Diagnostics and Therapeutics: Thoracentesis in the Emergency Department
/Shortness of breath is one of the most common complaints presenting to emergency departments. Although the etiology is varied, in this post we will examine one specific cause – pleural effusions – in addition to management of pleural effusions with the thoracentesis procedure.
Overview - what is a pleural effusion and how can i fix it?
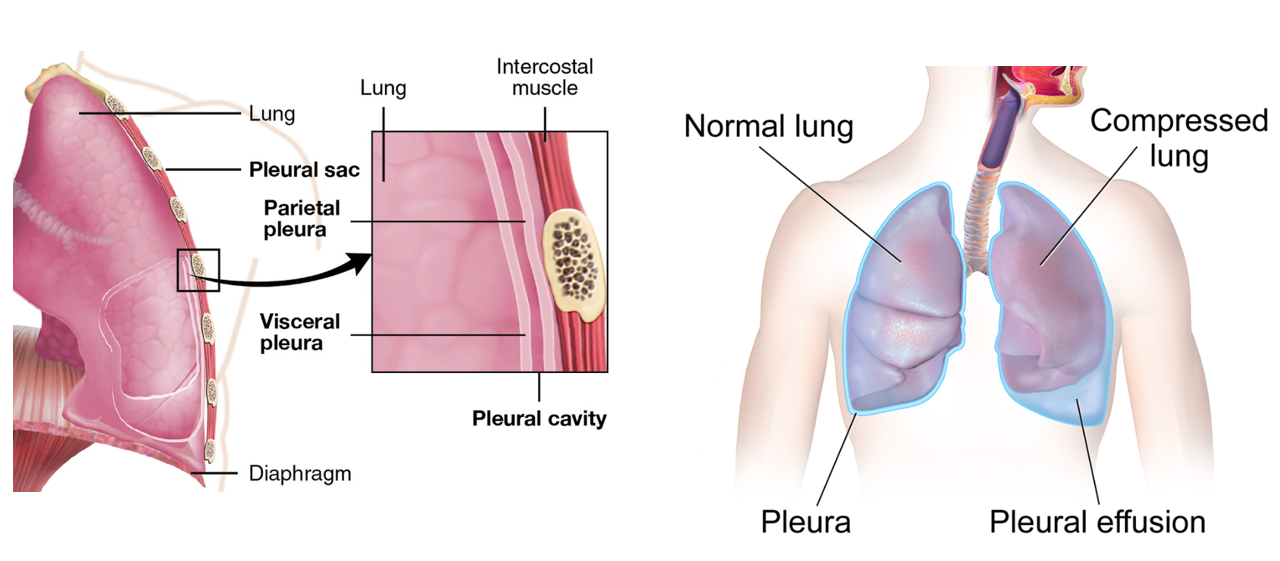
The pleural cavity is a potential space between the lung and chest wall. Within this cavity there is trace fluid (10-20 mL) that serves as a lubricant between the lung and musculoskeletal structures during inhalation and exhalation. An excess of fluid within this cavity - a pleural effusion - is pathologic. The volume of fluid, the rate of accumulation, and the cellular and chemical content or composition are used to guide the differential diagnosis and management of the underlying pathology (1).
Many pleural effusions will be small and have minimal symptoms such as mild shortness of breath on exertion or pleuritic chest pain on the side of the effusion. Diagnosis can be made clinically from decreased lung sounds on auscultation or dullness to percussion, but the most common way to diagnose is via chest x-ray. Lateral views are important for diagnosing small effusions, as AP views will usually only catch effusions with volumes > 175 mL (1,2). Ultrasound in recent years has become a very helpful tool in diagnosing smaller effusions, and is noted to be almost 100% sensitive for effusions > 100 mL (2).
Xrays and ultrasound may be helpful in diagnosing small pleural effusions to identify the cause of a patient’s symptoms, however these patients are often stable and may end up being discharged for outpatient management. A less common but more emergent scenario is the presentation of a patient to the emergency department with a large pleural effusion causing hypoxia and respiratory distress. This patient population will likely have large effusions easily seen on portable chest x-ray.
The drainage of these pleural effusions is performed through a procedure called a thoracentesis. This procedure may be done for diagnostic or therapeutic reasons, although performance for diagnostic reasons in the emergency department is rare. A therapeutic thoracentesis may be indicated in the emergency department for a patient with significant symptoms attributed to a pleural effusion such as dyspnea, hypoxia, or respiratory distress.
