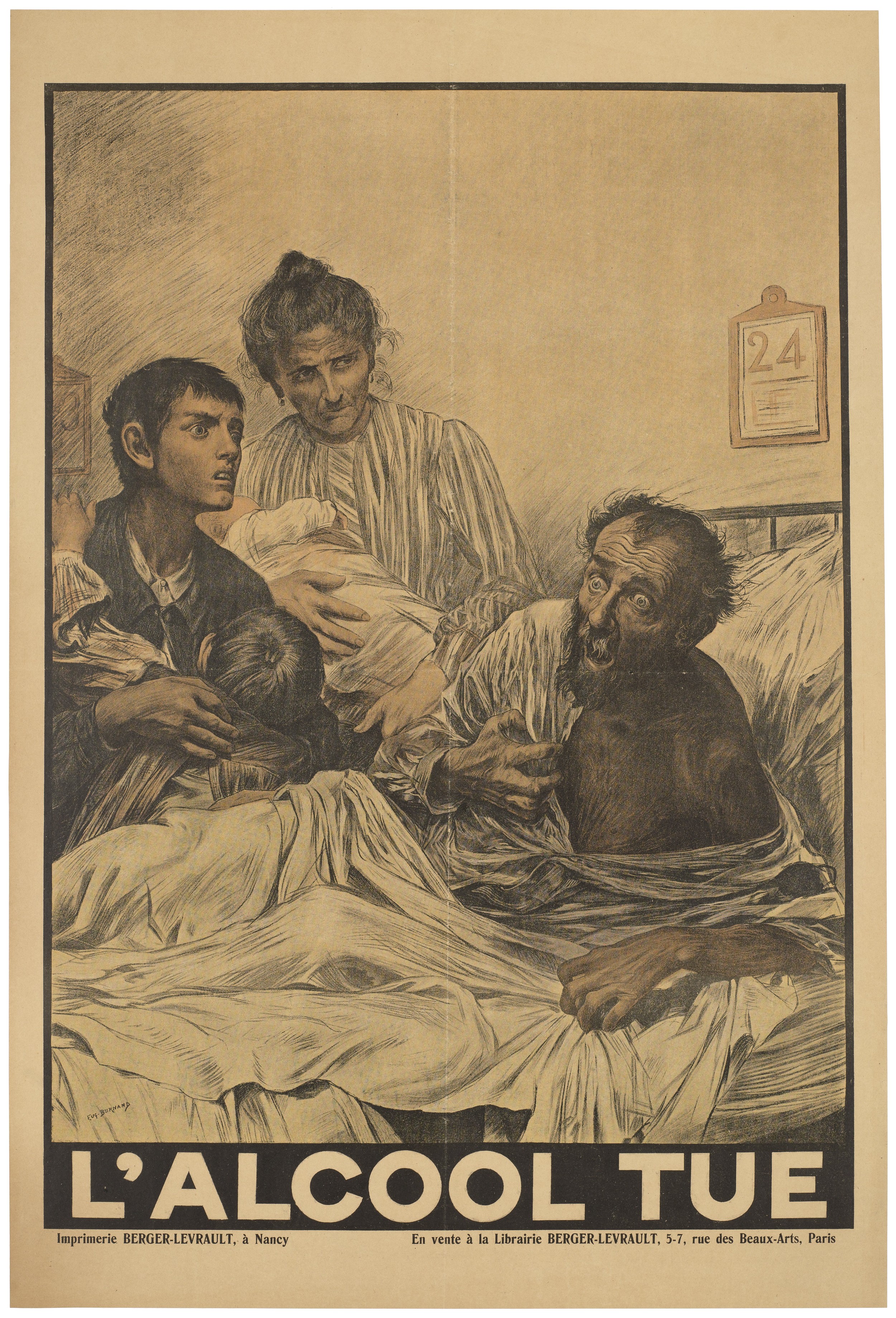
/Alcohol Emergencies with Dr. Whitford
Acute Alcohol Withdrawal Syndrome
- 8 hours after last drink symptom onset
- 72 hours symptoms peak
- 5-7 days for resolution
Withdrawal seizures occur early on (6-24 hours), tend to be self limited, and respond well to benzodiazepines. If refractory avoid phenytoin or carbamazepine as Na channel blockers are less efficacious in withdrawal seizures.
