Mastering Minor Care: Nasal Septal Hematoma
/Introduction
The nasal septum is composed of bony and cartilaginous components, and is lined on both sides by mucoperiosteum or mucoperichondrium, respectively. When bleeding occurs within this confined space, a nasal septal hematoma is formed. Nasal septal hematomas are most commonly caused by nasal trauma or are iatrogenic in nature (recent nasal surgery, etc.) and typically present within 24 to 72 hours post-injury. However, atraumatic nasal septal hematomas have been reported, particularly in patients with coagulopathy, including anticoagulant/antiplatelet use [1].
Although nasal septal hematomas only occur in 0.8% to 1.6% of patients with a nasal injury, over 50% of cases are missed during initial evaluation [1]. Delayed diagnosis results in significant and sometimes permanent complications, namely necrosis of the nasal cartilage, septal abscess, and saddle nose deformity, which can occur as early as 2-3 days following the injury [2]. Therefore, nasal septal hematomas require prompt intervention in the Emergency Department.
DIAGNOSIS AND EVALUATION
The diagnosis of nasal septal hematoma is typically based on history-taking and physical examination. Patients commonly present with nasal obstruction (95%) and pain (50%), but complaints may also include rhinorrhea (25%), and fever (25%) if there is associated infection. Physical exam should be performed using a nasal speculum or an otoscope. Identification of nasal septal hematomas can be made by the presence of swelling of the nasal septum, typically in the setting of recent facial trauma [3]. Patients may present with asymmetric bluish or reddish mucosal bulging and a boggy septum upon palpation. Nasal septal hematomas are often unilateral, though may occur bilaterally, especially in cases of severe facial trauma. A distinguishing diagnostic feature of nasal septal hematomas is the ineffective reduction of swelling by vasoconstrictive agents, such as oxymetazoline. A needle aspiration can be done to confirm the diagnosis but is not imperative [1].
Although nasal septal hematoma is usually a clinical diagnosis, a contrast-enhanced CT scan may be used in situations of diagnostic uncertainty, unknown underlying etiology, or when alternative causes are suspected (syphilis, sarcoma, lymphoma, TB, or granulomatosis with polyangiitis) [4].
MANAGEMENT
As previously mentioned, timely diagnosis and treatment of nasal septal hematomas is essential to prevent complications. Once identified, drainage of the nasal septal hematoma is indicated.
Step 1: Prepare
Obtain informed consent (if possible).
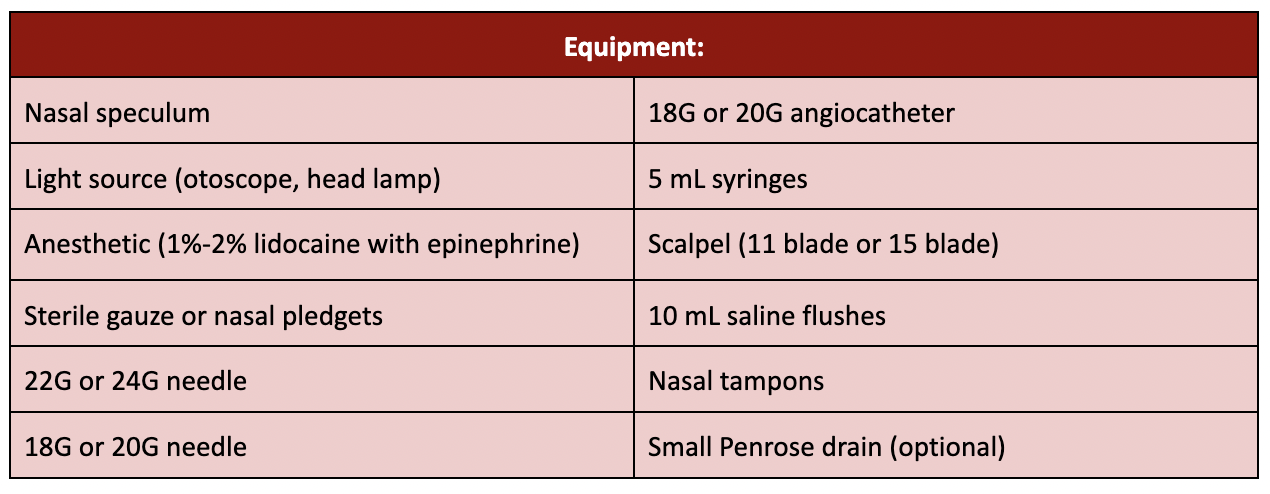
Gather the materials listed above.
