Grand Rounds Recap 04.21.21
/
LEADERSHIP CURRICULUM: GENERATIONAL AND GENDER-BASED COMMUNICATION WITH DR. PAULSEN
The workforce is changing
We live longer and work longer
We have more two-income households - 80% of millennials, 47% boomers
Women are not evenly distributed - 20-30s are majority female, 50+ majority male
Key concepts
Stereotype: an over-generalized belief about a particular category of people
Meta-stereotype: an assumption that members of one group have about the way in which they are stereotypically viewed by another group
Potential responses to the above can be to view it as a challenge, a threat, a conflict, or avoidance
Generational communication - values across the ages
International study including over 18000 people [Bresman, 2017]
Similarities - majority of people across generation valued leadership opportunity
Differences - Gen X/Y valued coaching and mentoring while Gen Z valued higher responsibility and more creative freedom/autonomy
This also varied amongst genders - women were more likely to value coaching and mentoring while men valued responsibility and financial independence
A study assessing hiring trends and preferences [McCausland, 2015; Bernstein, 2019; Waldman, 2020]
Older age was viewed as a disadvantage and were assumed to have technologic incompetence and more difficulty learning new skills or information
Knowledge and expertise actually predict job performance, not the ability to learn new skills or information
Younger workers perceive more negative age stereotypes and meta-stereotypes - millennials are stereotyped as narcissistic, unable to take feedback, managing “up” or colleagues that are older than them
Gender-based communication
Talking from 9 to 5 by Deborah Tannen notes that men have a hierarchical structure (challenge is accepted, confidence is praised) whereas women have a communal structure (group harmony and likability is valued and assertiveness is penalized)
Ritual exchange - males tend to “one up” with showing off, teasing, and mock-hostility whereas females tend to “one down” with I’m sorry, diminishing compliments, self-deprecation
“The requirements of a good leader and a good woman are mutually exclusive. A good leader must be tough, but a good woman must not be. A good woman must be self-deprecating, but a good leader must not be.” - Tannen
A study demonstrated that men speak more frequently, speak for more time, and are more likely to get credit whereas women may feel ignored, marginalized, and attacked
An article published by Zimmerman, 2016 in the Atlantic assessed the experience of transwomen in the cross-industry setting comparing before- and after-transition experiences
“Finding my voice as a woman gave me new strength…”
“There’s some things I do the same, but my comfort and confidence is different…”
“Authenticity resonates”
Case-based discussions
Males were more likely to introduce their male colleagues by their official title and female colleagues casually, whereas females were more likely to introduce both genders by their official titles [Files, 2017]
High-stakes conflict (such as AirCare) - disagreements can be due to differences status versus experience and require direct communication and debriefing with the goal to restore a collegial, respectful dynamic
Everyday conflicts (such as calling a consult) - remember we’re all human, seek first to understanding, make it patient-centered first
The contentious debrief - know your audience, pick your battles, do not point fingers, keep calm and remain evidence-based and patient-centered, and defend your team publicly while giving formative feedback privately
Cultural workplace solutions
Create diverse working groups
Emphasize individual strengths among the team
Unite around shared goals and share credit
Be confident enough to be vulnerable
Get comfortable with being uncomfortable
Call out microaggressions
Use neutral language in recruitment
Maintain an open dialogue about shifting needs at various life stages
qi/kt: STATUS EPILEPTICUS WITH DRS. FRANKENFELD & IJAZ
Definitions
Prolonged seizure: single seizure >5mins OR multiple seizures without return to baseline
Status epilepticus (SE): seizure lasting more than 30mins
Refractory SE: failure to control seizures with 1 benzo + 1 AED
Super refractory SE: failure to control seizures 24hours after anesthetic initiation
Operational dimension:
T1 = 5min → seizures are unlikely to resolve spontaneously
T2 = 30min → seizures cause irreversible neuronal damage
Time and seizure subtype:
GTC 5mins
Focal 10mins
Absence 10-15mins
The longer the seizure duration, the higher the mortality
Four axes of defining seizures
Semiology - motor versus consciousness
Etiology
EEG correlates
Age
Epidemiology
10-41 cases/100,000 persons
Mortality of 20%
30d mortality ranges from 3.7-42.8% depending upon the underlying etiology
Etiologies include idiopathic, remote symptomatic, trauma, alcohol-related, drug overdose, low AED levels, metabolic, CNS infection, other infection, tumor, hemorrhage, cerebrovascular disease, hypoxia, or anoxia
Most common are medication noncompliance and cerebrovascular disease
Pathophysiology: Seizures are usually inhibited by GABA-mediated inhibitory pathways. Prolonged seizures can cause a down-regulation of GABA-A receptors causing them to become more resistant to benzodiazepines.