Severe alcohol withdrawal, or delirium tremens (DTs), is a medical emergency with high morbidity and mortality. These patients can die from aspiration events if their delirium is poorly controlled. Patients are most at risk for developing DTs 2-3 days into their withdrawal
How we treat patients in the ED sets the course for their withdrawal.
Diazepam IV has a faster onset of action and longer half life than lorazepam IV, making it more titratable and self tapering. This minimizes the risk of inadvertent dose stacking and over sedation, as well as protecting your patient from rebound withdrawal later on during their admission.
There is also the risk of propylene glycol toxicity in patients on prolonged high dose lorazepam infusions.
Don't be afraid of large doses of diazepam. Aggressive and rapidly up titrated doses have been shown to reduce the need for intubation, ICU LOS, and pneumonia. Doses can be given every 5 minutes with a target RASS of -1 to -2 (sleepy but arousable).
10mg --> 10mg --> 20 mg --> 20 mg --> 40 mg --> 40 mg --> 60 mg --> 60 mg
Avoid diazepam and use lorazepam in patients with advanced cirrhosis. Advanced cirrhosis will prolong diazepam's half life and contribute to benzodiazepine induced delirium well after their withdrawal delirium has resolved. Most alcoholics do not have advanced cirrhosis however have induced P450 systems.
Phenobarbital has a uniquely adept mechanism to fight withdrawal because of its NMDA antagonism in addition to the GABA agonism benzodiazepines off. An upfront 10 mg/kg load has been shown to decrease the need for ICU level of care. Use caution if a patient with other sedation as this can precipitate both hypopnea and hypotension
Here is a conceptual model of what this strategy looks like from Dr. Farkas, a pulmonary and critical care doctor practicing in Vermont. He guest posts on EMCrit.
Capstone with Dr. Niziolek - Vector-borne illness
Dengue Virus
- Leading vector-borne illness with 50 million infections per year
- Consider in any returning traveler with fever within 14 days of travel
- Associated headache, myalgias, rash are consistent amongst most vector borne illnesses
- 4 serotypes with only temporary cross immunity making multiple infections possible over a lifetime
- Diagnosis - RT-PCR, IgG or IgM, not readily available but worthy send-outs to confirm
Zika Virus
- 80% asymptomatic infection
- Symptoms of rash, fever, arthritis, conjunctivitis, and myalgias
- Also a flavivirus and difficulty to distinguish from dengue acutely
- RT-PCR most accurate within 1 week, IgG testing available but also not readily available
- Stay up to date as initial research comes out with the NEJM Zika Updates
EM-Neuro Combined Conference with Dr. Stettler: Door to needle (the process)
Door to needle time is currently 60 minutes - how can we get this time down? What about 1st medical contact to needle?
- At 2,000,000 per minute, it is not an inconsequential reduction to move to 40 minutes...
- Literature shows that we are not good with < 30% reaching our 60 minute metric
So how do we do it better?
Concurrent diagnostics (head CT), interventions (place IV) and therapetucs (mixing tPA) need to happen concurrently, however given resource limitation there must be a sequence and priority which will be inherent to your institution and practices
In our discussion, and in our Stroke Team's practice, mixing tPA, which can be initiated once your wet read does not show a contraindication to treatment. The rate limiting step should be radiology's formal read, not mixing tPA once it comes back.