Diagnostic thoracentesis involves removal of a small volume (single 20 cc to 60 cc syringe) and sending the sample for laboratory, pathology, and/or cytology analysis. Therapeutic thoracentesis, on the other hand, often removes a few hundred mL up to multiple liters of fluid. Generally, patients can start to feel symptomatic improvement with removal of as little as 400-500 mL. In the case of a therapeutic thoracentesis, a sample is only sent to the laboratory for analysis when there is a question of a change in the etiology of the known chronic effusion such as new malignancy, new infection, or decompensation of a chronic condition (1,2).
If the volume of fluid is anticipated to re-accumulate quickly, a drain should be placed. This often is seen in trauma, cancer, post-operatively, and end-stage metabolic conditions with excessive colloid or protein leak.
contraindications to thoracentesis
There are several (relative) contraindications to consider for thoracentesis including any condition that prohibits safe positioning of the patient, thrombocytopenia (<50K) and uncontrolled coagulopathy (INR >1.5), cellulitis or herpes zoster overlying the site of insertion, uncontrollable or persistent coughing, or an agitated and uncooperative patient (as these conditions may lead to inadvertent damage of underlying vascular structures and lung parenchyma) (3).
While consensus guidelines have traditionally considered thrombocytopenia (platelets <50K) and coagulopathy (INR >1.5) as absolute contraindications to thoracentesis, this has not been supported by recent studies (3). Several prospective studies have not found an association between laboratory parameters (including INR >1.5 or PLT <50K) and bleeding risk, and routine correction of thrombocytopenia or coagulopathy prior to the procedure does not seem to mitigate bleeding risk. However, there are no randomized controlled trials surrounding this topic, so a proceduralist should use their best clinical judgment surrounding bleeding risks (3).
Additionally, caution should be taken in patients who are mechanically ventilated. The positive pressure may increase lung volumes and thus may increase risk of pneumothorax; however, if the size of the pleural effusion is thought to be the main reason the patient has respiratory distress and is requiring mechanical ventilation, then one should proceed with caution under ultrasound guidance (3).
complications of thoracentesis
Iatrogenic pneumothorax is the most common complication of a thoracentesis (3). While historically reported rates were ~20%, more recent literature with ultrasound guidance suggests much lower rates of ~3% (3, 4). The risk of pneumothorax is increased with multiple needle passes, drainage of large volumes of fluid (>1.5L), or when the patient is underweight (BMI <18) (3).
Of note, air in the pleural space following the procedure can also rarely be caused by negative pleural pressures against a lung that cannot fully re-expand (such as when there is fibrosis along the pleura from chronic inflammation), leading to a transpleural air gradient and the replacement of the drained effusion with air, termed pneumothorax ex vacuo (5). This can be differentiated from traumatic lung puncture as the collection of air will not expand or worsen on interval imaging.
Bleeding- including puncture site bleeding, chest wall hematoma, or hemothorax- occurs at a rate of 1-4% (3). Taking care to insert the needle directly over the rib of the intended intercostal space helps reduce the risk of hitting the intercostal vasculature which lies just inferior to each rib. Ultrasound can be used to evaluate for the location of vasculature in the intercostal space, as it can be more variable closer to the spine.
Inadvertent puncture of the diaphragm or abdominal organs can also occur. Choosing a site no lower than the 8-9th ribs helps minimize risk of abdominal injury (3).
Removal of >1L of fluid has been associated with complications such as re-expansion pulmonary edema (3,6,7). This is defined by new alveolar infiltrates and hypoxia within 24 hours of pleural drainage. Re-expansion pulmonary edema is thought to be related to increased pulmonary capillary permeability and microvascular injury due to negative intrapleural pressures and hydrostatic forces from lung re-expansion. While many patients have signs of pulmonary edema on CXR after lung re-expansion, this is often of little clinical significance unless the patient has persistent or worsening symptoms.
Fluid drainage should stop if the patient develops chest pain, dyspnea, or hypotension. Coughing is expected with lung re-expansion (5). Removing large volumes of fluid >500 mL can be associated with vasovagal symptoms.
The procedure itself
Equipment:
Local anesthetic (10 mL of 1% lidocaine)
Needles/syringes
o 25-gauge
o 20- to 22-gauge needles
o 10-mL syringe
o 30- to 50-mL syringe
Antiseptic solution with applicators, drapes, and gloves
Thoracentesis needle and plastic catheter
3-way stopcock
Wound dressing materials
Bedside table for patient to lean on
Appropriate containers for collection of fluid for laboratory tests
Collection bags (for large volume therapeutic thoracentesis)
Ultrasound machine (and sterile probe covers)
Patient Positioning
Ideally, the patient should be sitting upright leaning over a bedside table to allow for fluid to collect dependently, increasing the margin of safety between the effusion and the lung and diaphragm. However, if upright positioning is not feasible, the procedure can be performed with the patient supine with the arm raised over the head.
