Grand Rounds Recap 9/2
/Evidence-Based Medicine: Meningitis with Drs. O'Brien and Teuber
- In one study, 95% of people with meningitis had 2 of fever, headache, meningismus but only 44% had all 3
- CT prior to LP? The American College of Radiology says do it for papilledema, altered mental status, focal neuro deficit, immunocompromised stated, history of CNS disease.
- The diagnosis and distinction of viral and bacterial meningitis via CSF studies is not always clear and there can be a lot of overlap, with a significant number of bacterial meningitis with WBC<100 and/or with monocytic predominance
- 99% probability of bacterial meningitis: WBC>2,000, Glucose<34, Blood:csf ratio<0.23, protein >220mg/dL. These are specific findings though not sensitive
- Corticosteroids for bacterial meningitis? A recent Cochrane review suggests that giving dexamethasone (adequate CNS penetration) before or with a first dose of antibiotics significantly reduces morbidity
- IDSA: Every hour of antibiotic delay in bacterial meningitis approximates 12% increase in mortality. Take home point--if giving, give early.
- One approach to antibiotics:
- Neonates (birth to 1 mo): ampicillin + cefotaxime or gentamycin
- Children 1 mo to 2 years: vancomycin + cefotaxime
- Healthy Adults 2-50 yo: vancomycin + ceftriaxone or cefotaxime
- Adults>50: vancomycin + ampicillin + ceftriaxone or cefotaxime
- Immunocompromised (HIV, active chemo, active steroid use): vancomycin + ampicillin + ceftriaxone or meropenem
- Penicillin Allergic: vancomycin, moxifloxacin +/- sulfamethoxazole/trimethoprim (listeria)
- For more info, here is a link to ACEP's clinical policy on the diagnosis and management of Meningitis
R1 Clinical Diagnostics: EKGs and STEMI with Dr. Whitford
- STEMI: STE in two contiguous leads using the TP as baseline >2.0mm
- EKGs are 70% sensitive and 85% specific for complete, acute coronary occlusion
- Serial EKGs: In patients where ACS is suspected, their importance cannot be overestimated
- New left bundle branch block: It is no longer included in the AHA guidelines as an absolute indication for cath lab activation
- Want to evaluate left bundle branch blocks for signs of ischemia? Check out LIFTL's explanation of Sgarbossa's Criteria
- aVR ST elevation + diffuse ST depression + chest pain may indicated left main coronary artery insufficiency or diffuse multi-vessel disease. aVR ST elevation, in the right clinical context, may indicate a critical left main lesion. These are not acute occlusions as acute occlusion of the left main is not compatible with life. Here is LIFTL's explanation of aVR ST elevation
- In contrast to Wellen's Syndrome, DeWinter's signify unstable LAD lesions. For more explanation and examples, check out LITFL: DeWinter's T Waves
- Wellen's Syndrome. Do not stress test these people as it may result in acute onset death. These signify subacute occlusions that likely will require a cath on a non emergent basis. This is a syndrome in the context of chest pain--they mean little if found on EKG without the right clinical context.
- Again, for examples and explanations, here's a link to LITFL's Wellen's Syndrome
- STEMI is not the only indication to go to activate the cath lab, and, as above, it is not 100% sensitive for acute coronary artery occlusion. In the right clinical context (refractory angina in an unwell appearing patient), you should be activating the lab in the absence of a STEMI on EKG.
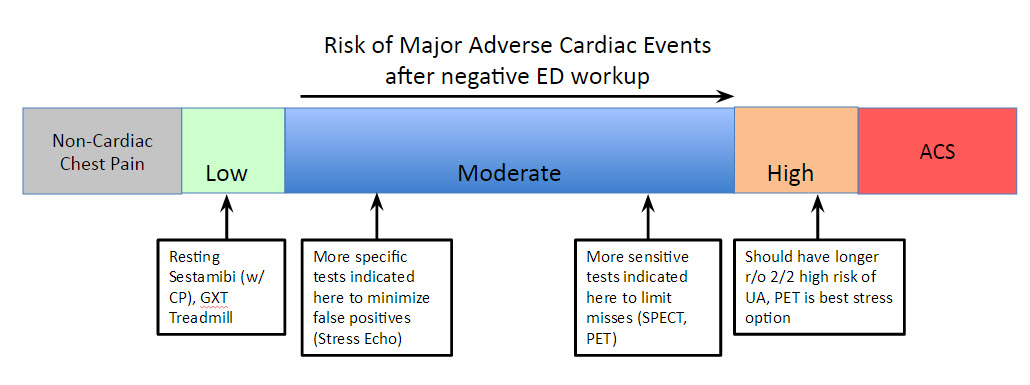
Cardiac Risk Stratification in the ED II: Stress Testing with Dr. Palmer
- Resting Tests: Radionucleotide Myocardial Perfusion Imaging (Sestamibi), Echo, CCTA
- Resting SPECT/Radionucleotide Myocardial Perfusion Imaging works as healthy myocardium binds an injected radionucleotide tracer whereas diseased myocardium does not. Tissue injected within two hours of injury (chest pain) will show pathology, and the test maintains accuracy if performed within 4 hours of injection because of a slow re-distribution rate.