Approach to Evaluation and Management
0-5 minutes
Complete initial evaluation - ABCS, IV, O2, monitor, POC glucose + other labs such as electrolytes, renal panel, LFTs, AED levels, and consider alternative causes
5-20 minutes
RECOMMENDATION:
IV lorazepam 4mg → redose x1 after 3-5min as needed
IM midazolam 10mg → no redosing
IV diazepam 5-10mg → redose x1 after 3-5min as needed
Delay in benzodiazepine administration >10min was associated with increased need for continuous infusions, more hypotension, and longer duration of convulsive SE [Gainza-Lein, 2018]
Randomized comparative trial including patients in overt or EEG confirmed status epilepticus [N=384] receiving IV lorazepam (0.1mg/kg) vs IV diazepam (0.15mg/kg)+ phenytoin (18mg/kg) vs phenobarbital (15mg/kg) + phenytoin (18mg/kg) [Treiman, 1998]
IV lorazepam showed superiority over phenytoin alone, otherwise similar success rates amongst intervention arms
Randomized, double-blinded control trial of pre-hospital adults in SE [N=205] comparing IV lorazepam vs IV diazepam vs IV placebo [Alldredge, NEJM]
SE termination by ED arrival was similar between lorazepam and diazepam groups, both of which were superior to placebo
Patients receiving placebo were more likely to require an airway due to lack of airway protection/hypoxia compared to those receiving benzodiazepines
Multicenter RCT including adults with SE [N=78] comparing IV lorazepam vs IV diazepam
No statistically significant difference in SE termination with a slight trend favoring lorazepam [Leppik, 1983]
Cochrane review of 18 studies, >2700 patients
IV lorazepam > IV diazepam for reducing the risk of seizure continuation (RR 0.64)
IV lorazepam had a lower risk for continuation of SE requiring a different drug or general anesthesia (RR 0.63)
RAMPART Trial: RCT, double-blinded including pre-hospital children and adults with SE [N=893] comparing IM midazolam (5/10mg) vs IV lorazepam (2/4mg) [Silbergleit, NEJM]
Adult arm received IM midazolam 10mg and IV lorazepam 4mg
IM midazolam was non-inferior to IV lorazepam with regards to primary outcome of seizure cessation prior to hospital arrival
Time to administration in IM midazolam group was quicker than IV lorazepam group that likely confounded time to seizure cessation when comparing these two groups
A 2019 study of California EDs demonstrated that lorazepam was frequently under-dosed (23%) as was midazolam (14%) - if you’re going to commit to administering benzodiazepines, give an appropriate dose!
