Grand Rounds Recap 3.1.17
/Morbidity and Mortality Conference with Dr. Axelson
Case #1:
Young female at approximately 8 weeks gestation by LMP, presenting with nausea and vomiting, recent visit to ED and discharged with ondansetron 2 days prior. Past medical history notable for type 1 diabetes being treated with insulin. Sugar on presentation noted to be 427, sodium 130, 80 ketones in urine, normal anion gap. Patient received 2 liters of IVF and prescribed promethazine, discharged home. 2 hours after being discharged presented to outside ED and admitted to ICU in DKA.
Diabetes in Pregnancy
- Pre-gestational diabetes: T1DM or T2DM prior to pregnancy
- Gestational Diabetes: typically diagnosed around 24 weeks gestation via glucose tolerance test. Can be diagnosed earlier in pregnancy if mother has risk factors for primary diabetes.
Pregnant DM Learning point #1: In pre-gestational DM, what are the risks to mom and baby in pregnancy?
- 1st trimester
- For mom: Increased insulin resistance and worsening glucose control
- For fetus: congenital abnormalities and intrauterine fetal demise
- Associated with as little as a 1% increase in hemoglobin A1c from baseline
- 5% will have cardiac defects
- Also at risk for neural tube defects
- Associated with as little as a 1% increase in hemoglobin A1c from baseline
- 3rd trimester
- For mom: preeclampsia, preterm labor, increased c-section rates and difficult delivery
- For fetus: macrosomia, polyhydramnios, and neonatal hypoglycemia
Pregnant DM Learning point #2:: How does DKA differ in pregnancy?
- Pathophysiology is unchanged, however, acidosis is transferred directly to fetus
- Fetal heart rate in DKA can develop to category 3 tracing (minimal variability, decelerations)
- 36% of DKA in pregnancy will present with blood glucose less than 200
- Fetal mortality rates of 9-36% reported for maternal DKA
- Management is similar to non-pregnant patients and delivery is typically not required
Pregnant DM Learning point #3: How do I manage non-DKA hyperglycemia in pregnancy?
- Progression to DKA between type I and type II DM varies
- Type I DM found to progress from hyperglycemia to DKA between 78-86% of cases in two studies
- Pregnant patient with pre-gestational diabetes with fingerstick blood glucose greater than 200 requires check for ketonuria
- Pregnant patient with pre-gestational diabetes and an illness or physiologic stressor requires checking of sugar and urine ketones
- Pregnant patient with pre gestational diabetes and a fingerstick blood sugar greater than 200 with or without ketonuria requires insulin administration and admission to hospital
- goal blood sugar is between 60-90, very tight glycemic control
Case #2:
Middle aged male patient with presenting from nursing home with altered mental status. Noted to have sodium of 120 on renal panel. Noted to be afebrile with normal vital signs otherwise. Question as to whether patient was euvolemic v hypovolemic, patient placed on 100ml/h of NS. Serial sodium levels continue to drop so patient is transferred to MICU.
Hyponatremia
Hypotnatremia learning point #1: My patient’s sodium is low, how can I mess this up?
- Correct hyponatremia too fast
- Goal is to correct at rate less than 6 to 8 meq/L in any 24 hour period
- If you’re not willing to calculate a fluid correction rate, not giving fluids is ok! (presuming chronic hyponatremia)
- 1-2 Liter bolus of NS is enough to overcorrect, be cautious.
- Giving 0.9% NaCl to an SIADH patient
- results in further drop in sodium level by desalination
- if urine osmolarity is more concentrated than the fluid you’re infusing, body treats that as free water and dumps further sodium to get rid of it.
- results in further drop in sodium level by desalination
Hyponatremia learning point #2: We are not as good at evaluating volume status as we think we are.