Taming the SRU with Dr. Derks
In the critically in patient, when you start to fall into the weeds of your differential diagnosis, step back and think systematically. ABCs
- Regardless of the cause of acidosis, diaphragmatic function decreases. VBG is a great way to evaluate if your patient in compensating and if not readily reversible, intervene early to avoid further acidosis
- Sodium bicarbonate is just a medication and not a cure-all. It too can have deleterious effects. Be sure you want to use it. In a poorly compensated patient it will worsen your acidosis. Be cautious / avoidant of its use in DKA
- Think broadly when you see a large lactate. It is sepsis until proven overwise but metformin has been associated with lactic acidosis and nephrotoxicity and may require dialysis if refractory acidosis
Case Follow with Dr. Dang
Myesthenia Gravis (MG)
MG characterized by fatigability and muscle weakness due to antibodies directed at the acetylcholine receptor
- Symptoms can consist of ocular findings, bulbar dysfunction, and/or muscle weakness
- It is important to identify MG crisis due to the risk of respiratory failure requiring mechanical ventilation
Testing
- Ice pack test has shown to have a high sensitivity and specificity for MG (only if ptosis present), however studies limited by selection bias.
- Tensilon test (edrophonium) may be used to differentiate cholinergic crisis from MG crisis or aid in diagnosis of MG. Be aware of parasympathetic stimulation including bradycardia
- Formal diagnosis of MG can be made with serology and EMG
- ED evaluation requires a complete neurologic exam, respiratory assessment, bulbar function, and pulmonary function tests on all known MG patients
- Involve neurology early to initiate treatment and determine disposition. Any patient with tenuous respiratory status should be admitted to ICU
Airway Control
- PFTs (FVC and NIF) are important to trend, however are not predictive for need of mechanical evaluation – <20 cc/kg FVC and <30 cmH20 NIF have been correlated for respiratory failure in patients with GBS
- Values greater than 20 cc/kg FVC and 30 cmH20 NIF in MG are less likely to require mechanical ventilation, however not predictive. Hypercarbia is associated with need for intubation.
- Principals for intubation are the same, based on clinical assessment for ability to protect airway, handle secretions, bulbar function, PFTs, blood gas, and chest xray
- We should have a lower thresh hold for intubation as the MG course is unpredictable. Have caution in those whom are hypercarbic and/or have FVC <10 or NIF < 20
- When choosing a paralytic the same contraindications apply, Succinylcholine will require double the dose with longer paralysis time and half dose rocuronium is required to achieve same paralysis
- There is little high quality evidence in MG patients, but consider NIPPV in patients whom it is not contraindicated and do not have poor PFTs. Patients that were hypercarbic had higher rates of NIPPV failure.
Treatment of MG crisis
- IVIG or PLEX, high dose steroids, and immune modulating medications
- Many medications can exacerbate weakness and should be avoided in treatment of MG patients, particularly antibiotics such as aminoglycosides and flouroquinolones
SAEM Open Mic
Our residents had a great showing at SAEM 2016 in New Orleans - here are a few of the highlights
Academic Opinion on M&M Survey
- 33 programs
- 60% of residents have nevere submitted a case report
- 10% find that it is punitive
- 6% find that it identifies professional accountability
- 43% report no interaction of presented cases
Court Case Review - Resident vs Faculty
- 732 cases were reviewed from a database of ~30% of US court cases involving physicians
- $51k vs $162k per case
- Resident cases were more likely cardiac, more likely procedural
- Faculty only cases were more likely behaviorally anchored citation
Sepsis Expert Thinkspace
- EGDT is not dead, yet, but SIRS is dying and it is welcome
- qSOFA is introduced, but the jury is still out on the applicability
- Fluid status is still in flux with US, PPV and bio-impedance all still contenders
The Myth of Zero Risk
- The PanScan - does not decrease risk of mortality, ICU stay duration, and yet the argument of risk aversion seems to be winning
- Percent Risk - 20% of EM providers would only accept 0% risk in regards of chest pain, but the lowest risk population has a 0.2% miss rate, there is no such thing as zero risk