Meta-analysis of 6 studies [N=774] demonstrated that midazolam by any route is as good and sometimes better than diazepam (including buccal midazolam > rectal diazepam). Many of these routes are studied in pediatric studies. [McMullan, 2010]
20-40 minutes
RECOMMENDATION:
IV levetiracetam 60m/kg (max 4500mg)
IV valproate 40mg/kg (max 3000mg) → can redose 20mg/kg if needed (contraindicated in pregnancy and hepatic disease)
IV fosphenytoin 20mg/kg (max 1500mg)
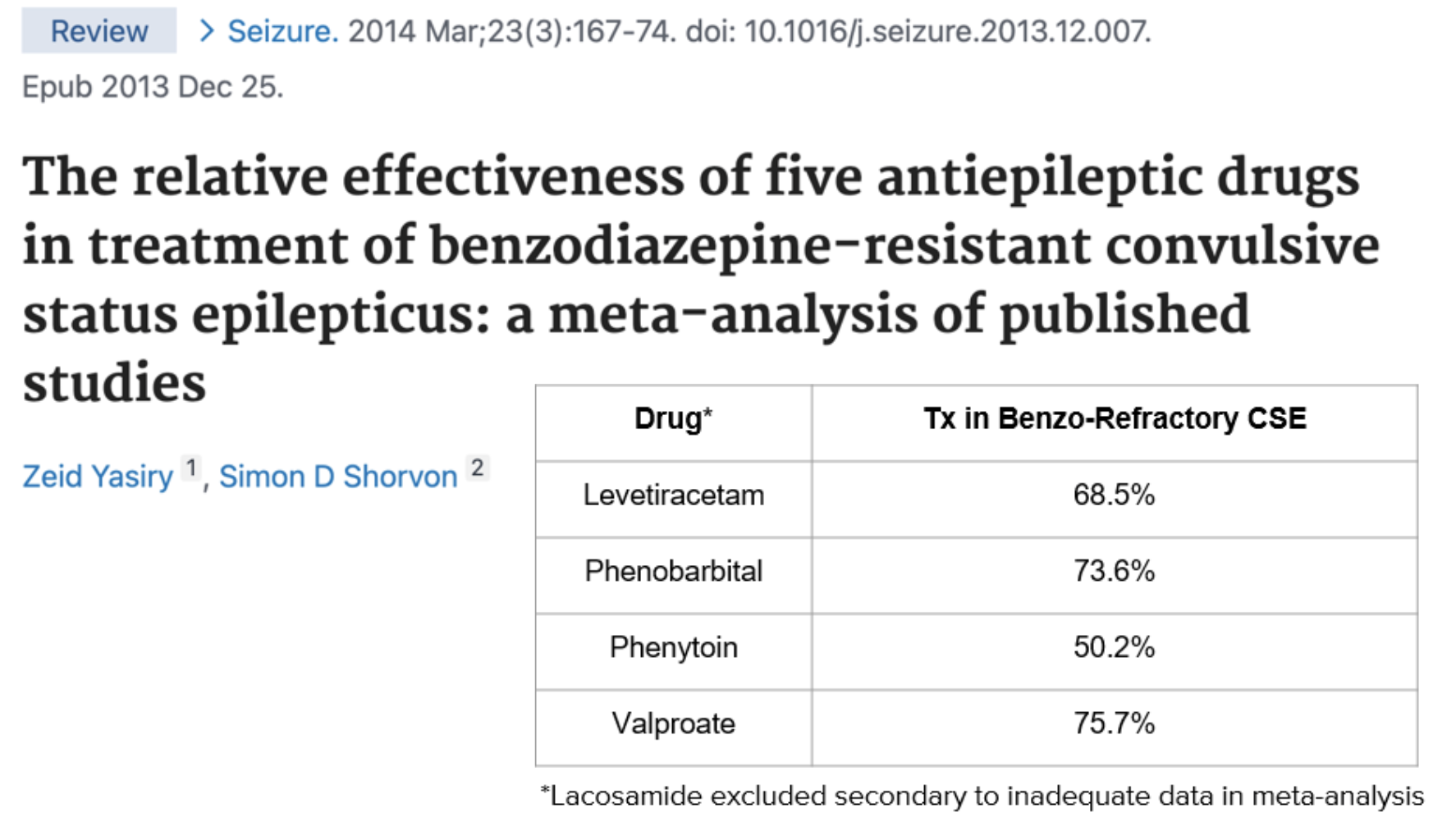
Meta-analysis comparing levetiracetam, phenobarbital, phenytoin, valproate, and lacosamide (only 2 studies) [Yasiry, 2014]
Phenobarbital had the highest success rate in treating benzodiazepine-refractory convulsive SE, however also had the highest rate of intubation as well as need for vasopressors
Phenytoin acts on voltage-gated calcium channel, diluent contains propylene glycol
Complications: injection-site complications (purple glove syndrome) and cardiovascular collapse
Dosing is 18mg/kg → max push rate of 50mg/min
Can only administer in normal saline
Fosphenytoin is the prodrug form of phenytoin without propylene glycol vehicle
Most of the evidence in favor of fosphenytoin is based on a single-dose, double-blinded study showing fosphenytoin was better tolerated at higher infusion rates without similar injection site problems (17% v 2%) and cardiovascular collapse
Dosing 15-20mg/kg fosphenytoin → max rate 150mg/min
Can administer in normal saline and D5W
ESETT Trial: Prospective, comparative, adaptive, double-blind comparative effectiveness trial including children and adults [N=384] with seizures after an adequately dosed benzodiazepine comparing fosphenytoin (20mg/kg) vs valproate (40mg/kg) vs levetiracetam (60mg/kg) [Kapur, NEJM]
No significant differences in primary outcome of absence of clinically significant seizures and increased responsiveness at 60min
Fosphenytoin was associated with more hypotension and intubation rates than the other meds
Brivaracetam and lacosamide may be considered as potential second line agents, however not enough studies to recommend definitively as of yet
40-60 minutes
RECOMMENDATION:
Midazolam bolus 0.2mg/kg + infusion 0.1mg/kg/hr OR
Propofol bolus 1-2mg/kg + infusion 20mcg/kg/min
+ STAT EEG
Oftentimes if seizures persist despite benzodiazepine administration and second line agent, these will only cease ~10% of the time. Refractory SE is considered at this point.
Review article outcome of therapies in refractory and super-refractory convulsive status epilepticus and recommendations for therapy demonstrated:
