Therapeutics: Nephritic, Nephrotic and the Glomerulonephridities in between
/The urinalysis is a ubiquitous test in the Emergency Department, often used to assess for various pathologies from infection to ureterolithasis. However the UA can go well beyond these to hint at the complexities of pathophysiology of the kidney and its components. In this post we will review the pertinent physiology and get into causations to consider in the UA that is ‘abnormal’.
Physiology
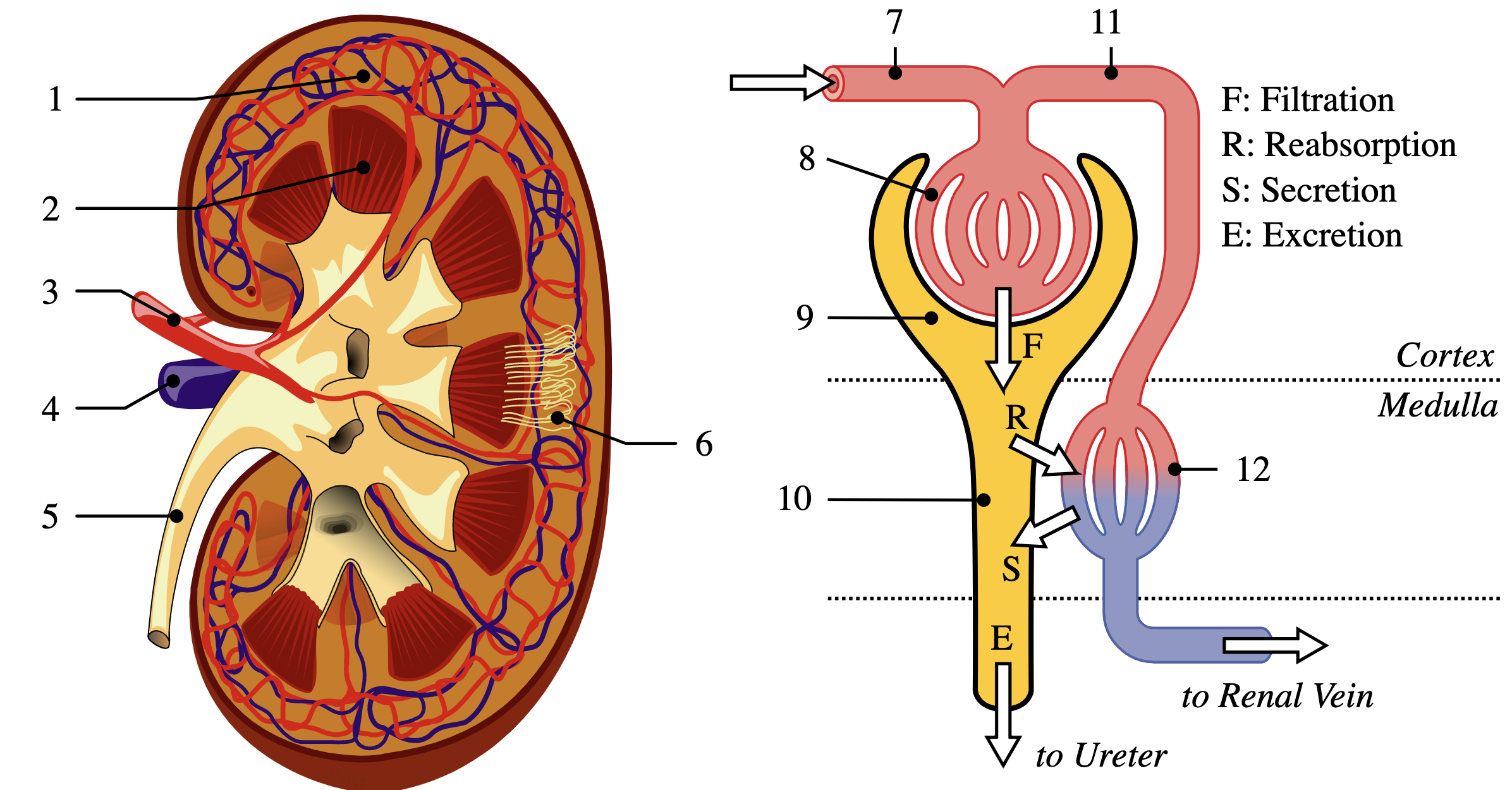
The glomerulus is the filtering element of the nephron, the functional unit of the kidney. It is a complex structure of capillaries supported by a matrix known as mesangium which filters solutes across concentration gradients. Solutes pass from the glomerulus through epithelial cells known as podocytes into Bowman’s capsule and the urinary renal tubules.