Procedural Steps (9):
Confirm the extent of the pleural effusion using bedside ultrasound which reduces the risk of pneumothorax and increases the success rate. A curvilinear probe is the optimal choice for this procedure and placed on the patient’s back or axilla in the sagittal position (8). The lung is echogenic and moves with respiration. Find the deepest fluid pocket superficial to the lung.
Select a needle insertion point in the mid-scapular line at the upper border of the rib one intercostal space below the top of the effusion.
The patient should be ideally positioned sitting upright and leaning over a bedside table to allow for fluid to collect dependently. If the patient cannot tolerate being upright, the supine or lateral decubitus position can be used with the dependent side down.
Mark the insertion point, cleanse the skin with chlorhexidine and apply a sterile drape while wearing sterile gloves.
Numb the patient - using a 25-gauge needle, make a wheal with lidocaine over the insertion point. Switch to a larger (20- or 22-gauge) needle and inject anesthetic progressively deeper until reaching the parietal pleura. Continue advancing the needle until pleural fluid is aspirated and note the depth. It is important to infiltrate the parietal pleura with anesthetic because it is the most sensitive part of the procedure for the patient.
The anesthetic syringe can simply be switched to a larger empty syringe or an alternative needle/syringe setup can be used. Ideally a thoracentesis needle-catheter device is used. However, an 18-20 g safety needle (non-angiocath) or spinal needle with a 3-way stopcock can also be used.
If performing therapeutic thoracentesis, place a 60-mL syringe on one port of the stopcock and attach drainage tubing and a collection bag to the other port. If only performing a diagnostic thoracentesis, attach a 20-60 mL syringe directly to the needle.
Drain the effusion - insert the needle along the upper border of the rib while aspirating and advance it into the effusion.
When fluid or blood is aspirated, insert the catheter over the needle into the pleural space and withdraw the needle, leaving the catheter in the pleural space. While preparing to insert the catheter, cover the needle opening during inspiration to prevent entry of air into the pleural space.
Withdraw at least 20-30 mL of fluid into the syringe and place in appropriate containers for laboratory/pathology.
For larger volumes, turn the stopcock and allow fluid to drain into a collection bag or bottle.
Remove the catheter while the patient is holding breath or expiring.
Apply a sterile dressing to the insertion site.
Diagnostics
In terms of etiology, pleural effusions are often divided into two categories – transudative and exudative (10). Transudative effusions are due to increased capillary hydrostatic pressure (e.g., congestive heart failure) or decreased plasma oncotic pressure (e.g., hypoalbuminemia). (2, 10). Alternatively, exudative fluid forms due to increased permeability of the pleural surfaces when tissues are inflamed or damaged (2). Being able to categorize the type of effusion is helpful for quick and rapid therapeutic interventions in sick or unstable patients with unknown effusion etiology.
Common causes of transudative effusions include hypoalbuminemia (cirrhosis, nephrotic syndrome), congestive heart failure, and constrictive pericarditis. Common causes of exudative effusions include infection (TB, parapneumonic, empyema), malignancy, pancreatitis, autoimmune disease, esophageal rupture, hemothorax, chylothorax (2,10).
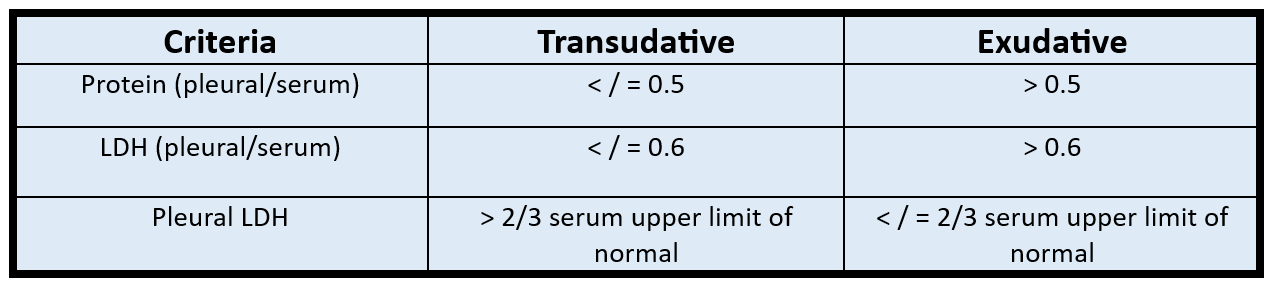
Lights criteria is a diagnostic tool that examines pleural-to-serum fluid protein and LDH ratios to classify the effusion as transudative or exudative (11). As exudative fluids are generally due to inflammation and protein leakage, the relative protein level will be elevated compared to a transudative effusion. LDH is a marker of cellular inflammation and damage and is therefore elevated in pleural fluid with exudative effusions. If pleural fluid meets any of the 3 Light’s criteria (pleural:serum fluid protein ratio >0.5, pleural:serum LDH >0.6, or LDH >2/3 serum upper limit of normal) it is considered an exudative effusion, with a sensitivity of ~97% but a specificity of only ~80% (11). Of note, diuretics can cause falsely positive Light’s criteria.