Randomized control, single blind study among several institutions included patients in refractory SE [N=24] comparing propofol vs barbiturates [Rossetti, 2010]
Caveat is that the study was ultimately terminated early due to lack of recruitment but it did highlight
Similar rates of SE termination between drug groups
The barbiturates group had longer ventilation times compared to the propofol group
Retrospective chart review of adults with acute seizures >2hr or at least 2 seizures/hr [N=20] comparing propofol bolus + infusion vs midazolam bolus + infusion
Propofol and midazolam were equally effective in suppressing refractory SE
Ketamine acts at the NMDA receptor that is upregulated in these states to attenuate risk for seizure at another channel
Large retrospective study demonstrated that ketamine decreased seizure burden in ~50% and led to cessation of seizures in 63% [Alkhachroum, 2020]
Retrospective cohort study over 14 years included patients with refractory SE [N=77] comparing initiation of continuous IV anesthetic drug (CIVAD) before 48 hours vs after 48 hours [Madzar, 2018]
Early use of CIVAD associated with better functional outcome (RR 3.175)
Early use was also associated with lower rates of thiopental use
Data AGAINST IV anesthetic drugs for SE
Marachi (2015) - prospective cohort that demonstrated higher risk for new disability and mortality when treated with CIVAD versus none, and this was replicated in Sutter, 2013 and Kowalski, 2012
When to intubate?
A 2015 review of patients demonstrated that ⅕ patients presenting to the ED for seizures ended up intubated. Mortality is higher in those requiring intubation (probably more to do with the refractoriness of the seizure than the intubation itself). Those with prior seizures or febrile seizures were less likely to be intubated, whereas toxic or metabolic etiologies and CNS seizures were more often intubated. Not a ton of guidance for who to intubate or not, but some considerations [Perier, 2018]
Retrospective single center study included patients with seizures ~60min in the pre-hospital setting comparing etomidate and thiopental as induction agents.
Similar rates of seizure recurrence
>60 minutes
Ketamine 1.5m/gkg bolus q5min PRN (max 5mg/kg) + infusion 0.5-1.5mg/kg/hr
Pentobarbital 5mg/kg bolus q15-30min (max 20mg/kg) + infusion 1mg/kg/hr
Minimal evidence for use of magnesium or lidocaine
Hypothermia for neuroprotection in convulsive status epilepticus?
