Mastering Minor Care: Knee Arthrocentesis
/INDICATIONS
Arthrocentesis is a common procedure performed in the Emergency Department, in which a needle is inserted into a joint to withdraw fluid from the joint capsule. This procedure may be performed for diagnostic and/or therapeutic purposes [1]. Diagnostic arthrocentesis is often performed to distinguish between septic arthritis and other common causes of acute monoarthritis including hemarthrosis, crystal arthropathies (gout, psedogout), and autoimmune arthropathies (SLE, RA, etc.) [2]. Removal of a knee effusion via arthrocentesis can also have therapeutic benefit, and may be performed solely for this purpose [3].
While there are no absolute contraindications to performing this procedure, risks and benefits should be carefully weighed in the presence of overlying infection and coagulopathy. Additionally, orthopedic surgery consultation should be considered when the joint of interest contains a prosthetic component. [2]. Complications that may arise from this procedure include infection and damage to tendons, nerves, or vascular structures.
APPROACHES
Due to the large size of the knee joint, multiple approaches can be used in order to successfully access the joint space. The joint space may be accessed either superior, medial, or inferior to the patella, with needle entry either medial or lateral relative to the patella at each of these levels [5].
After the patient is positioned appropriately (see below), palpate the patella to assess which area allows for the widest margin for access. The needle should be directed posteriorly to the patella, with a trajectory pointing toward the intercondylar notch.
EQUIPMENT
LANDMARK-GUIDED PROCEDURE
Step 1: Obtain consent for the procedure
Step 2: Gather supplies
Step 3: Position the patient
Patient lies supine with the knee fully extended ot held in slight flexion.
Consider placing a towel roll underneath the knee joint to facilitate slight flexion.
step 3. supine positioning with knee fully extended
step 3. SUPINE POSITIONING WITH KNEE HELD IN SLIGHT FLEXION USING A TOWEL ROLL
Step 4: Identify landmarks and plan approach
See above for description of approaches.
No single approach has been proven to be superior.
Step 5: Prep and drape the joint
Prepare the skin over the entire knee joint in the event that multiple approaches need to be utilized.
STEP 5. APPLY A SKIN PREPARATION SOLUTION TO THE SKIN OVER THE KNEE JOINT
step 5. drape the joint with sterile towels
Step 6: Anesthetize the area
Inject a small amount of lidocaine to create a skin wheal at the planned needle entry site.
Inject additional lidocaine into the deeper structures along the anticipated needle trajectory.
Step 7: Perform arthrocentesis
Enter the skin with the needle and advance while applying negative pressure on the attached syringe.
If the needle encounters bone, retract the needle as much as possible without exiting the skin. Then redirect the needle appropriately based on this feedback.
Consider alternate approach if multiple attempts using this strategy are unsuccessful.
Synovial fluid with enter the syringe when the joint capsule is entered. Collect a sample for laboratory testing.
Application of gentle pressure to the supra-patellar region can help “milk” the effusion during collection.
With large effusion, removal of additional fluid through multiple syringes may be necessary to achieve adequate pain control. After the attached syringe is filled, hold the needle in place proximally (adjacent to the skin surface), while attaching a new syringe to maintain positioning without the joint capsule.
Withdraw the needle and apply pressure to the entry site until any bleeding stops. Place an adhesive bandage over the site.