Lights Criteria
Of note, Light’s criteria is sensitive but not specific for an exudative effusion. Pleural fluid cholesterol has up to 97% sensitivity and up to 100% specificity for an exudative effusion (12).
In general, the diagnostic testing that should be ordered for all thoracenteses includes a cell count and differential, Gram stain, culture, pleural fluid LDH and protein, pleural fluid cholesterol.
post by charlene kotei, md
Dr Kotei is a PGY-1 in Emergency Medicine at the University of Cincinnati.
editing by justine milligan, md and anita goel, md
Dr Milligan is a PGY-4 in Emergency Medicine at the University of Cincinnati with plans to complete an ultrasound fellowship next year, also at the University of Cincinnati.
Dr Goel is an Adjunct Assistant Professor in Emergency Medicine at the University of Cincinnati and an Assistant Editor of TamingtheSRU.
references
Wiederhold BD, Amr O, Modi P, et al. Thoracentesis. [Updated 2023 Jan 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441866/
Beaudoin S, Gonzalez AV. Evaluation of the patient with pleural effusion. CMAJ. 2018;190(10):E291-E295. doi:10.1503/cmaj.170420
Cantey EP, Walter JM, Corbridge T, Barsuk JH. Complications of thoracentesis: incidence, risk factors, and strategies for prevention. Curr Opin Pulm Med. 2016;22(4):378-385. doi:10.1097/MCP.0000000000000285
Cavanna L, Mordenti P, Bertè R. Ultrasound guidance reduces pneumothorax rate and improves safety of thoracentesis in malignant pleural effusion: report on 445 consecutive patients with advanced cancer. World journal of surgical oncology. 12:139. 2014.
Staes W, Funaki B. "Ex vacuo" pneumothorax. Semin Intervent Radiol. 2009 Mar;26(1):82-5. doi: 10.1055/s-0029-1208386. PMID: 21326535; PMCID: PMC3036450.
Feller-Kopman D, Berkowitz D, Boiselle P, Ernst A. Large-volume thoracentesis and the risk of reexpansion pulmonary edema. Ann Thorac Surg. 2007;84(5):1656-1661. doi:10.1016/j.athoracsur.2007.06.038
Walter, James M et al. "Acute Hypoxemic Respiratory Failure after Large-Volume Thoracentesis. Mechanism of Pleural Fluid Formation and Reexpansion Pulmonary Edema." Annals of the American Thoracic Society, vol. 13, issue 3, March 2016, p 305-450. https://doi.org/10.1513/AnnalsATS.201510-716CC. Accessed 21 May 2024.
Soni NJ, Franco R, Velez MI, Schnobrich D, Dancel R, Restrepo MI, et al. Ultrasound in the diagnosis and management of pleural effusions. J Hosp Med. 2015 Dec. 10 (12):811-6.
Dezube R. How to do thoracentesis - pulmonary disorders. Merck Manual Professional Edition. Accessed May 15, 2024. https://www.merckmanuals.com/professional/pulmonary-disorders/how-to-do-pulmonary-procedures/how-to-do-thoracentesis.
Yu H. (2011). Management of pleural effusion, empyema, and lung abscess. Seminars in interventional radiology,28(1), 75–86. doi:10.1055/s-0031-1273942
Light RW. Clinical practice. Pleural effusion. N Engl J Med. 2002 Jun 20;346(25):1971-7. doi: 10.1056/NEJMcp010731. PMID: 12075059.
Hamal AB, Yogi KN, Bam N, Das SK, Karn R. Pleural fluid cholesterol in differentiating exudative and transudative pleural effusion. Pulm Med. 2013;2013:135036. doi: 10.1155/2013/135036. Epub 2013 Jan 10. PMID: 23365740; PMCID: PMC3556870.