Grand Rounds Recap 9/9
/Case Follow up with Dr. Winders
The Sick Patient with Pulmonary Artery Hypertension (PAH)
- PAH defined as right heart catheterization with mPAP > 25mmHg, which can be estimated by echo
- Readily associated with right ventricular failure, measured by TAPSE < 1.8 with M mode over tricuspid annulus
- EKG can also help identify these patients with right axis deviation or right atrial enlargement
Hypoxia in PAH
- Airway status can be tenuous in these patients - a retrospective review found 100% mortality in a 2 year cohort in patients that require intubation, should be used as a last resort
Hypotension in PAH
- Make sure you are dealing with isolated RVF
- Look for secondary causes, pneumonia, COPD, PE
- If on continuous vasodilators, check the connections (tube kinking, empty cartridge)
- Fluid status optimized and need pressors?
- Norepi vs Epi - no great data and both a readily used
- Dobutamine vs Milrinone - Dobutamine more likely to cause tachydysrythmia and tachycardia, milrinone tends to drop your pressure initially
- Fluid overloaded?
- Per our PAH specialists - diurese these patients despite the AKI as it tends to improve with better forward flow
- Other tips
- Place large lines if placoing them as likely to need swan
- SCVo2 can useful for med titration
Case Follow up with Dr. Shah
Middle aged female with vague respiratory symptoms that had undergone multiple prior antibiotic courses and has 1+ peripheral edema and a new murmur.
Causes of Mitral Regurgitation
- Papillary Rupture (2-7d after MI)
- Leaflet/chordae dysfunction
- Cardiomyopathy/global dysfunction (ischemic, infectious/septic, metabolic)
- Mortality benefit for CAD + MR, get CT surgery involved as may be candidate for early CABG plus valve replacement
Treating the Cardiogenic Shock
- Optimize preload, contractility and afterload as bridge to the only long term solution once to the point of shock - surgery
- Increase your suspicion for repeat visits - this patient had multiple antibiotic treatments for questionable CXR findings that were likely 2/2 pulmonary edema from gradually worsening MR - in these patients have a low threshold for getting echo, BC in someone with a suspicion for endocarditis
EMS Event Medicine with Dr. Leblanc
Why did Event Medicine become a thing?
A few tragic sentinel events led to the specialty and a rethinking of how to appropriately manage and care for mass gatherings
- 1965 - Nebraska Football - 2 cardiac arrests in one year and implemented CPR teaching, defibrillation and save 8/9 people over the next several seasons
- 1979 - Cincinnati Ohio - 15,000 general admission tickets to The Who's concert lead to an enormous stampede - 11 deaths - 26 injured and barring of GA seating for decades within the city.
Why does this fall to our specialty?
- Chaos begets chaos - coming from EM we have a baseline knowledge of organization but this takes it to another level. To organize it - events management are based off ICS (standardized incident command system)
START Triage / SALT Triage - Both great systems with their own benefits - pick at least one to know and know well - when the situation occurs when you need it there won't be time to look it up
Tips of setting up Med Control for events
- Assess your population, your duration and your nearest resources as most of your utility is not in definitive care but your ability to get people where they need to be for definitive care.
Clinical Knowledge with Dr. Randolph
Aortic Dissection
Dissection starts with an intimal tear separating it from the tunica media
Stanford A - Retrograde flow, higher risk of coronary involvement, MI
Stanford B - Distal to the left subclavian
40% of patients with dissecton do not make it to the hospital, and those that do have classic presentations.
- 25% are missed on initial presentation
- 84% had acute onset of the pain, but only 16% radiated from the front to the back
- EKG neither sensitive nor specific
- 88% of CXR show some abnormalitiy (widened mediastinum, pleural effusion)
IRAD - Males in their 60s with HTN were the classic presentations
D-Dimer? Data still equivical and ACEP defers to traditional testing for risk stratification, the CTA being the gold standard (100% sensitive)
Treatment goals
- Get your consultants involved early - Type A: Cardiothoracic Surgery, Type B: Vascular Surgery
- Heart rate and BP with goals of HR ~60 and BP ~100. Esmolol is easily titratable and the first line, CCB, vasodilators second line
R4 Capstone with Dr Denney
Sick, hypotensive, hypoxic female found down at home presents O2 sat 70% on NRB, 66/46, HR 140s. Does she buy a tube? YES
These patients are at high risk of peri-intubation mortality
caution - RSI can be as dangerous as the laryngoscope as a cause of peri-intubation arrest
Could ketamine induce hypotension?
We usually rely on the sympathomimetic effects brought on by cathecholemine release, however it does decrease myocardial contractility as well.
If you have someone that has maxed out their catecholamines, you may get hypotension - so be ready for push-dose pressors
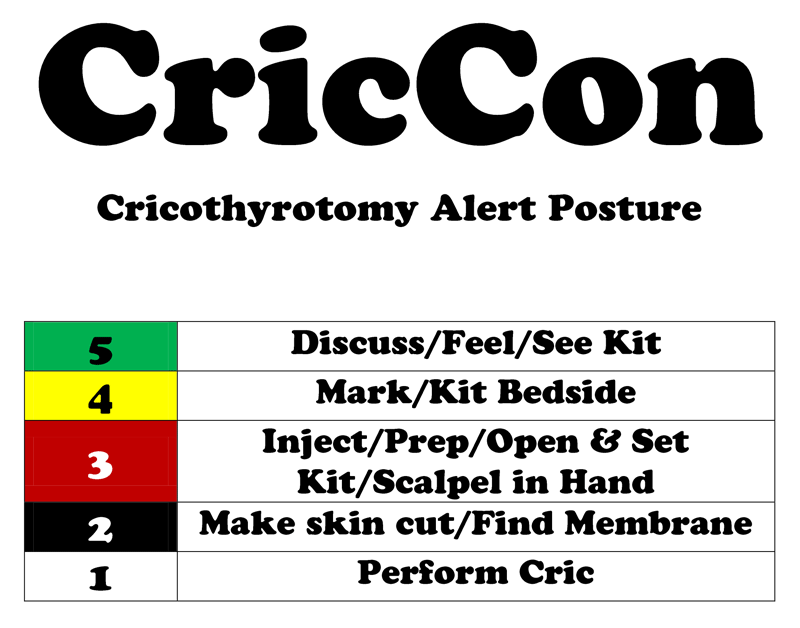
Have a low threshold for cric preparation. EMCrit has a great guide for how to prepare for a cric in a staged manner such that it is never a last-minute unprepared surprise.
Pediatric Status Epilepticus
First lines - benzodiazipines - ativan shown more efficacious if IV access, if not move quickly to IM/IN midazolam. Give 2 weight-based dosing 5 minutes apart, any additional doses are less likely to be effective and more likely to increase your side-effect profile (hypopnea, hypotension)
Second line - fosphenytoin, keppra, divalproate - no great data but closely monitor your respiratory status and consider intubation. If these aren't working, move towards barbiturates... but the patient likely shouldn't be in the ED anymore
Check out CCHMC's evidence based algorithmic approach to status and many other medical emergencies here
Case Studies at CCHMC
Infantile Botulism - floppy baby presenting with general fatigue and baby not able to hold is head up
Only 20% cases reported from honey exposure, when most comes from soil (direct exposure, family members clothing, etc)
Most common in the 2m-2y with the highest incidence <6m
PE: Constipation common, Weakness all develop over 4-5 days
Treatment: Antitoxin started (ordered if not a center that stores it) concurrently with diagnostic confirmation as likely a send-out test