JAMA article demonstrated there was no 90d mortality difference when inducing hypothermia in comparison to normothermia
Likely no role for hypothermia protocol
attending case follow-up WITH dr. hill
Female in her 70s presenting with shortness of breath. Her watch told her she was in Afib, however she did not follow up with her primary care doctor until 2-3 days later. On arrival to the ED, she was noted to be in Afib.
NEJM 2019 - Large scale assessment of a smartwatch to identify atrial fibrillation (N=>419,000) that demonstrated about 30-40% of patients who had Afib on their watch had Afib on the patch monitor.
The study was not designed to assess the algorithm as a screening tool or to measure sensitivity, specificity, or false positive results. The algorithm was designed to minimize false positive findings and the low incidence of notifications reflects this intent. The algorithm was not designed to detect short episodes of afib, and participates with a low burden of afib could have been missed.
Circulation 2020 - Accuracy of apple watch for detection of Afib: found 292/300, 90 on telemetry
Apple watch notification/display demonstrates sensitivity 41%, specificity 100%; PDF interpretation sensitivity 96%, specificity 100%
JAMA Cardiology - multichannel electrocardiogram obtained by a smartwatch for the diagnosis of ST-segment changes can be used accurately
Approach to Afib with RVR
Stable or unstable?
Unstable? Shock.
Stable?
Primary? Consider in HRs 150s-160s. May need to rate-control once secondary etiology is ruled out.
Secondary? Consider in HRs 120s-130s. Treat the underlying cause.
Timing?
<48hrs? Rhythm control is feasible.
>48hrs? See above and below.
Heart failure?
Decreased EF? Avoid BB or CCB as it can precipitate/exacerbate heart failure. Consider digoxin or amiodarone.
Normal EF?
Convenience sample of adult patients presenting with rapid Afib/Aflutter was randomly assigned to receive either diltiazem or metoprolol [Fromm, 2015]
Mean decrease in HR for diltiazem group was more rapid and substantial than that of the metoprolol group
From a safety perspective, no difference in hypotension or bradycardia between the two groups
Retrospective chart review of patients [N=51] presenting with Afib with RVR who received IV diltiazem or IV metoprolol in the ED.
Primary outcome: sustad rate control defined as HR <100 without need for rescue IV medication for 3h following initial rate control attainment
Secondary outcomes: time to initial rate control, time to oral dose, admission rates, safety outcomes
No difference in sustained rate control, however time to rate control was significantly shorter with diltiazem than metoprolol
No difference in hypotension or bradycardia
Systematic review of two studies [n=92] comparing IV diltiazem with IV metoprolol [Martindale, 2015]
Concluded that diltiazem may be more effective than metoprolol in achieving rapid rate control, but high-quality randomized studies are needed
Case reports outline that use of both BB and CCB can cause heart blocks
Rate versus rhythm control
Cardiac CT has been shown to accurately identify L atrial thrombus and has demonstrated to be as accurate as TEE with sens 94%, spec 99%. Advantage is that it is non-invasive and can be rapidly performed in th eED. May be a method to screen high risk patients for thrombus prior to cardioversion [Christians, 2020]
Early rhythm-control therapy in patients with Afib [Kirchhof, 2020]
Those with early rhythm control had improved first primary outcome, death from cardiovascular causes, stroke, and hospitalization with worsening of heart failure
Future of Afib Management
Dilt drip and admit should die - push more for rhythm control
Arrange partnerships with cardiology for early cardioversion - possible developments of observation protocol
A negative CTPA plus relatively recent onset Afib = cardioversion
Skills acquisition for TEE as EM providers?
Patient was placed on diltiazem gtt + digoxin and admitted overnight. Got cardioverted the next morning after TEE was performed and is doing well!