Oriented the patient in a supine position with the neck slightly extended.
Step 2: Anesthetize the nasal septum
Soak two pledgets in lidocaine with epinephrine.
Can alternatively roll up sterile gauze if pledgets are not available.
Place the pledgets or gauze rolls into both nares, along both sides of the patient’s nasal septum.
Allow 5-10 minutes for the topical anesthetic to take effect.
Remove the pledgets/gauze and inject small amounts of local anesthetic into the superficial nasal septum at the anticipated incision site.
Step 3: Aspirate the hematoma
Once anesthetized, insert a 18G or 20G needle into the nasal septal hematoma and aspirate with a 5ml syringe. This may successfully evacuate small hematomas.
Step 4: Incise the septum and evacuate the hematoma
Use a scalpel to incise the epithelium in an anterior/posterior direction along the inferior border of the nasal hematoma.
This incision needs to be sufficient to prevent the reaccumulation of a hematoma .
If bilateral nasal septal hematomas are present, stagger the height of the incision on each side of the nasal septum.
Evacuate the hematoma.
Direct evacuation method: extract clotted blood with small forceps.
Suction method: use a small suction catheter (eg. Frazier suction tip).
Gently irrigate the incised area with saline using an 18-20G angiocatheter.
Step 5: Pack the nares
Pack both nares with a nasal tampon.
Attempt to advance the nasal tampon posteriorly to ensure tamponade.
Impregnate the nasal tampons with sterile saline.
Optional: Some sources recommend placing a small Penrose drain in the open hematoma and securing it with a suture.
DISPOSITION
If there are no other injuries necessitating hospitalization, patients may be discharged from the Emergency Department following successful hematoma evacuation. Patients should be placed on prophylactic antibiotics. While there is no clear consensus on antibiotic choice, amoxicillin-clavulanate (875 mg PO BID for 7 days) is a reasonable choice. If there is concern for a nasal septal abscess, Staph aureus coverage with doxycycline (100 mg PO BID for 7 days) is recommended [3]. If the aspirated contents of the hematoma appear necrotic, obtaining a culture of the fluid may be useful to guide future antibiotic therapy [1,3].
Patients should follow up with an ENT specialist (or in the Emergency Department if this is not feasible) 24-48 hours from discharge. At this appointment, the packing is removed and the area is re-examined to assess for infection and/or reaccumulation of the hematoma. Patients should be advised to return to the Emergency Department if they experience fevers, trouble breathing, or if the nasal packing dislodges [1].
Post by sarah ray, alexander treon, AND COLLEEN arnold, md
Sarah is a third-year medical student at the University of Cincinnati College of Medicine
Alexander is a third-year medical student at the University of Cincinnati College of Medicine
Dr. Arnold is a PGY-3 in Emergency Medicine at the University of Cincinnati and Mastering Minor Care Section Editor
Editing by ALEXA SABEDRA, MD and ANITA GOEL, MD
Dr. Sabedra is an Assistant Professor at the University of Cincinnati and a graduate of the UC EM Class of 2019
Dr. Goel is an Assistant Professor at the University of Cincinnati and a graduate of the UC EM Class of 2018
References
Gupta, Gunjan. and Kunal Mahajan. “Nasal Septal Hematoma.” StatPearls, StatPearls Publishing, 8 August 2023.
Ali, Hawa M et al. “Nasal septal hematoma in children: Time to diagnosis and resulting complications.” International journal of pediatric otorhinolaryngology vol. 145 (2021): 110734. doi:10.1016/j.ijporl.2021.110734
Kass, Jason I., and Berrylin J. Ferguson. “Treatment of hematoma of the nasal septum.” New England Journal of Medicine, vol. 372, no. 22, 28 May 2015, https://doi.org/10.1056/nejmvcm1010616.
Alshaikh, Nada, and Stephen Lo. “Nasal septal abscess in children: From diagnosis to management and prevention.” International Journal of Pediatric Otorhinolaryngology, vol. 75, no. 6, June 2011, pp. 737–744, https://doi.org/10.1016/j.ijporl.2011.03.010.
Original Illustrations by Stella Ray