- Board certified nephrologists in evaluating volume status in SIADH as euvolemic vs hypovolemic are accurate in assessment in only 48% of cases in one study
- As such, get the urine studies to complete this volume assessment
Hyponatremia learning point #3: Break it down into simple break points
Case #3:
Incidentalomas Learning point #1: look at your radiology studies
Incidentalomas Learning point #2: Incidental findings are a big deal
- In CT scan of abdomen/pelvis found to have 5-16% of scans will have a clinically significant incidental finding in one study
Learning point #3: Use a dot phrase and put in the diagnosis
- .edradincidental to pull up a script for discharge instructions
Learning point #4: If significant, make someone aware
Case #4:
Middle aged female presenting to emergency department with complaint of hematemesis and altered mental status, history of alcoholism and liver disease. Hypotensive, tachycardia, lactate elevated, acute elevation in transaminase, anemic, and INR is elevated. Patient resuscitated with IVF bolus, PRBC, pantoprazole drip, ceftriaxone and admitted to MICU.
Upper GI Bleed Learning point #1: How should I prioritize stuff I give for upper GI bleed?
- PPI noted to have reduction in upper GI bleed rate (6% vs 23% for placebo), no effect on mortality. Of note, BID PPI as efficacious as IV drip, also oral PPI as efficacious as IV in general.
- Octreotide: decreases chance of re-bleed from esophageal varices, not for other sources of GI bleed, no effect on mortality.
- Ceftriaxone: rate of mortality from upper GI bleed in all comers decreased with administration of ceftriaxone in ED. Number needed to treat of 22 for mortality, NNT of 4 for infection prevention.
- Consider the following priority order: resuscitation/blood if needed -> ceftriaxone -> PPI -> Octreotide if concerned for varices.
Upper GI Bleed Learning point #2: What's the data for TXA in GI bleed?
- TXA when analyzed in literature during age of endoscopy found to have no mortality benefit
- Current trial is ongoing, stay tuned for future literature.
Upper GI Bleed Learning point #3: Which upper GI bleed patients can I send home?
- Consider the Blatchford score or Modified Blatchford score: the higher the score, the more likely the patient is to need endoscopic intervention
- Score of 0 in either can consider for outpatient management (considering patient has good outpatient followup)
Case #5:
Elderly female with history of T cell lymphoma presenting to ED with weakness. Vitals look normal. Found to have elevation of WBC to 53, elevation of uric acid, concern for tumor lysis syndrome.
Tumor Lysis Syndrome Learning point #1: Electrolyte control is key
- Tumor lysis syndrome results in massive release of potassium, phosphate and DNA into bloodstream, broken down to uric acid which can precipitate in kidneys and cause renal failure.
- Typically begins after initiation of cytotoxic therapy
- Tumors with high proliferative rate (NHL, ALL, Burkitt lymphoma, T-cell lymphoma) are at higher risk as are high solid tumor burden.
Tumor Lysis Syndrome Learning point #2: Will I see tumor lysis syndrome?
- 17% of leukemia patients undergoing chemotherapy stuffer this
- It is associated with significantly higher risk of death during induction
- 6 month mortality ranges from 21% to 66% if AKI present
Tumor Lysis Syndrome Learning point #3: How do I treat tumor lysis syndrome?
- IVF for resuscitation, electrolyte management
- Hemodialysis if refractory hyperkalemia, serum creatinine greater than 10 or volume overload
- Consider rasburicase
R3 Taming the SRU with Dr. Renne
Elderly male patient was in distress while swimming at gym, pulled from pool and entered cardiac arrest, 5 minutes of bystander CPR, received shocks from EMS and is intubated, arrives undergoing CPR. Continues in VT/VF, doses of amiodarone, epinephrine, defibrillation. Obtained ROSC, EKG shows anterolateral STEMI and patient called to cath lab.
Intra-arrest Quick Hit #1: Intra-arrest arterial lines
- Intra-arrest arterial lines eliminate pulse checks, can save valuable chest compression time
- Would be concerning to give full dose epinephrine to a beating heart
- AHA consensus statement suggests a-line/capnography with rhythm on monitor as possible other option to traditional pulse checks
- Also consider an arterial line as a ROSC safety net (a more point of care and in real time monitor of patient’s perfusion)
- Can give good feedback in terms of quality of CPR
- AHA consensus also reports expert panel recommendation of titration of diastolic blood pressure to greater than 25 mmHg, relies on quality of CPR and titration of epinephrine, would require arterial line for in time monitoring.