R1 CLINICAL TREATMENTS: RENAL COLIC WITH DRS. MARTELLA & HUGHES
Epidemiology
12-15% prevalence in the United States
1% of all ED visits are due to renal colic
MOST renal stones will pass spontaneously
Mechanism of pain: increased urinary wall tension and pressure from stone obstruction → stimulates release of prostaglandins → leads to dilation of afferent arterioles → leads to increased diuresis that can then again lead to increased urinary wall tension in a vicious cycle
NSAIDs
Mechanism of action: inhibition of COX-1 and 2 that prevents prostaglandin synthesis and vasodilation, helping to break the pain cycle listed above
Adverse effects: GI side effects and renal toxicity
Cochrane review [2004] included 20 RCTs comparing NSAIDs to opioids in the treatment of renal colic with 19 different reported outcomes
Patients had lower reported pain scores when given NSAIDs as part of therapy
Patients were significantly less likely to require rescue analgesics when they received NSAIDs
More adverse effects in the opioid group (most of whom received meperidine) however could not be pooled given unexpected heterogeneity amongst studies
GI bleeding and renal impairment side effects were not reported
Conclusion: limited applicability to clinical practice given use of meperidine
Cochrane review [2015] included 50 RCTs comparing effectiveness of NSAIDs vs non-opioids (mainly antispasmodics and anticholinergics) for acute renal colic with outcomes include VAS pain scale reduction, 50% reduction in pain, need for rescue analgesics, and pain recurrence
NSAIDs in combination with antispasmodics > NSAIDs alone in achieving pain relief
Combination therapy with antispasmodics required more rescue analgesics
Evidence was weak
Indomethacin was found to be less effective than other NSAIDs
Limitations: pain recurrence reported by minority of studies, data on other major non-opioid medications was scarce
Systematic review and meta-analysis included 36 RCTs, >4800 patients, comparing the NSAIDs vs opioids vs paracetamol in pain reduction [2018]
Majority of studies (32) compared NSAIDs vs opioids
NSAIDs showed marginal benefits over opioids and no difference to paracetamol
RCT including >1600 patients, of whom >1300 had confirmed stones, comparing IM diclofenac vs IV morphine (0.1mg/kg) vs IV paracetamol (1g) [2016]
Both diclofenac and paracetamol were more effective at pain control when compared with morphine
No reported dialysis, death, hospitalizations, or GI bleeds
Limitations: single center study including mostly young and healthy males
Summary of NSAIDs:
NSAIDs are at least as effective, if not more effective, when compared to opioids
They remain the superior non-opioid agent
They do not appear to require the level of rescue analgesia as opioids and other non-opioids medications do
They are an adequate first line option
Opiates
Mechanism of action: interaction with mu receptor as they are mimics of endogenous opioids
Adverse effects: hypotension and respiratory depression (long term use can lead to dependence and abuse)
RCT [n=130] comparing the combination of ketorolac (15mg IV) + morphine (5mg IV) vs ketorolac vs morphine for use in adult patients presenting with flank pain and at least a 5 on VAS scale [Safdar, 2006]
Exclusion: contraindications to NSAIDs/opioids, renal dysfunction, history of bleeding diathesis, history of drug abuse or on methadone
Combination was superior in pain reduction to each agent alone with no difference appreciated between each single agent
Combination required less rescue analgesia
RCT [n=300] comparing ketorolac (30mg IV) + morphine (0.1mg/kg IV) vs ketorolac vs morphine for use in patients presenting with a clinical diagnosis of renal colic with a VAS pain score of at least 5
Excluded: history of renal dysfunction, pregnancy or breastfeeding, history of GI bleeding, use of analgesia 6h prior to arrival
Combination was more effective at achieving pain reduction at 20min and 40min with less requirement for rescue analgesia
No pain relief difference between single agents with more side effects for morphine group
Retrospective analysis [n=962] comparing use of opioids before and after implementation of guidelines in the treatment of renal colic [2019]
1st line: NSAIDs, APA, IVF
2nd line: IV lidocaine
3rd line: opioid rescue
Post-guideline group had a decrease in opioid requirement in both the ED course and atw discharge, however had higher admission rates and higher 7d re-presentation rates
Limitations: many clinicians did not adhere to the guidelines, many patients were chronically on outpatient opiates
Summary of Opioids:
They remain a viable option if NSAIDs are contraindicated or pain is refractory