STEP 6. ANESTHETIZE THE AREA
step 7. perform arthrocentesis
ULTRASOUND-GUIDED PROCEDURE
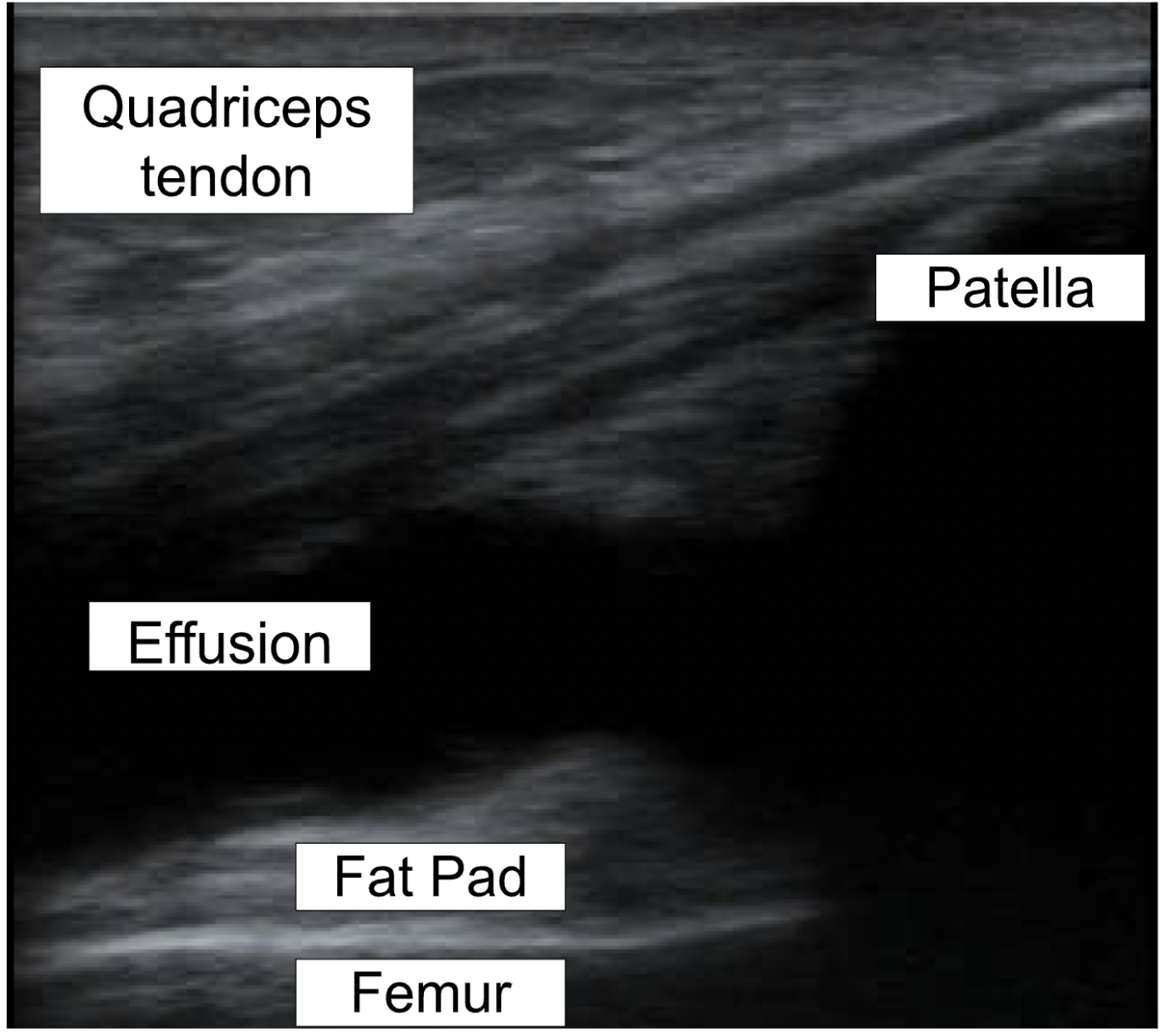
Ultrasound-guided (USG) arthrocentesis may be helpful in instances where there is no obvious effusion that can easily be palpated on physical exam. Studies have shown that effusions of as little as 2 to 4 mL can be identified using ultrasound [6]. Even in instances where effusions are obvious, ultrasound has become a heavily utilized technique due to multiple advantages over “blind” or landmark-guided approaches. US allows for real-time visualization of the needle, potentially increasing first-pass success rate [7]. Studies have shown that ultrasound needle guidance helped reduce the number of attempts and maximized the amount of effusion removed [8]. Overall, US has been found to be less time-consuming, less technically difficult, less painful, and has increased procedural success [6,9]. When utilizing US, it is important to visualize varying structures such as the patella, femur and quadriceps tendon.