- Arterial line for frequent arterial gasses and labs
Patient goes into cardiac arrest again, refractory to multiple shocks in spite of continuing and refractory VT/VF. Underwent double sequential defibrillation (DSD)
Intra-arrest Quick Hit #2: DSD
- Is the energy safe? Porcine study finding no difference in post shock cardiac function via troponin level and echocardiography.
- Is the energy effective? In case series, 5/5 refractory V fib patients converted, 7/10 in another case series.
Continued in cardiac arrest, more shocks and IV magnesium, discussion with cath team about IV esmolol drip. Patient progressed to PEA, cardiac standstill on ultrasound, expired.
Intra-arrest Quick Hit #3: Esmolol in electrical storm
- Theory: beta 1 blockade improves myocardial oxygen supply and demand
- blocking beta 1 while still allowing alpha vasopressor effect of epinephrine to continue
- Retrospective case series in patients with refractory V fib, double numbers for patients with ROSC and survival to ICU, possible improvement in neurologically intact discharge
- Can administer as 500 mcg/kg bolus
- Possible concern for patient with large MI and acute heart failure with reduced ejection fraction.
9 minutes after time of death, patient noted to be breathing spontaneously, BP 180/90, 89% on room air, HR 59.
Intra-arrest Quick Hit #4: Autoresuscitation
- Of all studies on subject, maximum time after time of death for auto resuscitation noted to be 33 minutes, however, of those with precise timing maximum time is 7 minutes.
- How does this happen?
- No idea. Theories are myocardial stunning, delayed drug response, hyperinflation (discontinuation of positive pressure ventilation allows for increased venous return).
Patient found to have complete LAD in cath lab, GCS 4T with myoclonus, in cardiogenic shock post ROSC, anoxic brain injury on CT.
Adult Congenital Heart Disease (ACHD) with Dr. Nicole Brown
- Survival to 18 years of age with ACHD has improved from 20% in 1940 to 90% as of 1980 (greater than 80% for complex congenital heart disease)
- in 2010, 66% of patients with congenital heart disease are adults, outnumbering pediatric congenital heart disease by 2:1
- There is a huge concern and problem of patients being lost to follow up with congenital heart disease as they get older.
- by age 18 only 38% are visiting with cardiology routine follow up
- Emergencies in ACHD patients
- Case #1
- 42 year old female with tricuspid atresia ultimately underwent classic atriopulmonary Fontan at 12 years old. Found to be in atrial fibrillation at clinic visit with good rate control, found to have a right atrial/Fontan thrombus, had developed multiple pulmonary emboli. Underwent tPa thrombolysis and eventually discharged on amiodarone and coumadin.
- Adult patient with atrial Fontan will have large dilated right atrium, if you need to defibrillate/cardiovert they respond better to anterior/posterior pad placement as opposed to both anterior.
- Single ventricle patients after Fontan are at risk for PE, but beware of false diagnosis of such or inadequate study
- Case #2
- 24 year old female with tetralogy of fallot, underwent full repair with VSD patch closure at 1 year of age, presenting to ED with shortness of breath, fatigue, and exercise intolerance, progressing over past 2 years.
- Some older repairs allowed for regurgitation in right ventricle in order to avoid pulmonary stenosis or hypertension, may have large regurgitant right ventricles
- 24 year old female with tetralogy of fallot, underwent full repair with VSD patch closure at 1 year of age, presenting to ED with shortness of breath, fatigue, and exercise intolerance, progressing over past 2 years.
- Case #3
- Loeys-Dietz syndrome is at high risk for aortic aneurysm
- Most common reasons for ED visits: chest pain, palpitations, shortness of breath and syncope.