Literature suggests the combination with non-opioids is more effective and prevent the need for rescue analgesia
The combination may mitigate adverse effects
Operations may play a role in future opioid mitigation
IV Acetaminophen
Mechanism of action: weak COX-1 inhibitor; onset within 5-10mins, peak effect at ~60mins
Systematic review included 5 RCTs comparing IV acetaminophen vs diclofenac, morphine, or piroxicam for renal colic [Sin, 2016]
APAP was slightly more effective at treating pain than morphine and equivalent to NSAIDs; APAP required less rescue analgesia, however no specific requirement reported for rescue analgesia need
Limitations: no definitive criteria as to when rescue analgesia is required, ambiguous study protocols, small sample sizes
Summary of IV APAP:
May be more effective than opioids
Weak evidence limits its utility
Cost remains a significant barrier
Requires further evaluation, especially in patient populations in whom NSAIDs and opioids are contraindicated
Ketamine
Mechanism of action: noncompetitive NMDA receptor antagonist with possible stimulation of mu receptors to enhance effects of opioids
Adverse effects: dissociative effect
RCT [n=106] comparing combination of morphine (0.1mg/kg) + ketamine (0.15mg/kg) vs morphine alone in renal colic [Abbasi, 2017]
Exclusion: history of liver or kidney disease, chronic respiratory disorders, cardiovascular disorders, blood clots, use of psych meds
Pain reduction at 10, 30, 60, 90, and 120min was the same
Morphine alone group required more rescue analgesia
Morphine alone group had more nausea/vomiting, respiratory depression, and hypotension
RCT [n=40] comparing intranasal ketamine (1mg/kg) vs IV morphine (0.1mg/kg) in renal colic
Exclusion: opiate use, hemodynamic instability, altered level of consciousness
Outcome: patient reduction in VAS scale
Morphine had improved pain scores at 5min, however no difference between the groups at 15 or 30min
Summary of IV APAP:
There are limited studies with strict inclusion criteria
Its role may be primarily as a combination with morphine to limit it’s required dosage, requirement of rescue analgesia, and side effects
IN route of administration may eventually serve a bigger role
Needs further research overall
Lidocaine
Mechanism of action: voltage dependent sodium channel blocking agent , G protein coupled receptors and NMDA receptors
Systematic review included 8 studies evaluating the efficacy of lidocaine compared to other agents in pain reduction for patients presenting with various conditions [Oliveira, 2018]
Limited evidence for its role in acute renal pain
Limitations: variation in dosing (some weight-based doses, some fixed-doses)
RCT [n=240] comparing IV lidocaine (1.5mg/kg) to IV morphine (0.1mg/kg) for the treatment of renal colic
Lidocaine provided significant more relief than morphine based on VAS pain score at all time points measured
Summary of lidocaine:
Weak evidence for its use and limited evidence studying the safety profile as an analgesic in the ED
Magnesium
Mechanism of action: acts as a smooth muscle relaxer and antagonist of NMDA receptors that may lead to blockage of neurotransmission of pain
Adverse effects: hypotension, nausea/vomiting, facial flushing, retention of urine, depression, lethargy
Systematic review included 4 RCTs comparing magnesium (varying doses) to morphine (0.1mg/kg), ketorolac (30mg), and placebo [2020]
Morphine and ketorolac were superior to mag
Limitations: heterogeneity in studies
Summary of magnesium:
Very limited role, requires further research
Tamsulosin
Cochrane review included 67 RCTs, >10,000 patients included, looking at the use of alpha blockers as medical expulsive therapy for ureteral stones [2018]
Alpha blockers resulted in a shorter time to stone passage of about 3.7d, fewer episodes of pain, and lower risks of both surgical intervention and hospital admissions
Findings were independent of stone location
Systematic review and meta-analysis of 55 RCTs evaluating the effectiveness of alpha blockers vs standard therapy
No benefit to treatment with alpha blocker in smaller ureteric stones
Demonstrated the above findings
R2 CPC WITH DRS. BROADSTOCK & LANG
Female in her 60s with PMH ADHD, HTN, kidney stones, peripheral neuropathy who presents with 1 month of “feeling off.” She’s felt weak, not like her normal self mentally, and has had a 15lb weight loss. She’s also had swelling in her legs and a sore throat. She suffered a fall yesterday and now has pain in her left shoulder and knee. Intermittent throbbing headaches, memory loss, tired, short of breath with ambulation, diarrhea.