Glomerulonephritis refers to disease states caused by inflammation of the glomerulus via cellular or immune-complex mediated mechanisms, leading to impairment in the filtration ability of the glomerulus. Glomerulonephritis be further subdivided into nephritic and nephrotic syndromes as well as rapidly progressive and chronic glomerulonephritis based on clinical presentations, laboratory studies and, definitively, by kidney biopsy; from the perspective of emergency medicine, it is most useful to consider nephritic and nephrotic syndromes. [1]
Nephritic Syndromes
| Name | Demographics | Signs / Symptoms |
|---|---|---|
| IgA Nephropathy | Children post-URI, young adults | Flank pain, gross hematuria, edema |
| Post-streptococcal GN/Infection related GN | Children post-URI, cellulitis | Flank pain, hematuria, edema; preceding-infection |
| Henoch-Schonlein purpura | Childhood vasculitis | Palpable purpura, abdominal pain, arthritis |
| Hemolytic Uremic Syndrome | Childhood with e. coli | Diarrhea, hematuria, renal failure |
| Lupus nephritis | Adults, women>men | Hematuria, edema, HTN, many systemic symptoms |
| Membranoproliferative GN | Children and young adults typically, less well defined | Nephritic to nephrotic, asymptomatic renal disease |
| ANCA-Vasculitis | Adults | Pulmonary involvement, nervous involvement, ulcers |
Nephritic syndromes are characterized by inflammation of the glomerular basement membranes, leading to passage of both red blood cells and protein into urine. Hematuria is specific to nephritis (in contrast to nephrotic syndromes). Clinically, patients present with acute onset of hematuria, sub-nephrotic levels of proteinuria (defined as <3.5 g/day), hypertension, azotemia, and edema. There are a variety of classified nephritic syndromes. Some of them are fairly well characterized, such as HUS, which typically results from Shiga toxin producing Escheria coli infection in children that creates autoantibodies leading to nephritic syndrome.[2] Others, such as membranoproliferative glomerulonephritis, are characterized primarily by kidney biopsy findings of mesangial cell proliferation and can clinically produce a spectrum of disease ranging from nephritic to nephrotic syndrome with a variety of associations including hepatitis and HIV. [3] Ultimately, evidence of nephritic syndromes should prompt urgent Nephrology consultation as a firm diagnosis of the specific type is not typically made in the emergency department, although several syndromes have historical clues which may raise suspicion.[4]
Nephrotic Syndromes
| Primary Causes | ||
|---|---|---|
| Focal Segmental glomerulosclerosis | Minimal change disease | |
| Membranous glomerular disease | Membranoproliferative disease (IgA nephropathy) |
Nephrotic syndrome, or nephropathy, refers to damage to the glomerulus which leads to increased passage of large molecules such as albumin and other proteins through the glomerulus into urine, likely through defects in the podocyte membrane. Clinically, this results in new onset of edema in the lower extremities and potentially in the abdomen, genitals, lungs, and periorbital region. Symptoms additionally include foamy urine and exertional dyspnea. Nephrotic syndromes are rare effecting approximately 3/100,000 adults and 2-7/100,000 children per year.[5,6] Diagnostic criteria include and require all except hyperlipidemia: proteinuria(>3.5g/24h), hypoalbuminemia (<2.5 g/dL), clinically evident peripheral edema, hyperlipidemia (total cholesterol >350 mg/dL).[7] Causes of nephrotic syndrome can be divided into primary, referring to an insult originating within the glomeruli defined on renal biopsy, or secondary, glomerular injury resulting from a systemic disease such as diabetes or systemic lupus erythematosus.
