Grands Rounds Summary 01.25.2017
/Morbidity and Mortality with Dr. Betham
Cases #1 & #2: Lets talk about Gout
How good are physicians at the diagnosis of gout by history & physical?
Sensitivity of H&P for gout was good, but not very specific. 119/324 patients called gout but after arthrocentesis were diagnosed with something else.
What does serum uric acid mean in the diagnosis of gout?
There is no correlation to acute gout flares. Serum uric acid may actually go down during acute gout flares.
Case #3: ITP with ICH
Risk of head bleeds in Adults with ITP: Acute 0.6% Chronic 1.8%, Overall risk is 1.5%
Risk of head bleeds in kids with ITP: Total 0.5%
Platelet count to be concerned about: <30 more likely to bleed, need >10 to maintain normal intravascular hemostasis, recommendations vary for hard transfusion cut-off, but < 10 requires tranfusion.
Increased ICH risk: Chronic ITP or a rapid fall in platelets
Headache red flags and risk factors:
- Anticoagulation, clotting disorders, thrombocytopenia
- Sudden onset
- Severity of headache
- Immunocompromised
Beware headache +
- Vision changes
- Weakness
- Dizziness
- Sensation changes
Case #5: R MCA Stroke in an HIV+ patient
Beware of the barriers to care:
- Language barriers
- Antagonistic/anxious family
- Stigma of certain diseases (HIV, for example)
- Co-morbidities: HIV/AIDs brought many things into the DDx that would not have been there otherwise
- Waxing and waning presentation
Is this a stroke?
- New, abrupt onset of neurological deficit
- Stroke, stroke, stroke,
- Seizure
- Spinal cord pathology
- Infection unlikely
- Get the last known well time
- Call the stroke team if within 12 hours of onset
- Get POC glucose
tPA?
- Acute onset within 3 (or 4.5 hours in certain patients)
- Negative head CT
- Debilitating deficit (NIH ~6)
- No contraindications (tamingthesru.com)
tPA Contraindications
- Significant head trauma or stroke within 3 months
- Symptoms suggest SAH
- Arterial puncture at non-compressible site within 7 days
- Any prior ICH
- Intracranial neoplasm, AVM, or aneurysm
- Recent intracranial or intraspinal surgery
- Elevated BP (SBP >185 or diastolic >110)
- Active internal bleeding
- Acute bleeding diathesis
- Platelet count <100,000
- Heparin within 48h with aPTT greater than the upper limit of normal
- Current use of anticoagulant with INR >1.7 or PT>15 sec
- Use of direct thrombin inhibitors or direct factor Xa inhibitors with elevated sensitive laboratory tests
- Blood glucose <50 mg/dL
- CT demonstrates multi lobar infarction
- Large vessel occlusion amenable to angio
- Protocol: any acute stroke within 12 hours onset
- Not to rule out stroke
- tPA decisions are made independent of CTA findings
HIV in ischemic stroke
- HIV infection Hazard Ratio 1.17
- HIV + CD4 <200 Hazard Ratio 1.66
- HIV + RNA >500 Hazard Ratio 1.36
Case #6: Hyperkalemia in ESRD
Can you hang your hat on EKG changes?
- 74 patients with ESRD, immediately before dialysis they tested both K and EKGs--> none of the patients had EKG changes no matter what their K was
- The concept that the first sign of hyperK can be a lethal arrhythmia comes from a study in the 1950s where they fed patients huge amounts of K and then watched their EKGs. Some of them didn't do well...
Does CKD protect you from hyperkalemia?
- The higher your stage of CKD, the lower OR of death with hyperK, no matter what level of hyperK you have
Good news:
- Slower rate of rise is probably less dangerous
- Lower mortality with higher CKD stage
- Adaptations in renal failure
- New steady state K
- Increased gut secretion
Bad News
- Less likely to show EKG changes
- Less reserve for increased potassium intake
- Heart failure patients are more prone to cardiotoxic effects
- Chronic hyperkalemia often means non-compliance
Adherence barriers to chronic dialysis:
- GI Upset
- Drug or alcohol abuse
- Chronic pain
- Transportation van as mode of transportation
- >17min to dialysis clinic
- >1.5 inches of snow
- Holidays
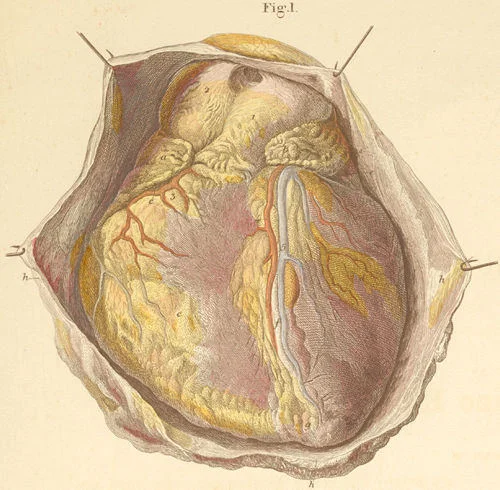
Taming the SRU with Dr. Teuber - ED Thoracotomy (EDT)
Procedure done in the ED to open the chest to control hemorrhage both intra-thoracic and extra-thoracic
Who Should Get an EDT?