Step 1: Prepare
STEP 2. USE ULTRASOUND TO IDENTIFY ANATOMY AND LOCATE EFFUSION (LONGITUDINAL PLANE)
Obtain patient consent, gather supplies, prep and drape, and anesthetize as described above.
Place a sterile cover over the ultrasound probe and have sterile ultrasound gel available.
Step 2: Use ultrasound to identify relevant anatomy and locate effusion
Place the linear ultrasound probe in the longitudinal plane at the junction between the femur and patella.
Identify the patella, quadriceps tendon, and suprapatellar fat pad.
Step 3: Visualize effusion in the transverse plane
Rotate the ultrasound probe 90 degrees. The probe marker should point to the patient’s right.
Step 4: Perform ultrasound-guided arthrocentesis
Direct the needle into the effusion under ultrasound visualization, utilizing in-plane technique.
This may also be performed utilized out-of-plane technique, but care must be taken to ensure that the needle tip is visualized throughout the procedure.
See above for general arthrocentesis technique.
QUICK REFERENCE
Post by Julius de castro, MD AND colleen arnold, md
Dr. De Castro is a PGY-2 in Emergency Medicine at the University of Cincinnati
Dr. Arnold is a PGY-2 in Emergency Medicine at the University of Cincinnati and Mastering Minor Care Section Editor
Editing by alexa sabedra, MD and ANITA GOEL, MD
Dr. Sabedra is an Assistant Professor at the University of Cincinnati and a graduate of the UC EM Class of 2019
Dr. Goel is an Assistant Professor at the University of Cincinnati and a graduate of the UC EM Class of 2018
References
Roberts, W. N. (2023, October 9). Joint aspiration or injection in adults: Technique and indications. UpToDate. https://www.uptodate.com/contents/joint-aspiration-or-injection-in-adults-technique-and-indications
Akbarnia, H., Saber, A., & Zahn, E. (2022, August 29). Knee arthrocentesis - StatPearls - NCBI bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470229/
Villa-Forte, A. (2023, June). How to do knee arthrocentesis - musculoskeletal and connective tissue disorders. Merck Manuals Professional Edition. https://www.merckmanuals.com/professional/musculoskeletal-and-connective-tissue-disorders/how-to-do-arthrocentesis/how-to-do-knee-arthrocentesis
Tieng, A., & Franchin, G. (2022, February 25). Knee Arthrocentesis in Adults. Journal of visualized experiments : JoVE, (180), 10.3791/63135. https://doi.org/10.3791/63135
DeVivo, A. (2019, April 30). Unlocking Common ED Procedures – Is there Water on the Knee?: Arthrocentesis in the ED. emDOCs.net - Emergency Medicine Education. http://www.emdocs.net/unlocking-common-ed-procedures-is-there-water-on-the-knee-arthrocentesis-in-the-ed/
Gottlieb, M., & Alerhand, S. (2020). Ultrasound should be considered for all Arthrocentesis. Annals of Emergency Medicine, 75(2), 261–262. https://doi.org/10.1016/j.annemergmed.2019.04.018
Harrison, C. W. (2021, October 28). Arthrocentesis. ACEP. https://www.acep.org/sonoguide/procedures/arthrocentesis
Josie Acuna, Adrienne Yarnish, Elaine Situ-LaCasse, Richard Amini & Srikar Adhikari (2021) The Use of Point-of-Care Ultrasound for Arthrocentesis Among Emergency Medicine Residents, Open Access Emergency Medicine, 13:, 161-167, doi: https://10.2147/OAEM.S305762
Springer B, Pennington B (2017). “Joint Arthrocentesis in the Emergency Department” Emergency Medicine Reports, October; 38(19):217-231.
Reichman E.F.(Ed.). Chapter 77. Arthrocentesis. (2013). Emergency Medicine Procedures, 2e. McGraw Hill. https://accessemergencymedicine.mhmedical.com/content.aspx?bookid=683§ionid=45343718
Wiler JL, Costantino TG, Filippone L, Satz W. Comparison of Ultrasound-Guided and Standard Landmark Techniques for Knee Arthrocentesis. The Journal of Emergency Medicine. 2010;39(1):76-82. doi:https://doi.org/10.1016/j.jemermed.2008.05.012