Medications: lisinopril-HCTZ, diltiazem, hydroxyzine, analgesics for chronic back pain
Exam: A&Ox3. Fine tremor of bilateral hands, requires assistance with ambulation, ⅘ strength to bilateral lower extremities. Dry mucous membranes. Tachycardic and regular heart rate with clear lungs. 2+ pitting edema to the bilateral lower extremities. Atraumatic left shoulder and left knee.
Labs: K 2.8, WBC 10.9, alk phos 286, troponin 26, BNP 744, UA WBC 13
CXR, XR L shoulder and L knee: unremarkable
EKG: sinus tachycardia, prolonged QTc 550ms, nonspecific TWI
CT head non-con: unremarkable
...and then a test was ordered…
[Interlude]
Type 1 thinking: Fast, easy, automatic, unconscious, relies on experience, pattern recognition, prone to bias
Type 2 thinking: Slow, difficult, effortful, conscious, relies on knowledge, logical, overcome bias
TSH, T4: Thyroid Storm
Incidence: 2 per 1,000,000 persons per year in the US
16% of thyrotoxicosis cases progress to thyroid storm
Mortality rates are 10-30%
This is a clinical diagnosis, however difficult to make in real time. Scoring systems have been created to help determine who may be at risk:
Burch-Wartofsky Point scale: Temperature, CNS dysfunction, GI symptoms, HR, CHF, Afib, precipitating event
No external validation and it is non-specific
Japanese Thyroid Association Score
Labs (fT4 or fT3) +
CNS manifestations: fever, tachycardia, congestive heart failure, GI
Thyroid storm = CNS + 1 other OR ¾ non-CNS sx → mortality of 11%
Suspected = 2/4 non-CNS sx → mortality of 9%
Most common symptoms in patients >50yo: tachycardia, fatigue, anorexia, weight loss...in lieu of psychomotor agitation most commonly associated with thyroid storm in younger patients
Management:
Beta blocker (can use calcium channel blockers if contraindication to BB...won’t get the additional benefit preventing peripheral conversion from T4 → T3)
Assists with tachycardia, HTN
Decreases peripheral conversion of T4 to T4
Anti-thyroid medication
Methimazole or PTU - PTU in pregnancy!
Steroids
Decreases conversion of T4 to T3 and decrease antibodies against the thyroid in Graves’ disease
Iodine supplementation
Decreases the synthesis of thyroid hormone
Administer 60min after the anti-thyroid medication
Cholestyramine
Decrease enterohepatic circulation of thyroid hormone and leads to excretion
Case reports on use of plasma exchange to remove excess hormone
CONSIDER
Ultrasound to assess low output v high output heart failure
Administration of furosemide can lead to uncoupling of thyroid hormone from its carrier protein which can further exacerbate thyroid storm if unintentionally mistreating as acute congestive heart failure
Treat fevers preferably with tylenol. NSAIDs will dislodge T4 from its protein binding making it available for conversion to T3. Can passively externally cool if needed, avoid active cooling as it will worsen vasoconstriction in an already hyperadrenergic state that will exacerbate hypertension and thyroid storm
Hyperthyroidism increases risk of thromboembolic events by 1.4X. Consider anticoagulation.
The patient received propranolol and steroids in the ED and methimazole after admission. Thyroglobulin antibodies were positive, indicating a new diagnosis of Graves disease. She was discharged with metoprolol and methimazole on HD3 and is overall doing well on outpatient follow up visits.