| Secondary Causes | ||
|---|---|---|
| Immunologic | SLE, EM, HSP, PAN, Sarcoidosis | |
| Oncologic | Myeloma, lymphoma, myeloma | |
| Metabolic | Diabetes mellitus, amyloidosis | |
| Drugs | Gold, NSAIDs, Lithium, antibiotics, heroin | |
| Infectious | HIV, hepatitis, syphilis, | |
| Congenital | Alport’s syndrome, Pierson’s syndrome, etc.. | |
| Other | Malignant HTN, preeclampsia |
Management of the glomerulonephritides in the emergency department should consist of symptomatic management, consideration of steroids in consultation with nephrology, and evaluation for complications. Due to loss of immune-mediating molecules in nephrotic syndrome among other proposed etiologies, infectious comorbidities are more likely in these patients including bacteremia, cellulitis, pneumonia, and peritonitis. Children with nephrotic syndrome are at risk for bacterial peritonitis from streptococcus pneumoniae and should be given the 23-valent pneumococcal vaccine.[8] Thromboembolic disease is another serious complication of nephrotic and, to a lesser degree, nephritic syndromes, presenting in 25 % of adult patients and 3 % of children with nephrotic syndrome. Careful consideration should be given to PE, DVT, and renal vein thrombosis, which may warrant evaluation in the ED.[9]
Acute renal failure is uncommon in nephrotic syndrome and when it exists, other causes (such as iatrogenic/medications, renal vein thrombosis, pyelonephritis, SLE) should be investigated.[10] Intravascular and total body volume derangements are common and may co-exist. For patients with signs of hypovolemia (e.g. tachycardia, hypotension, dry mucous membranes, abdominal pain in children) and hypoalbuminemia, consider albumin infusion in consultation with nephrology (typically 0.5-1 g/kg). Hypertension, most commonly seen in nephritic syndromes, should be managed medically as this may help limit further renal damage. Pulmonary edema is a common finding and evaluation with X-ray imaging should be considered. [11]
Ultimately, definitive diagnosis of glomerulonephritis caused by primary renal disease can be made only after renal biopsy. Emergency physicians should maintain a high index of suspicion for glomerular disease, especially in older adults with multiple comorbidities that may cloud the diagnosis. Patients who are likely to have glomerulonephritis should be admitted for further management as delay in care can lead to significant morbidity. Patients with isolated hematuria without renal impairment, significant volume derangement, or other concerning symptoms could be considered for close outpatient follow-up with nephrology.
Post by jeremy Sobocinski, mD
Dr. Sobocinski is a PGY-1 in Emergency Medicine at the University of Cincinnati
Editing and peer review by Brandon Berger, MD and Ryan LaFollette, MD
Dr. Berger is a PGY-4 in Emergency Medicine at the University of Cincinnati pursuing a fellowship in Wilderness Medicine. Dr. LaFollette is an Associate Professor of Emergency Medicine and Co-Editor of TamingtheSRU.com
References
Pavenstädt H; Kriz W; Kretzler M (2003). "Cell biology of the glomerular podocyte". Physiological Reviews. 83 (1): 253–307. doi:10.1152/physrev.00020.2002. PMID 12506131
HUS and atypical HUS. T.S. Jokiranta. Blood. 2017 May 25; 129(21): 2847-2856.
Membranoproliferative glomerulonephritis. B. Alchi; D. Jayne. Pediatr Nephrol. 2010 Aug; 25(8) 1409-1418.
Nephritic Syndrome. P. Lamba MD; K.H. Nam, MD; J. Contractor, MD; A. Kim, MD. Primary Care: Clinics in Office Practice. 2020 Dec. 47 (4) 615-629.
Diagnosis and Management of Nephrotic Syndrome in Adults. Charles Kodner, MD. University of Louisville School of Medicine, Louisville, Kentucky. Am Fam Physician. 2016 Mar 15;93(6):479-485.
Nephrotic Syndrome. T.P. Andolino, MD. J Reid-Adam, MD. Pediatrics In Review. (2015) 36 (3): 117-126
Nephrotic Syndrome in Adults. Richard P Hull; David JA Goldsmith. BMJ. 2008 May 24; 336(7654): 1185-1189. Doi: 10.1136/bmj.39576.709711.80
Complications of nephrotic syndrome. S.J. Park, MD; J Shin, MD. Korean J. Pediatrics. 2011 Aug; 54(8): 322-328
Epidemiology and Pathophysiology of Nephrotic Syndrome-Associated Thromboembolic Disease. B.A. Kerlin; R. Ayoob; W.E. Smoyr. Clin J Am Society of Nephrol. Vol 7: 513-520.
Koomans HA. Pathophysiology of acute renal failure in idiopathic nephrotic syndrome. Nephrol Dial Transplant. 2001;16(2)221-224.
Cline, David, et al. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. McGraw-Hill Education, 2020.