- If no perfusion defect with pain=not ischemic in origin
- Perfusion defect with pain=possibly due to acute ischemia/infarct vs prior ischemic event
- Resting trans-thoracic echo (TTE) can be helpful (mainly in concern for acute infarct) although is not as valuable or accurate of a tool when compared to SPECT and is not used as part of our institutional protocols
- Coronary Computed Tomography Angiogram (CCTA). Requires heart rate to be <60bpm, subjects patients to a larger amount of radiation, and may yield, if mis-applied, high false positives. Remember, this test allows you to see anatomy, not physiology. Probably better for the intermediate risk population rather than low risk
- Udelson, et al - Prospective RCT validating safety of normal resting sestamibi and discharge from the ED
- Stress Tests - Exercise Treadmill (ETT), Stress Echo, Stress PET, Stress SPECT
- GXT (Graded Exercise Treadmill) - WPW, paced rhythms, LBB, LVH with strain cannot be interpreted accurately via GXT - need a perfusion study
- ETT has reasonably good specificity, is widely available, cheap, and if applied correctly to a symptomatic patient after negative ED workup yields low rates of MACE
- Stress rMPI/SPECT - Visualize myocardial perfusion during resting and stressed states. Normal resting + abnormal stress=ischemia. Abnormal resting + abnormal stress = infarct/scar. These tests have higher sensitivity and thus many state better applied in more concerning, moderate-risk patients (lower risk of false negative).
- Stress Echo - High specificity, ie useful in less concerning, moderate-risk CAD and does not subject patients to radiation. Note these tests are less accurate in patient populations with large breast tissue.
- Stress PET - This may be a diagnostic modality of choice in the near future. High sensitivity and specificity with lower rates of attenuation artifact and radiation make it a useful tool in intermediate to high risk patients, especially those with larger body habitus or known CAD/prior ischemic areas. Increasing availability now at UCMC
R1 Clinical Knowledge on Pulmonary Embolus with Dr. Shaw
- Clinical gestalt and Well's score are essentially equivalent, with a sensitivity of ~85% and a specificity of ~52% according to a recent meta-analysis, when used to determine the pre-test probability of PE for a given patient
- The PERC (Pulmonary Embolism Rule-Out Criteria) is a test, analagous to a D-Dimer, that you can apply to patient's in whom you have a low suspicion of PE (<15% probability) that, if all negative, reduces your post-test odds of PE to less than 2%
- D-Dimer can be applied to moderate-risk patients as a rule-out test though it will lead to many false positives for PE
- Many people are starting to use adjusted D-Dimer cutoffs for pregnant patients and the elderly though these are not yet accepted as standard of care
- High pre-test probability->definitive testing ie CTPA
- Treatment for PE depends on its classification:
- Massive PE (Hemodynamic collapse)--TPA
- Submassive PE--half dose TPA according to MOPETT to reduce pulmonary arterial hypertension
- Less than submassive PE--anticoagulation with lovenox bridge to warfarin vs novel anticoagulant
Clinicopathologic Conference with Drs. Renne and Powell
- Presents case is a male in his mid-30s, otherwise healthy, presents on 3rd visit for generalized weakness, cough, trouble getting out of bed and breathlessness with a physical examination revealing no neurologic deficits and no focal findings. A diagnostic test was ordered...
- Dr. Powell: In general, with repeat visits and continued diagnostic uncertainty consider getting the next best test. In this patient who had no prior testing Dr. Powell offers up a renal panel which aptly diagnosis the patient's new onset diabetes.
- Remember the 6th vital sign: blood glucose
- Correct Na by 2.4 for every 100 mg/dl above 100
- 95% of cerebral edema occurs in children; these are typically children who are sicker and with lower pH, with those who had received sodium bicarbonate at particular risk
R4 Case Follow Up with Dr. Nelson
- Patient is a female in her 30s with history of IVDU presents with lower abdominal pain for a few hours with complaints of fevers at home. She is notably tachycardic though afebrile. She does not have a murmur.
- Labs reveal a leukocytosis of 34k and a POSITIVE pregnancy test with a quant of 6k
- Repeat exam reveals an acute abdomen and tachycardia refractory to 1LNS
- Trans-abdominal US reveals no evidence of IUP. A RUQ US as part of a FAST is positive
- The patient proceeds to the OR with OB/GYN ~10 minutes later which reveals a large right, ruptured and hemorrhagic ectopic pregnancy
- Ectopic pregnancy remains the #1 cause of maternal death in the first trimester
- If you are worried about the stability of a patient in whom you suspect an ectopic, do a FAST
University of Cincinnati IGNITE! Session on UCEM Research
- UCEM consistently produces high quality, nationally recognized research with significant implications in the lab, hospital, community and at the bedside. For residents interesting in getting involved please talk to Dr. Lindsell, Dr. Hooker or your Chiefs.
- Dr. Lindsell: Creating new methods of classifying sepsis with significant clinical implications.
- Dr. Adeoye: Biomarkers may help differentiate stroke vs non-stroke at the bedside as a point of care resource that may lead to more effective intervention earlier in the disease process
- Dr. Lyons: The TESTED Trial is a multi-center effectiveness trial that may give us an idea of the best method for testing and detecting HIV in the ED
- Dr. Hooker: We may be able to characterize appropriate clinical conditions for use of the Woods' Lamp as acceptable ophthalmologic examination
![H. Influenza Meningitis. By Photo Credit: Content Providers(s): CDC [Public domain], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1441602267010-7U3851Z8MOK4Y0AB5KUN/image-asset.png)
![By James Heilman, MD (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons](https://images.squarespace-cdn.com/content/v1/53c1a2cce4b0e88e61f99b70/1441602405031-I3D5FYHQRPF2NFU02VVZ/image-asset.png)