- EAST (eastern association surgery of trauma)
- Penetrating thoracic injury
- Signs of life-- strongly recommended
- No signs of life-- conditionally recommended
- Penetrating extra-thoracic injury
- Signs of life-- conditionally recommended
- No signs of life-- conditionally recommended
- Blunt Injury
- With signs of life-- conditionally recommended
- No signs of life-- conditionally recommend AGAINST EDT
- Penetrating thoracic injury
- WTA (western trauma association)
- Penetrating torso injury
- <15 min pre-hospital CPR
- Penetrating neck or extremity injury
- <5min pre-hospital CPR
- Blunt Trauma
- <10min pre-hospital CPR
- Refractory Shock
- SBP <70
- Penetrating torso injury
- ACEP Recommendations for EDT
- Strongly recommends
- Pulseless in ED with signs of life after penetrating thoracic injury (21% survival 90% neuro intact)
- Conditionally recommends
- Pulseless in ED without signs of life after penetrating thoracic injury (8% survival, 4% neuro intact)
- Pulseless in ED with signs of life after penetrating extra-thoracic injury (15% survival, 16% neuro intact)
- Pulseless in ED without signs of life after penetrating extra-thoracic injury (3% survival, 0.05% neuro intact)
- Pulseless in ED with signs of life after blunt injury (4.6% survival, 2% neuro intact)
- Conditionally recommends AGAINST
- Pulseless in ED without signs of life after blunt injury (0.7% survival, 0.1% neuro intact)
- Strongly recommends
Contraindications for EDT
- Blunt trauma without witnessed cardiac arrest
- Penetrating abdominal trauma without cardiac activity
- Penetrating thoracic trauma without pericardial effusion + lack of cardiac activity
- Non-traumatic cardiac arrest
- Severe head injury
- Severe multi-system injury
- Improperly trained staff
- Insufficient equipment
Increased survival chances
- Signs of life in the ED
- Pupillary response
- Spontaneous ventilation
- Carotid pulse
- Measurable BP
- Extremity movement
- Organized cardiac activity
- Penetrating Injury
- Stab Wounds
- Thoracic Injury
Ultrasound in EDT
- Prospective study completed 2010-2014
- 187 patients
- Cardiac motion: 100% sensitive 73.7% specific to ID survivors/organ donors
Pediatric guidelines read that EDT may benefit pediatric trauma patients
How to do an EDT:
- IV, O2, monitor
- Patient supine, elevated L arm
- Incise through skin and subcutaneous tissue along the 5th rib laterally
- Divide muscle and pleura with scissors using blunt dissection
- Insert rib spreader retractor
- May need to extend to the right side, cut through sternum with bone cutters or gigli saw
- If tampanode is suspected: complete pericardiotomy first then clamp aorta
- If tamanode is not suspected: cross clamp the aorta first, then complete pericardiotomy
- Clamp the aorta
- Hilar clamp
- Internal cardiac massage
- Internal Defibrillation
- Start with 20-30J
- Avoid coronary arteries
Pearls
- Surgical Consult Immediately
- Use L anterolateral approach if site of injury is unknown and patient requires immediate intervention
- Rib spreaders-- handle down-- in order to allow you to convert to bilateral clamshell if needed
- 90 seconds maximum to get into the pericardium
- Place NGT to help distinguish between esophagus and aorta
- Consider selective R mainstem intubation
- 2 hands for internal massage
- Similar outcomes in adult and pediatric patients
- Ultrasound has become a mainstay in EDT
- Don't forget: bicarb, calcium, blood products, TXA
- Ligate the mammary arteries once ROSC
Complications
- 50% of survivors suffer from anoxic brain injury
- Recurrent bleeding from chest wall
- Damage to coronary arteries
- Damage to esophagus
- Damage to phrenic nerve
- Organ ischemia/spinal cord ischemia due to aortic cross clamping
- Large risk for self injury to medical staff
R1 Knowledge Lecture WITH DR. BANNING: Neonatal ED visits
Most common PED neonatal visits:
- Jaundice
- Irritability
- Vomiting
- Rash
Most common diagnoses:
- Normal neonate
- Physiologic jaundice
- Colic
Factors contribution to non-acute presentations:
- First child
- Young mothers (<25yo)
- <14do
Chief Complaint #1: Jaundice
Three mechanisms of jaundice
- Catabolism of RBCs
- Unconjugated bilirubin
- Conjugated bilirubin
Physiologic Jaundice
- Breastfeeding Jaundice: 3rd-4th day of life, caloric deprivation