- Case #1
R3 Small Groups with Drs Polsinelli, Shah and Ludmer
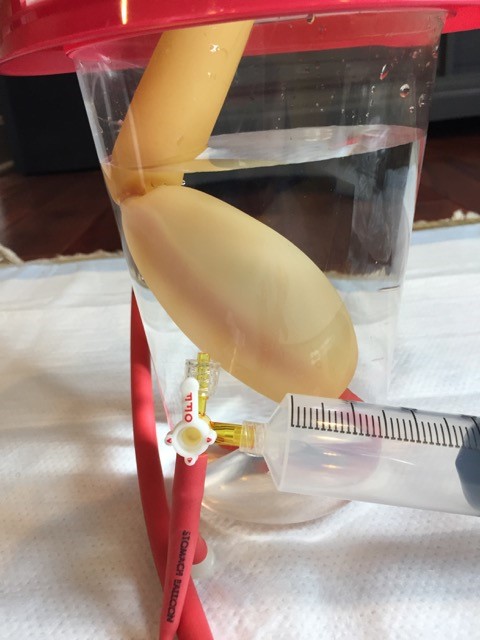
Minnesota Tube Placement with Dr. Polsinelli
- Step 1: Intubate the patient (for airway protection as well as for adequate sedation)
- Step 2: Place patient at 45 degrees or left lateral decubitus position
- Step 3: Place 3 way stop cocks in balloon ports (stomach ball and esophagus balloon labeled on tube), ensure small port is clamped to not allow air leak
- Step 4: test balloons in a bucket of water to look for air leak (bubbles). Make sure you fully deflate after test
- Step 5: Lubricate the ballons and tube well
- Step 6: Place tube beyond the 50 mark, preferably orally, same method as placing an OG tube
- Dr. Otten tip: deflate ETT balloon transiently during passage of minnesota tube to allow it to pass. Also, to facilitate placement consider using laryngoscope blade placed in esophagus, assist passage of tube with magill forceps.
- Step 7: Inflate stomach balloon with only 50 cc of air at first, it becomes diameter of esophageal balloon, confirm with x-ray that it is below diaphragm before further inflation to full volume of 450 cc. Don’t over-inflate, rupture of the balloon would be bad news as well.
- Step 8: Double clamp ports with hemostats to ensure no leakage
- Step 9: Apply traction. Can do to football helmet applied to patient, also consider 1 L bag IVF tied to tube and slung over IV pole, allows for access to airway if needed.
- Step 10: Mark the location of the tube at the patient's teeth with marker
- Step 11: Hook the gastric port up to intermittent low to moderate suction
- Step 12: Hook the esophageal port up to low continuous suction, if bleeding persists, continue to next step
- Step 13: Attach the manometer to the valve of the esophageal inflation port and inflate to 25 mmHg. BE CAREFUL! It does not take much squeeze to reach goal.
- Step 14: Use two Kelly clamps with teeth wrapped in tape to clamp off the esophageal inflation tube
- Step 15: If bleeding persists, increase the pressure in the esophageal balloon to a maximum of 40mmHg.
- Step 16: If esophageal balloon inflated over 25mmHG, try to deflate it every 2-3 hours in increments of 5 back to 25mmHg
- Step 17: Every 4-6 hours deflate the esophageal balloon and then re-inflate to 25mmHg
Reminders:
- Never leave the esophageal tube inflated for more than 12-24 hours
- Never deflate the gastric balloon unless you have deflated the esophageal balloon first AND you are removing the tube
- If the gastric balloon becomes deflated, you must re-verify position of the gastric balloon positioning before you re-inflate the gastric balloon
- Scissors should be at bedside to cut tube to be able to remove it immediately if needed
- Reassess patient frequently when tube is in place for evidence of malpositioning or pressure ulcer risk
Tips & Tricks
- The endotracheal balloon may need to be temporarily deflated to release esophageal compression and allow the tube to pass
- Try using a laryngoscope and Magill forceps to visually begin passing tube into esophagus
- Try bougie assisted placement with the straight end of the bougie through the proximal gastric aspiration eyelet. Remove the bougie after blowing up the gastric balloon.
Shoulder ultrasound for dislocations with Dr. Shah
- Probe placement on back in transverse orientation just inferior to scapular spine, transecting glenohumeral joint.
ACLS “Plus” with Dr. Ludmer
- Mortality in cardiac arrest drops with every minute following arrest
- At 20 minutes of resuscitation have reached 1% survival to discharge
- Time to interventions is key: the sooner you initiate compressions, defibrillation and drugs when indicated, the better
- Plan ahead if you have advance warning in order to minimize interruptions in compressions