Shock Differently - Out of Hospital Cardiac Arrest
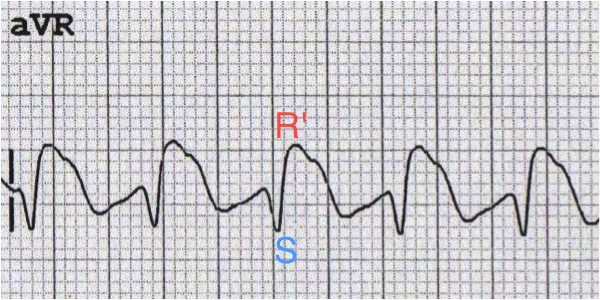
/Out of hospital cardiac arrest (OOHCA) represents a great cause of morbidity and mortality. Approximately 350,000 cardiac arrests occur in North America annually and 20% can be attributed to Ventricular tachydysrhythmias (i.e. ventricular tachycardia [v fib] and ventricular tachycardia [v tach]without a pulse). In this journal club recap, Dr Kelly Tillotson recaps an article comparing different ways of defibrillation and their effect on outcomes in OOHCA
Read More