- Breast Milk Jaundice: 4th-7th day of life, breast milk inhibits B-UGT
Pathologic Jaundice
- Jaundice within 24h
- Total serum bilirubin >17
- Evidence of underlying disease
- Conjugated bilirubin >20% of total serum bili
Starting point:
- Indirect + direct bilirubin
- CBC
- Hydration status, neurologic status, weight loss, signs of birth loss
- UA? (not in typical practice)
Abnormal Results
- Coomb's test
- Mom/baby blood type
- Retic count/peripheral smear
- Sepsis workup, TSH, abdominal US
Pearls:
- Don't try to predict bilirubin on exam
- Bilitool.org
- Start lights as soon as possible
- No need for exchange transfusion in the ED
- Continue to breast feed
Rashes:
- Erythema toxicum neonatorum: normal rash, macules with an erythematous base on the trunk that resolves in 5-7 days
- Transient neonatal pustular melanosis: 20% of babies non-caucasian babies, pustule with an underlying hyperpigmented macule
- Miliaria: result of overbundling, blockage of the ecrin glands, don't overheat
- Neonatal HSV: vesicles that are coalesced in one area over an erythematous base, sepsis work-up with viral PCR
Chief Complaint #2: Crying
Normal Crying Patterns:
- Typical newborn may cry for 2 hours per day
- Crying begins to increase around 2 wks and peaks around 6 wks old
- Younger than 3 months have higher frequency of crying
- Worse in the afternoons or evenings
Causes of Crying:
- Go with symptoms
- Make sure to rule out anal fissures, drug withdrawal, medication exposure in breast milk, hair tourniquet, corneal abrasion
Neonatal eye complaints:
- Corneal abrasion: oral acetaminophen, topical erythromycin TID x3d
- Gonorrhea: 0-5days, IV Cefotaxime with full sepsis work-up
- Chlamydia: 5 days- 5 weeks, oral erythromycin for 2 weeks (get a positive culture first)
- Lacrimal Duct Stenosis: referral after 7-8 months if symptoms persist
Chief Complaint #3: There is ____ colored _____ coming out of my baby's ______.
Vomiting
- 50% of infants under a month have daily emesis
- 12% diagnosis of reflux
- Tx: reassurance, no difference between kids started on PPI in 2 RCTs
- Warning signs: weight loss
- Infants lose 5-10% of birth weight
- Regain birth weight by 2 wks
- Gain 15-30g/day after 2 wks
- Warning signs: projectile emesis, bilious emesis
Poop
- 1 stool/7-10days --> 7-10 stools/day
- Normal for shrieking with pooping
- Constipation is rare but consider hypothyroidism, botulism, hirschprung disease
- Glycerin suppository safe
- Warning signs: acholic stool, bloody stool, PoopMD
- GI Bleed:
- Swallowed maternal blood
- Swallowed blood from nasopharynx/oropharynx
- Coagulopathy
- Vascular malformations
- Anal fissure
- Necrotizing enterocolitis (up to 10% of term babies can get necrotizing enterocolitis, so not just for premies)
- Liver disease
- Post steroids/indomethacin
- Other fluids:
- Vaginal bleeding (normal)
- Galactorrhea (normal in both males and females)
- Urine from umbilicus: Concern for patent urachus (transfer this one for further work-up)
Leadership Curriculum with Drs. Hill, LaFollette, McDonough, stettler and Toth: Pitching an Idea
As physicians, we are constantly presenting our plans and ideas to supervisors, to patients, families. It is a crucial part of academic promotion, but moreover a means of effective communication. We evaluated some of the literature behind an effective pitch, with most of the data coming from Silicon Valley and Hollywood. The uniform principal behind an effective pitch is to be prepared and be practiced. Here are a few tips to preparing your pitch:
- Identify your goal (are you garnering support? time? finances?)
- Identify your target (program director? medical director? chair? who has the influence to further your project?)
- Get their attention (anecdotes draw the audience into a shared experience and goal)
- Understand their perspective (how can this project further their goals as well)
- Do your homework (understand the context - has someone tried this before? what other players/finances will be needed?)
- Sell yourself (your audience needs to come away with the idea you have the ability to follow though)
- Progress logically
- Be positive
The next step - before you enter the conversation, you should have an idea of what you would like the next step to be
- Commitment
- Written Proposal
- A Timeline
- ... or why the pitch failed